Recurrent Respiratory Papillomatosis (RRP) and Other HPV-Induced Lesions
RRP is a disorder in which wart-like tumors or other lesions grow recurrently within a person’s airway. These growths are caused by the human papillomavirus (HPV), and they may occur anywhere in a person’s airway, such as on the vocal cords (by far the most common site), in the supraglottic larynx, or in the trachea. If these growths are removed, they will almost always grow back, or recur; hence, “recurrent respiratory papillomatosis.”
Symptoms and risks of recurrent respiratory papillomatosis
RRP can be life-threatening in young children, if not carefully followed and treated, since a child’s airway is relatively narrow and can potentially be obstructed completely by the disease’s proliferative growths; moreover, RRP in children tends to grow and recur more aggressively.
In adults, RRP will usually only impair voice function (when the growths occur on the vocal cords), though it can also impair breathing in severe cases. Occasionally, RRP can also progress to cancer, and therefore patients found to be at high risk for this (see below) need to be monitored carefully.
Characteristics of RRP growths
The growths usually associated with RRP are wart-like tumors, or papillomas, that protrude conspicuously from the surface on which they grow, often in grape-like clusters. These kinds of papillomas are usually seen in patients who have HPV subtypes 6 or 11, which are both lower-risk subtypes for incurring cancer.
There are some HPV patients, however, who manifest their HPV infection with subtler, velvety growths within the airway—“carpet-variant” growths, so to speak. Although these “carpet-variant” growths do not have the wart-like appearance of the papillomas typically associated with RRP, there at least a few key points of similarity:
- Both the “carpet-variant” and wart-like growths are lesions that sometimes appear, either independently or together, in patients who have HPV;
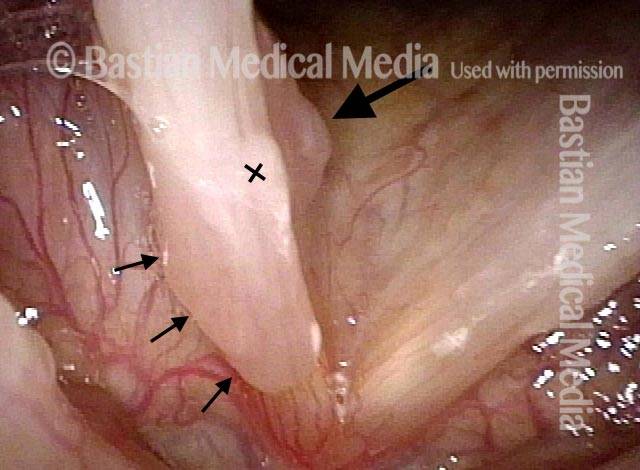
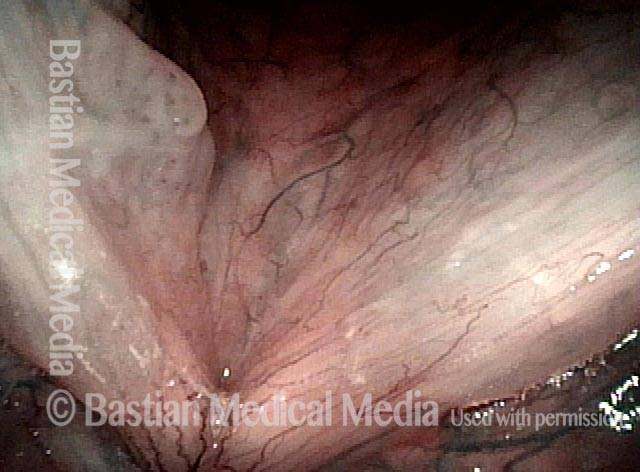
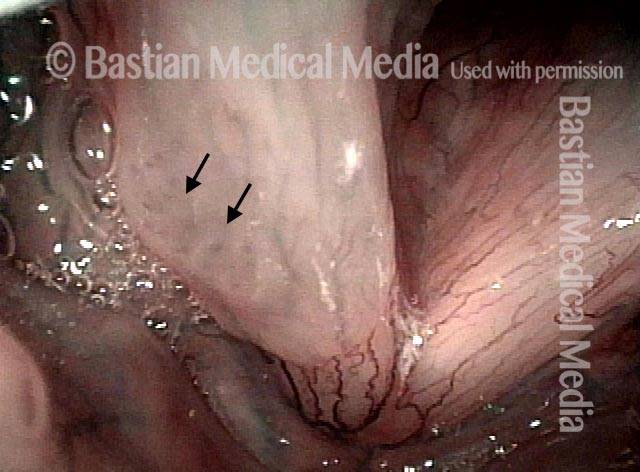
- Both the “carpet-variant” and wart-like growths are stippled with polka-dot vascular markings, because each “loop” in the “carpet” or each “grape” in the wart-like cluster has its own fibrovascular core, seen as a red dot;
- Both the “carpet-variant” and wart-like growths can disrupt voice function;
- Both the “carpet-variant” and wart-like growths usually recur if they are removed.
Because of these similarities, we consider these “carpet-variant” growths, even when the sole expression of the infection, to be at least a cousin to RRP, within the family of HPV-induced lesions. Many patients with this “carpet-variant” condition have HPV subtypes such as 16 or 18 that are higher-risk for cancer; such patients need to be monitored with particular care.
Treatment for recurrent respiratory papillomatosis
The primary treatment for RRP and other HPV-induced lesions is careful, conservative surgical removal of the growths. Because these growths almost always recur, surgery must usually be performed on a repeated basis, as frequently as every few weeks in children, but on average much less often in adults.
A common interval between surgeries for adult patients is between every six months and every two years, depending on how quickly the RRP or other HPV-related lesion recurs and impairs the patient’s voice function again.
There are also a few medical treatments that have been used in addition to surgery, including, among others, interferon, indole-3-carbinol, intralesional mumps or MMR (measles-mumps-rubella) vaccine, cidofovir, and bevacizumab.
Humility Before the HPV Virus—A Recurrence of Papillomas at Ten Years
HPV infection is considered chronic, and causes recurrent growth of papillomas in the larynx. Still, we sometimes see what appear to be cures, or at least long-term remissions. That appears to be the case here.
After an 8 year interval of perfect voice, the patient had a sudden increase of hoarseness occurring in the few weeks prior to the last examination below. This is an illustration of why we often say to a patient who appears to be cured, “You may be cured, but we usually say “long term remission.” This patient’s scenario is not rare.
Was her longterm, 8-year remission due to meticulous surgery? Cidofovir? Her immune response? It is impossible to say if it was one or all of these factors.
