How Do You Choke? Let Me Count the Ways…
Four examples of how the term “choking” can mean different things
First example
When asked the reason he was calling for an appointment, a middle-aged man offered that he was “choking.” Staff not unreasonably marked on his chart that swallowing was his primary issue. In the first minutes of our time together, he focused my attention on “choking caused by swallowing.”
But it shortly became clear that his choking was not “something going down the wrong pipe.” In fact, he had undergone prior xray evaluation of his swallowing function, and passed with flying colors. Rather, as he explained to me, a routine swallow would occasionally trigger a tickling sensation that set off a paroxysm of violent coughing.
Bottom line? He was experiencing sensory neuropathic cough but with swallowing, especially of acidic or “scratchy” foods as one of his most prominent triggers.. He had used the word “choking” because the coughing was so intense and prolonged that he could only think of that word to describe the episode.
Resolution
He was given the explanation he needed about sensory neuropathic cough and we began our search for best medication with low-dose amitriptyline…
Second Example
Another “choking” patient was also initially designated as having a swallowing problem, but in his view, he ate and drank normally. During a bad cold 2 months earlier, he had initially “coughed his head off.” Although the cough had mostly subsided, he had started to awaken at night “choking,” and unable to breathe. He had endured 4 such frightening episodes across the past two months or so, thankfully with none in the past 3 weeks. Despite the recent quiescence, he was terrified it would happen again.
If a drip of saliva, or an upsurge of stomach acid had been the entire explanation, he would be expected to have simply awakened coughing. But his episodes had been much more than that — his laryngeal closure reflex was triggered, and the result was much more dramatic than coughing. He made loud inspiratory breathing noise for what seemed like an eternity but was actually about a minute. In fact, his events have a name: laryngospasm.
Resolution
He was given a clear explanation of laryngospasm, an introduction to straw breathing, a suggestion that he take an acid-reducing medication for a month, and departed much relieved.
Third Example
A third patient, an elderly person, gave “choking” as the reason for the visit, and the chart was so labeled. In this case it was swallowing at issue. This person had been taking longer to eat and was having to chew extra carefully. He had abandoned eating meat, gummy bread, and even mashed potatoes. His diet had become mostly soft foods, puree consistency, and liquids, because solid foods and some larger pills were getting stuck low in his throat regularly.
The sensation was very uncomfortable and made him fear his airway would be blocked. A few times, he had tried to sip liquids to clear the sense of blockage, but the liquid wouldn’t pass and instead came out his nose. A videofluoroscopic swallow study confirmed that his trouble really was a disorder of the upper esophageal sphincter called cricopharyngeus dysfunction.
Resolution
Initial swallowing therapy to work on ways to reduce the problem behaviorally through food choices and extra care in chewing, and also the offer of cricopharyngeus myotomy.
Fourth Example
Yet a fourth patient, also elderly, described “choking” as the primary issue. Swallowing was also truly the problem here, too, except that it was happening mostly with liquids. Soft solids, and puree consistency worked quite well. A videofluoroscopic swallow study here showed good opening of the upper esophageal sphincter, but a pronounced tendency to pool some swallowed material in the throat after swallowing. When liquids were consumed, some tended to go into the airway—“down the wrong tube”—to cause coughing.
Resolution
Swallowing strategies, thickening liquids to slow them down, and taking liquids as sips were recommended.
Conclusion
Patients and their doctors can work efficiently to an understanding of “choking” when the four common uses of the word are kept in mind, as described above, and summarized below.
1. I am choking. By that I mean that swallowing, (or a loud laugh, or breathing in cold air, or….) causes an abrupt tickling sensation which in turn initiates a violent attack of coughing. (Sensory neuropathic cough)
2. I am choking. By that I mean that suddenly, my throat seems to close; I can’t breathe, and I begin making loud noises when I try to breathe in. It is terrifying but seems to be over within a minute or two. (Laryngospasm)
3. I am choking. By that I mean that when I swallow, solid food and pills tend to get stuck in my throat <point to where> and sometimes I gag and try to spit to get it up. (Cricopharyngeus dysfunction with or without Zenker’s Diverticulum)
4. I am choking. By that I mean that when I swallow liquids in particular, it wants to go down the wrong tube and it makes me cough. (Aspiration)
Share this article
Coughing That Won’t Go Away (SNC) – Part 1
Sensory neuropathic cough is a chronic cough condition that does not respond to the usual treatments. Many individuals who have been coughing for years find relief from treatment with “neuralgia” medications.
Laryngospasm: Sudden, Terrifying Difficulty Breathing
Dr. Robert Bastian of Bastian Voice Institute explains laryngospasm with video of the larynx and a simulated attack.
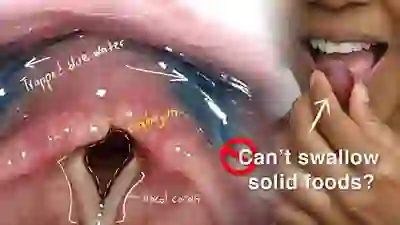
Cricopharyngeal Dysfunction: Difficulty Swallowing, Especially Solid Foods
Dr. Bastian explains this progressive swallowing problem and presents options for treatment. Cricopharyngeal dysfunction is caused by failure of relaxation of the upper esophageal sphincter—cricopharyngeus muscle—during eating.
Typically it is solid foods that tend to lodge in the mid-neck area where this muscle is located.
Swallowing Trouble 101
This video gives an overview of how swallowing works, how it can sometimes go wrong (presbyphagia or cricopharyngeal dysfunction), and possible ways to treat those problems (swallowing therapy or cricopharyngeal myotomy).