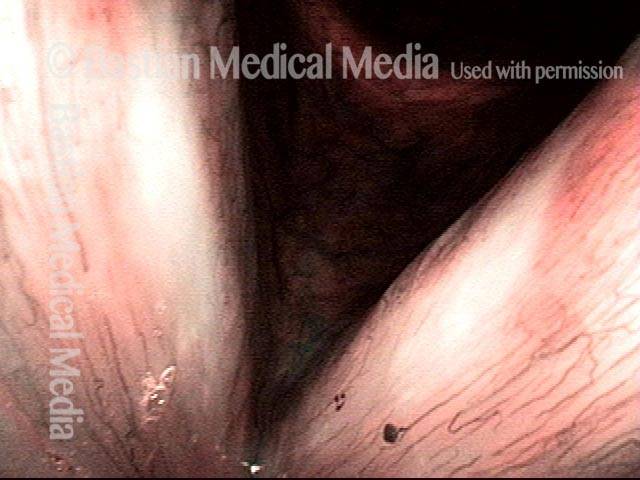
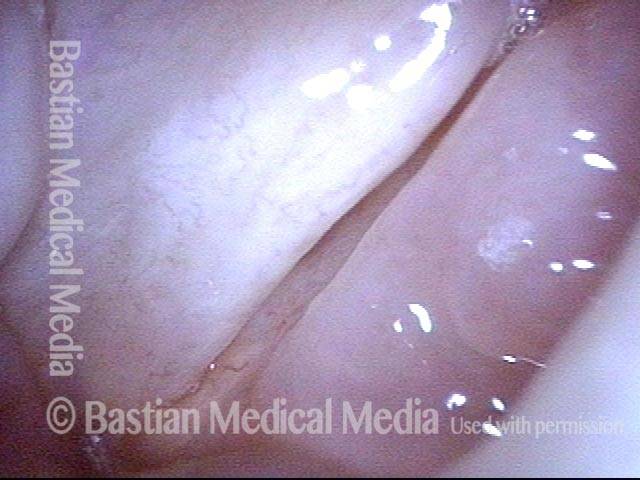
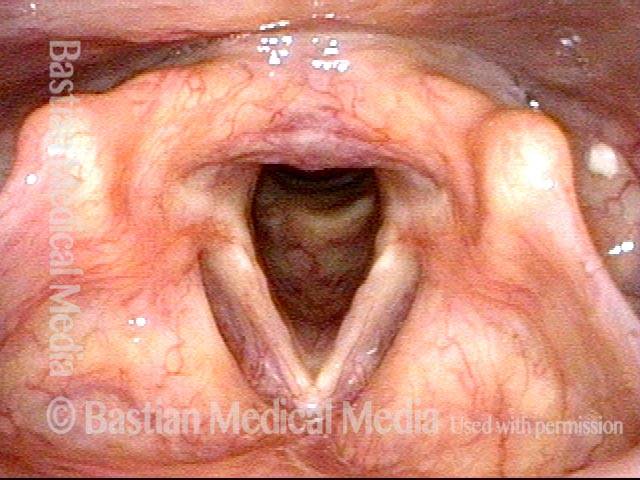
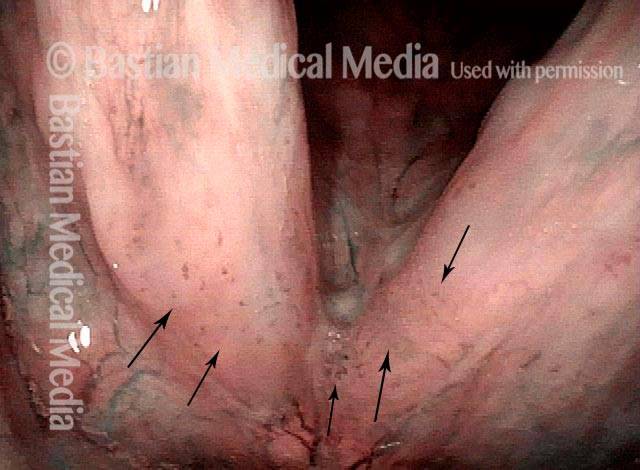
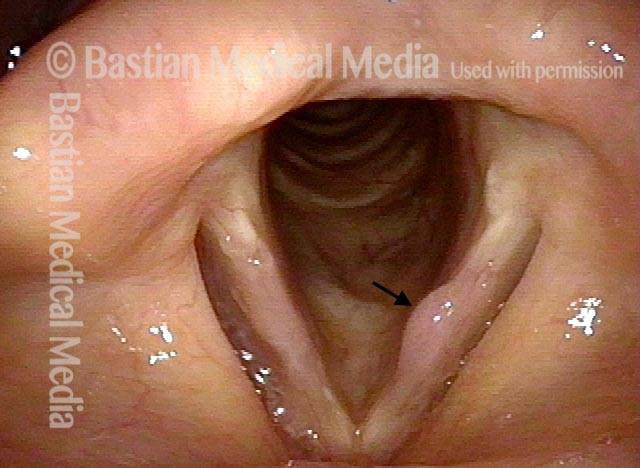
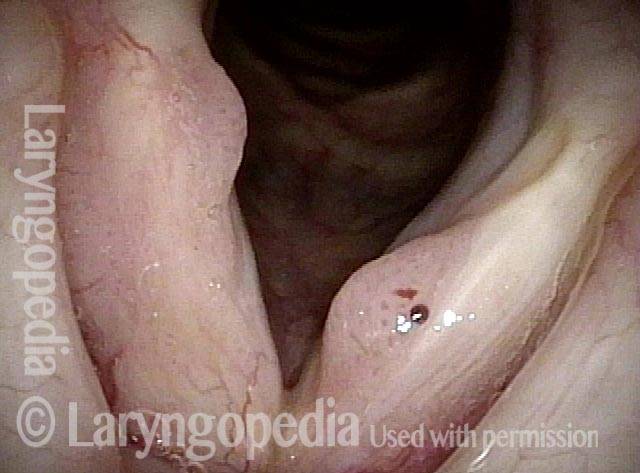
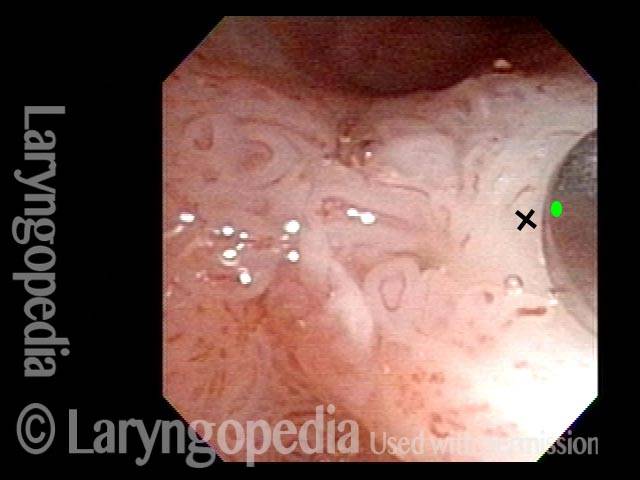
Stippled Vascularity (1 of 8)
Stippled Vascularity (1 of 8)
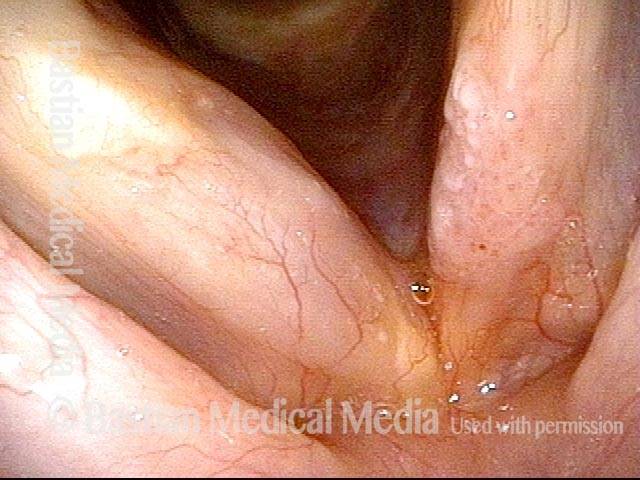
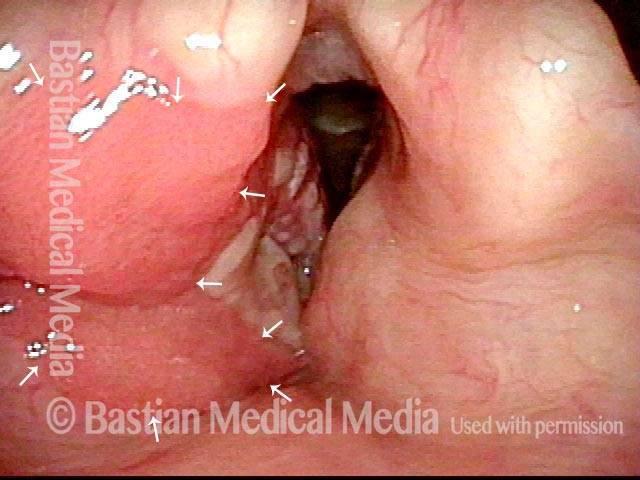
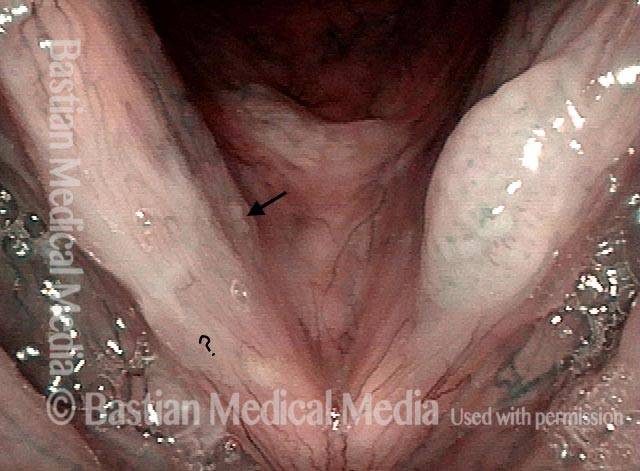
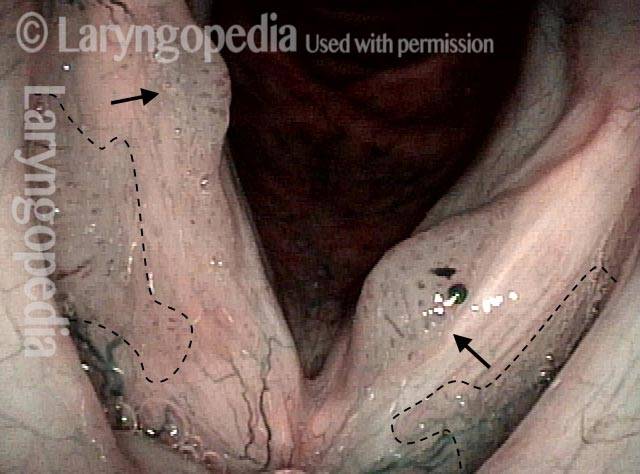
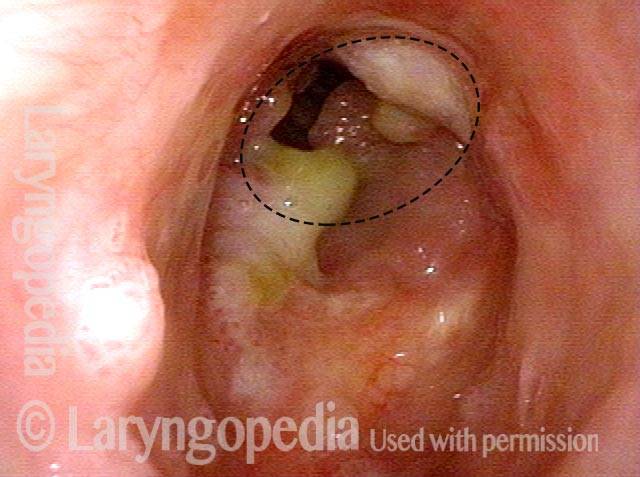
HPV infection (2 of 8)
HPV infection (2 of 8)
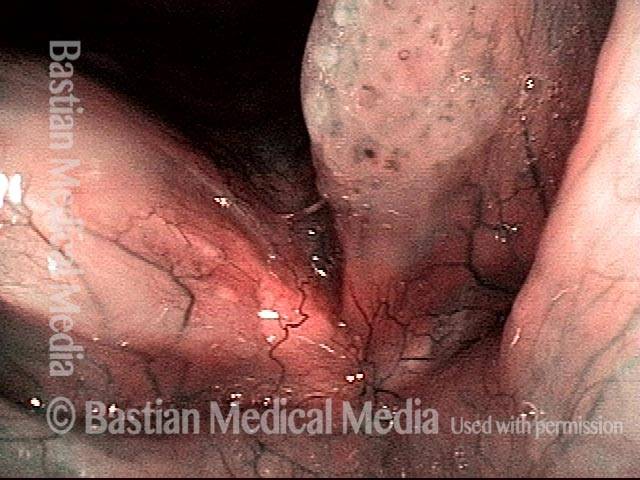
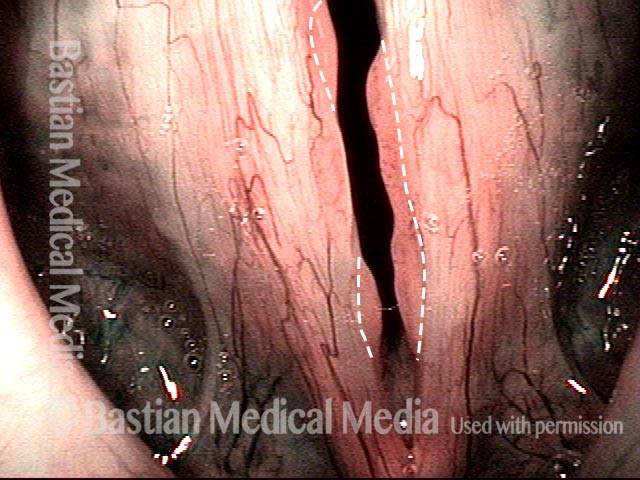
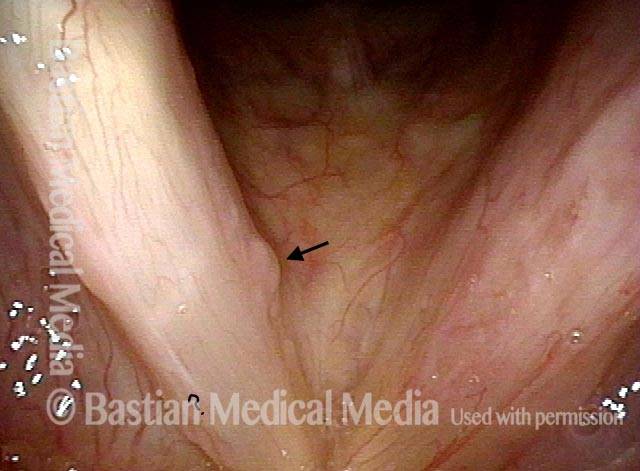
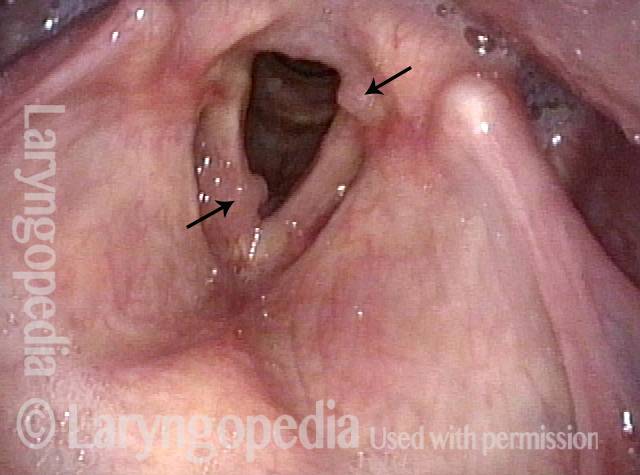
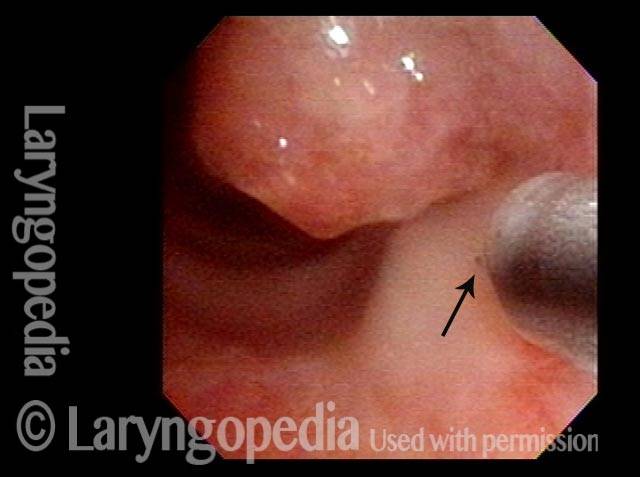
Stippled vascularity (3 of 8)
Stippled vascularity (3 of 8)
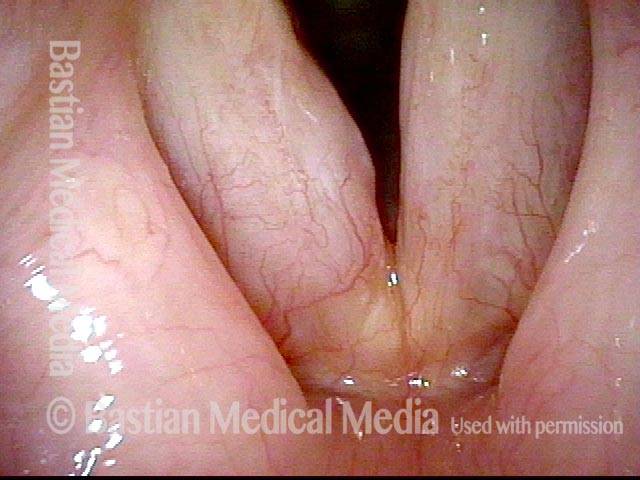
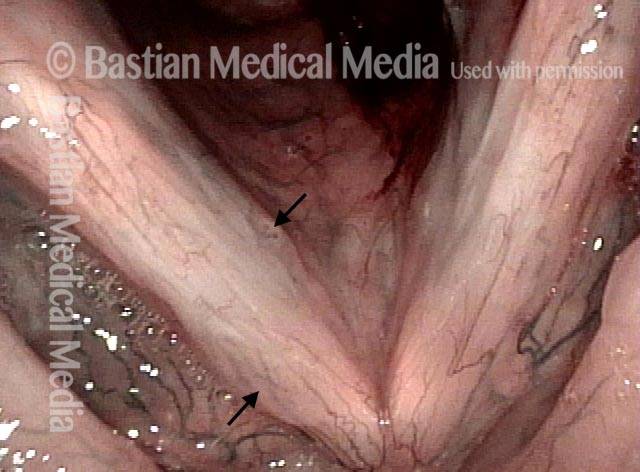
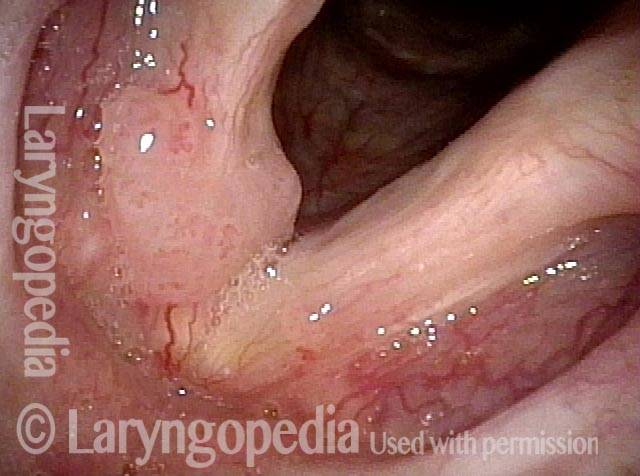
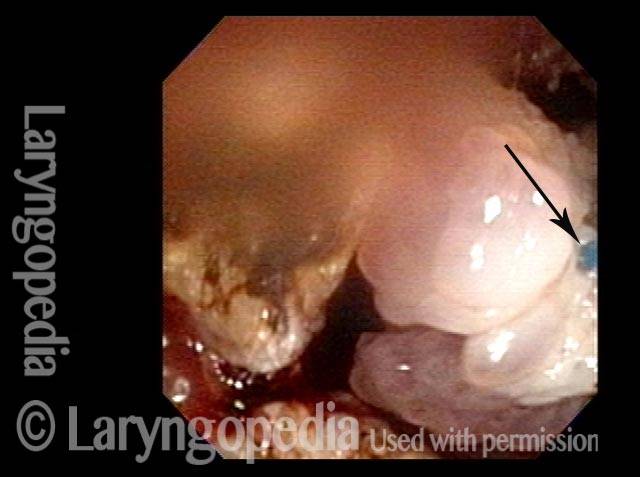
HPV vascular effect (4 of 8)
HPV vascular effect (4 of 8)
16 months later (5 of 8)
16 months later (5 of 8)
Is it long-term remission? (6 of 8)
Is it long-term remission? (6 of 8)
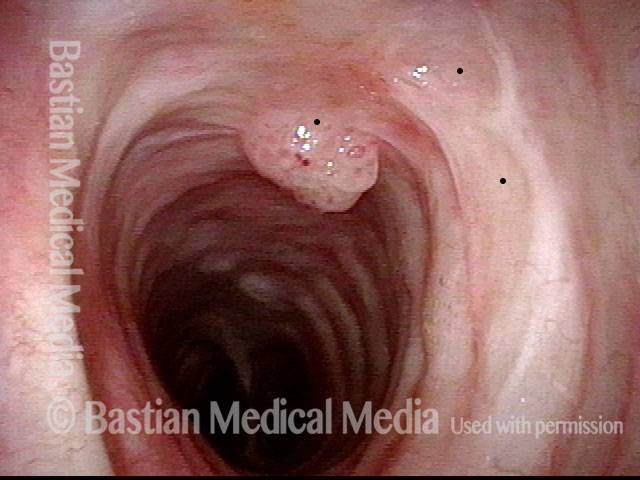
Recurrent Papilloma (7 of 8)
Recurrent Papilloma (7 of 8)
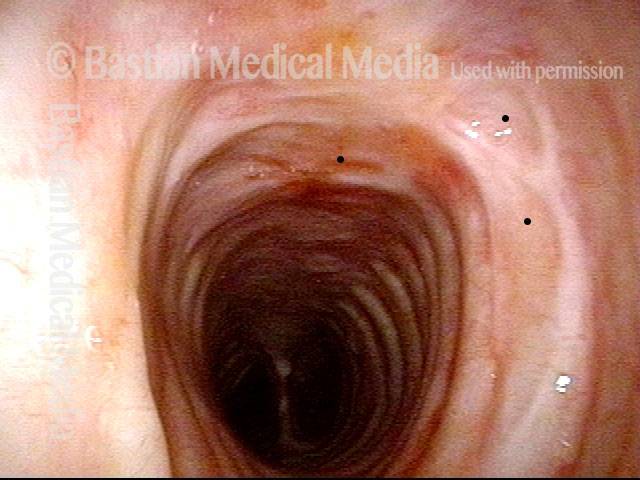
Stippled vascularity (8 of 8)
Stippled vascularity (8 of 8)
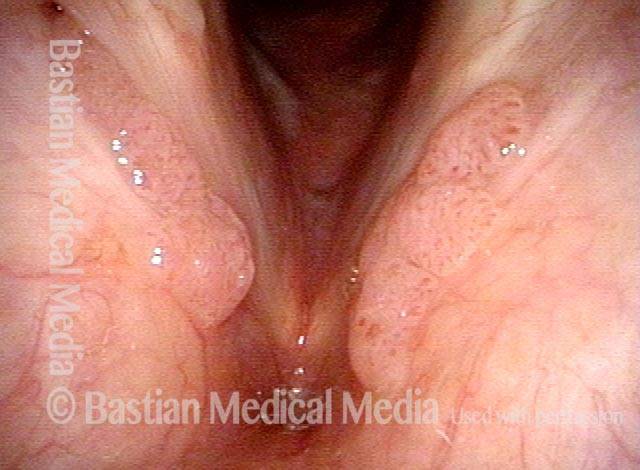
Papillomas, HPV Subtype 11, before and After Removal
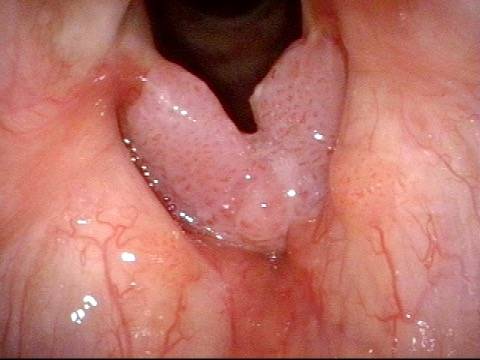
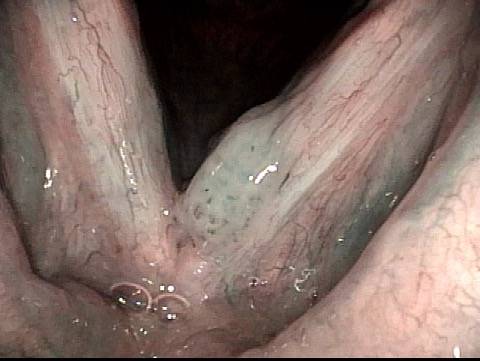
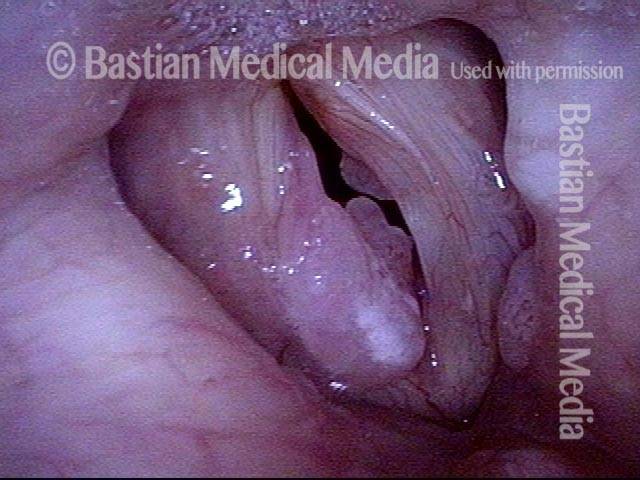
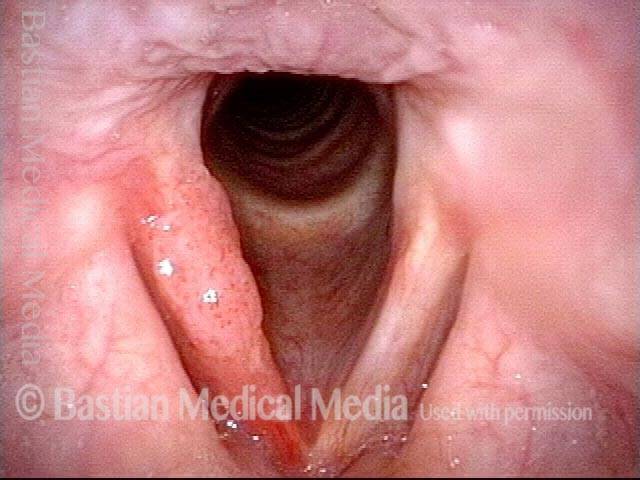
Papillomas: HPV Subtype 11 (1 of 4)
Papillomas: HPV Subtype 11 (1 of 4)
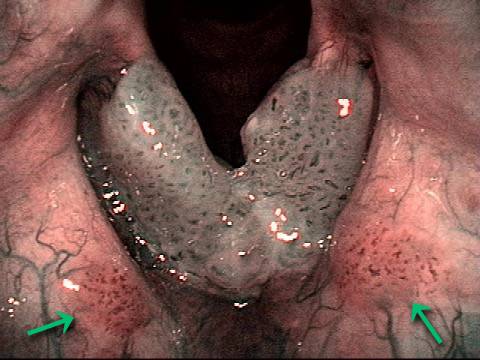
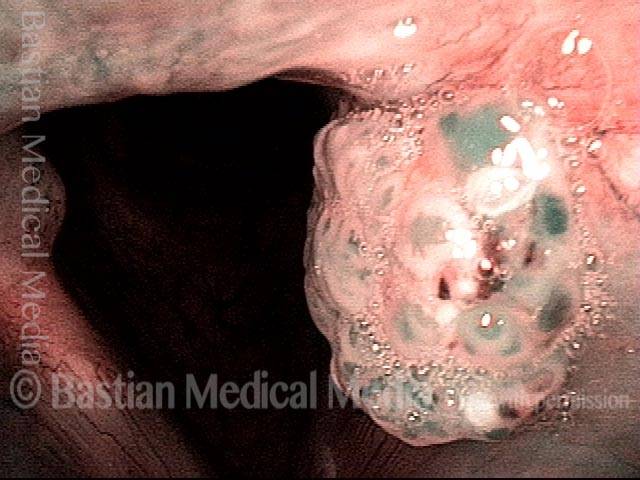
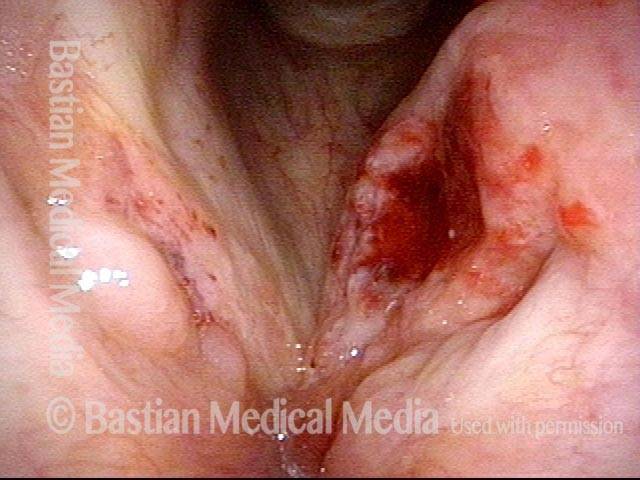
Papillomas: HPV Subtype 11 (2 of 4)
Papillomas: HPV Subtype 11 (2 of 4)
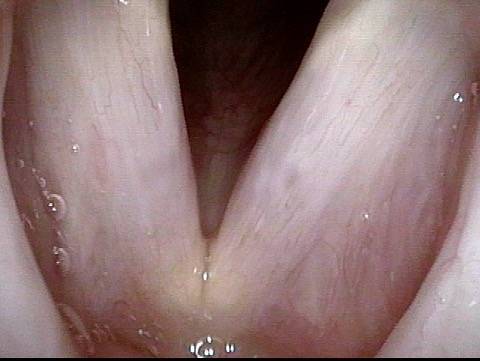
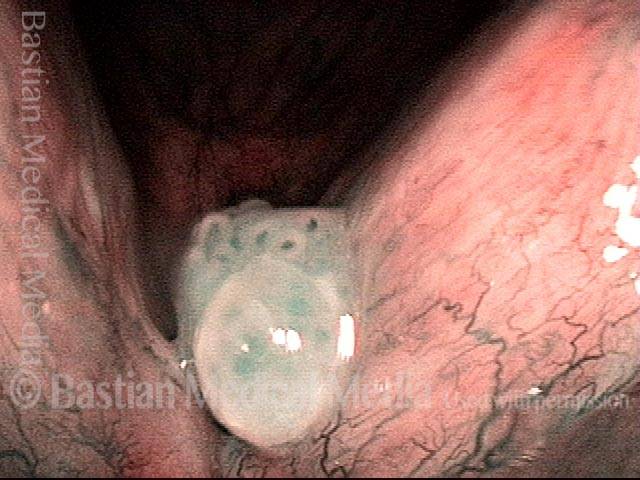
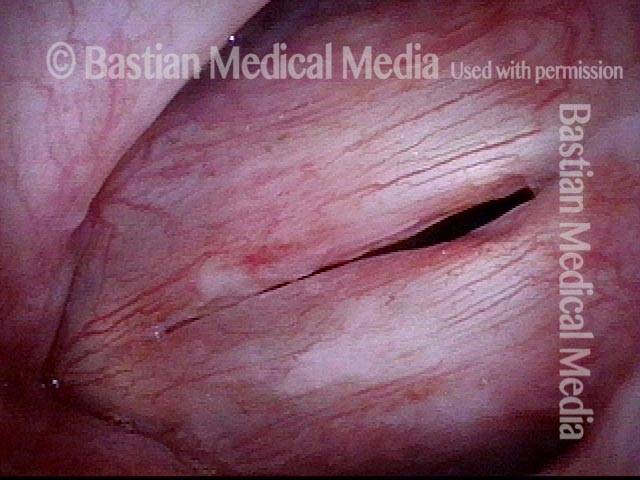
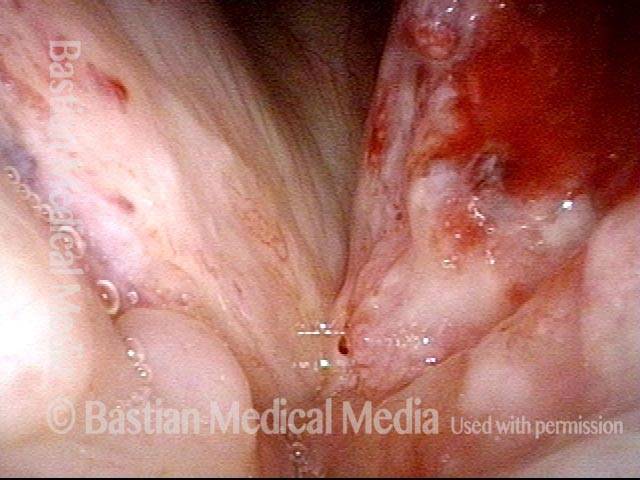
Papillomas, removed: HPV Subtype 11 (3 of 4)
Papillomas, removed: HPV Subtype 11 (3 of 4)
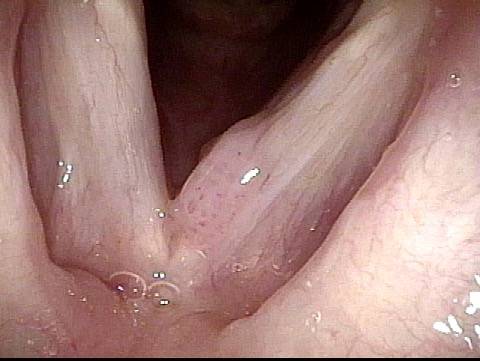
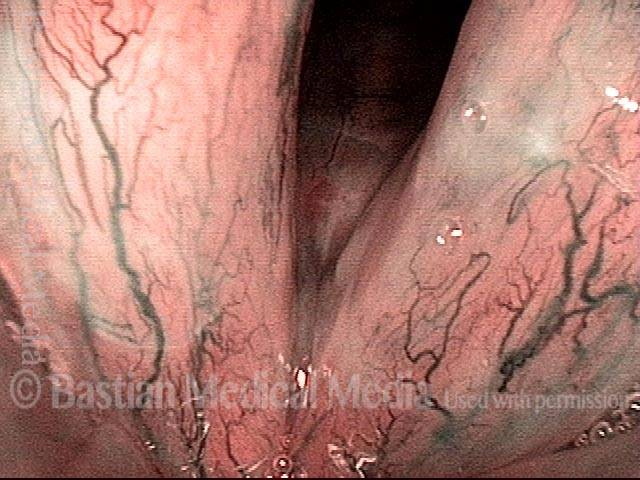
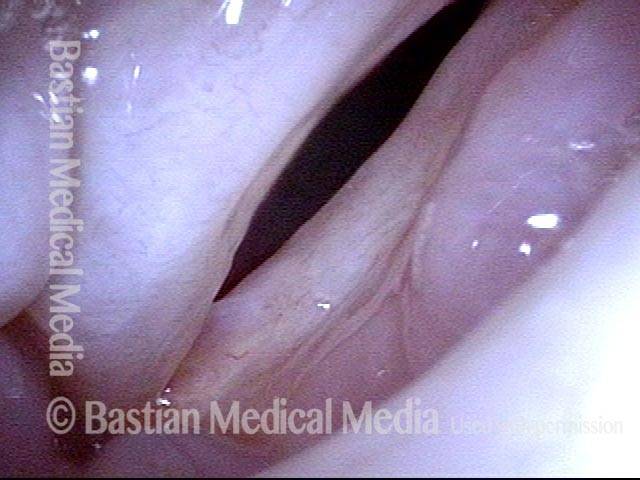
Papillomas, removed: HPV Subtype 11 (4 of 4)
Papillomas, removed: HPV Subtype 11 (4 of 4)
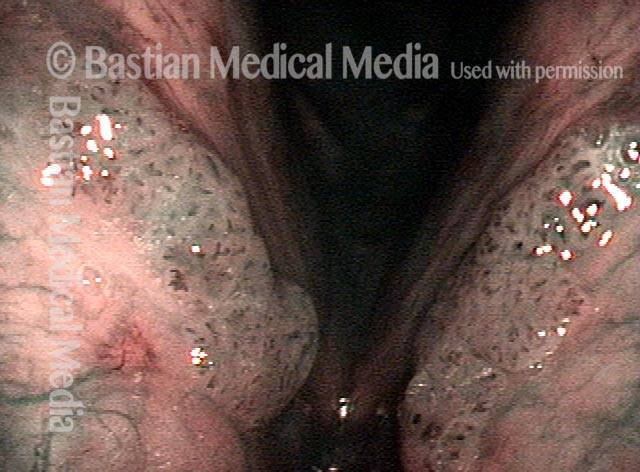
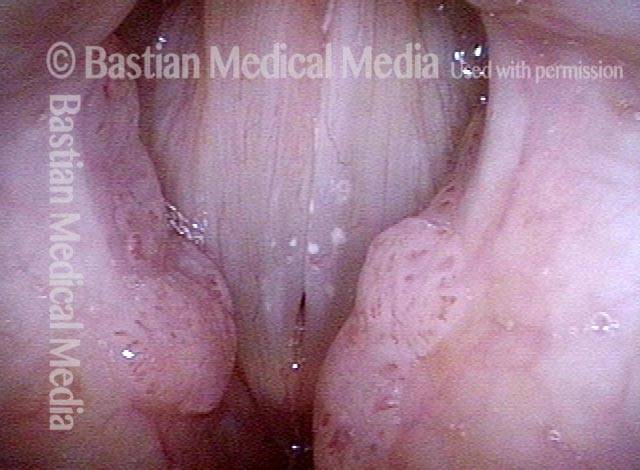
Papillomas, HPV Subtype 6, Before and after Removal
Papillomas: HPV Subtype 6 (1 of 4)
Papillomas: HPV Subtype 6 (1 of 4)
Papillomas: HPV Subtype 6 (2 of 4)
Papillomas: HPV Subtype 6 (2 of 4)
Papillomas, removed: HPV Subtype 6 (3 of 4)
Papillomas, removed: HPV Subtype 6 (3 of 4)
Papillomas, removed: HPV Subtype 6 (4 of 4)
Papillomas, removed: HPV Subtype 6 (4 of 4)
Papillomas, HPV Subtype 11
Papillomas: HPV Subtype 11 (1 of 3)
Papillomas: HPV Subtype 11 (1 of 3)
Papillomas: HPV Subtype 11 (2 of 3)
Papillomas: HPV Subtype 11 (2 of 3)
Papillomas: HPV Subtype 11 (3 of 3)
Papillomas: HPV Subtype 11 (3 of 3)
Example 2
Papillomas: HPV Subtype 11 (1 of 2)
Papillomas: HPV Subtype 11 (1 of 2)
Papillomas: HPV Subtype 11 (2 of 2)
Papillomas: HPV Subtype 11 (2 of 2)
HPV Lesions
Lesions of HPV Subtype? (1 of 2)
Lesions of HPV Subtype? (1 of 2)
Lesions of HPV Subtype? (2 of 2)
Lesions of HPV Subtype? (2 of 2)
Lesions and Papillomas of HPV, Before and After Removal and Adjuvant Injection
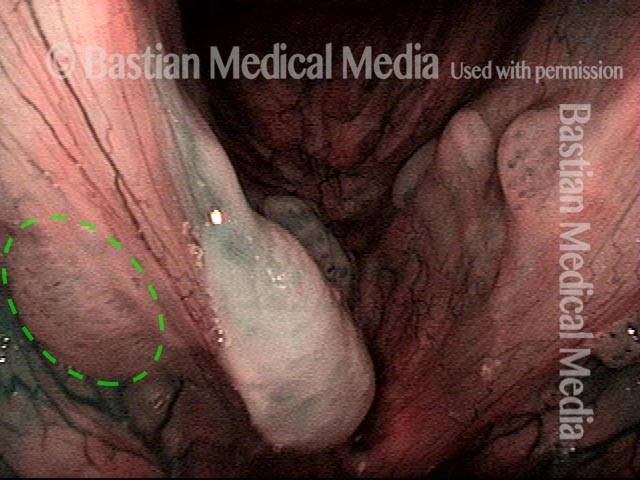
Lesions and papillomas of HPV subtype? (1 of 8)
Lesions and papillomas of HPV subtype? (1 of 8)
Subtle lesion (2 of 8)
Subtle lesion (2 of 8)
Open phase (3 of 8)
Open phase (3 of 8)
1 week after removal (4 of 8)
1 week after removal (4 of 8)
1 week after removal (5 of 8)
1 week after removal (5 of 8)
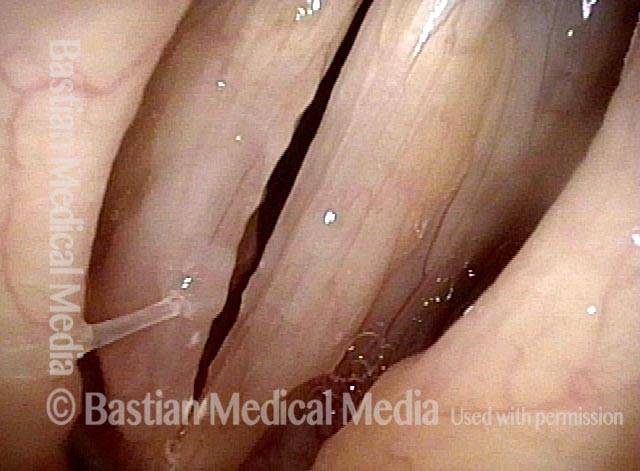
Injecting adjuvant (6 of 8)
Injecting adjuvant (6 of 8)
After injecting adjuvant (7 of 8)
After injecting adjuvant (7 of 8)
After final adjuvant injection (8 of 8)
After final adjuvant injection (8 of 8)
Papillomas, HPV Subtype 55, Going Into Remission
Papillomas: HPV Subtype 55 (1 of 4)
Papillomas: HPV Subtype 55 (1 of 4)
Papillomas: HPV Subtype 55 (2 of 4)
Papillomas: HPV Subtype 55 (2 of 4)
Papillomas, in remission: HPV Subtype 55 (3 of 4)
Papillomas, in remission: HPV Subtype 55 (3 of 4)
Papillomas, in remission: HPV Subtype 55 (4 of 4)
Papillomas, in remission: HPV Subtype 55 (4 of 4)
Papillomas, HPV Subtype 31, Going Into Remission
Papillomas: HPV Subtype 31 (1 of 4)
Papillomas: HPV Subtype 31 (1 of 4)
Papillomas: HPV Subtype 31 (2 of 4)
Papillomas: HPV Subtype 31 (2 of 4)
Papillomas, in remission: HPV Subtype 31 (3 of 4)
Papillomas, in remission: HPV Subtype 31 (3 of 4)
Papillomas, in remission: HPV Subtype 31 (4 of 4)
Papillomas, in remission: HPV Subtype 31 (4 of 4)
Papillomas, HPV
Papillomas: HPV Subtype? (1 of 2)
Papillomas: HPV Subtype? (1 of 2)
Papillomas: HPV Subtype (2 of 2)
Papillomas: HPV Subtype (2 of 2)
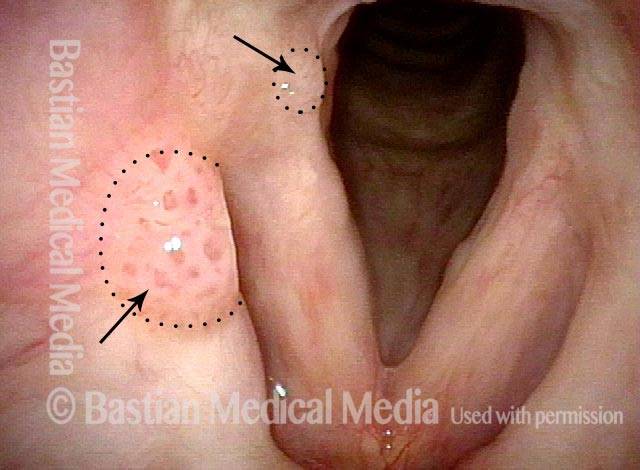
Pushing Past Red Herrings to Find the Real Issue
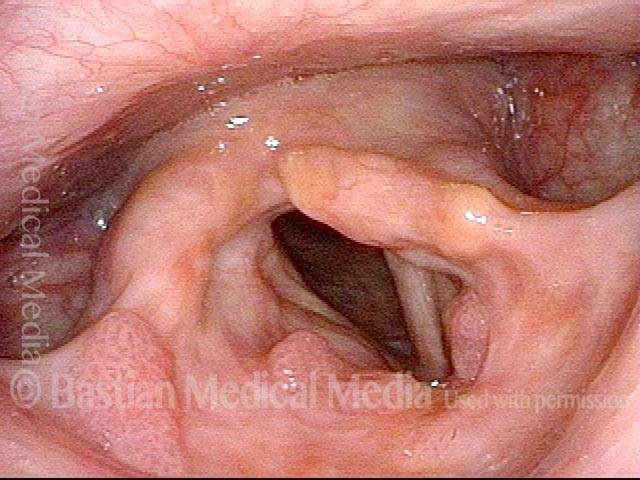
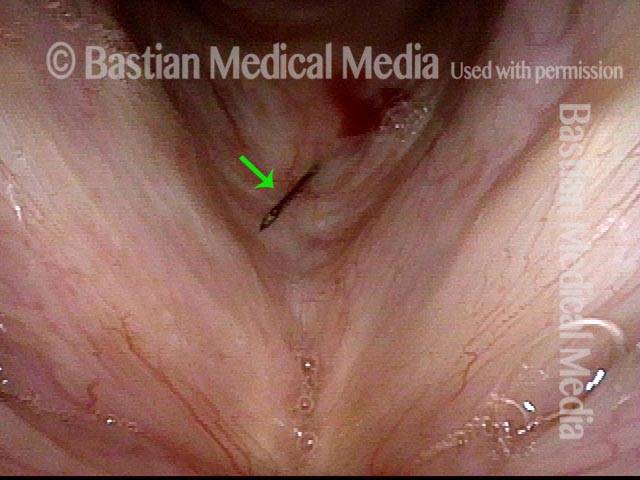
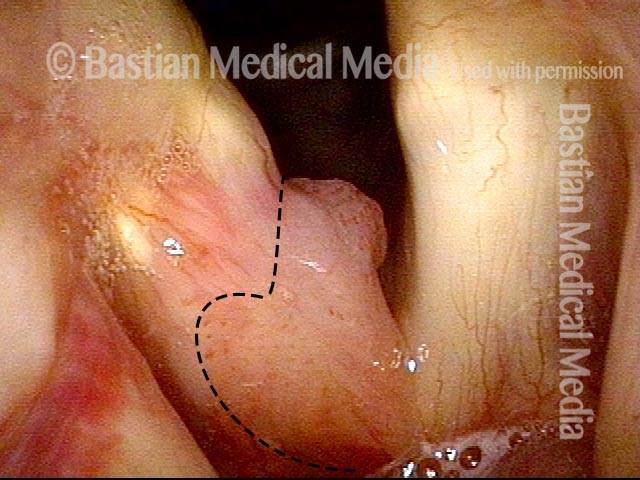
Obvious lesion not important (1 of 3)
Obvious lesion not important (1 of 3)
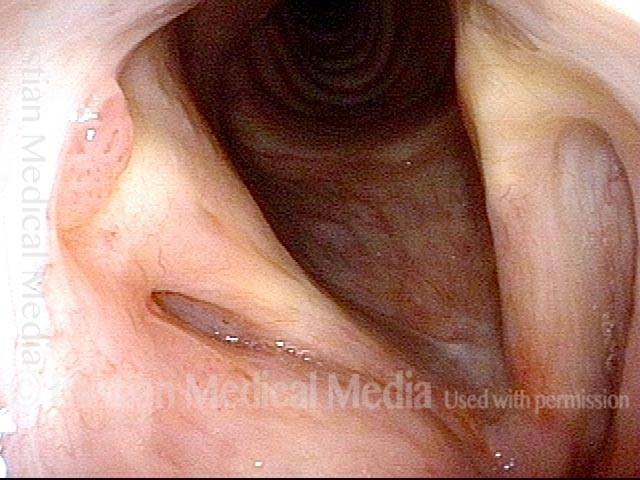
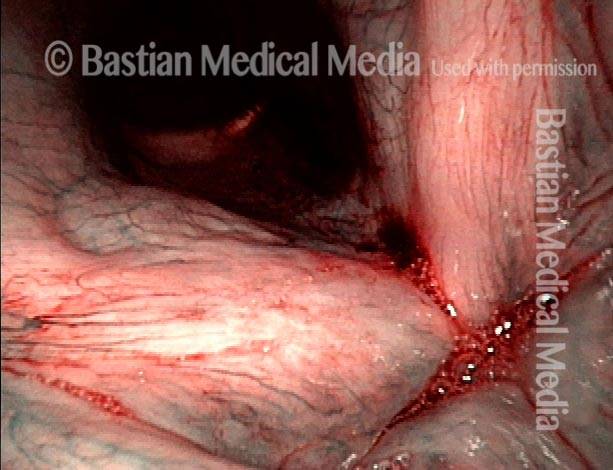
Granuloma (2 of 3)
Granuloma (2 of 3)
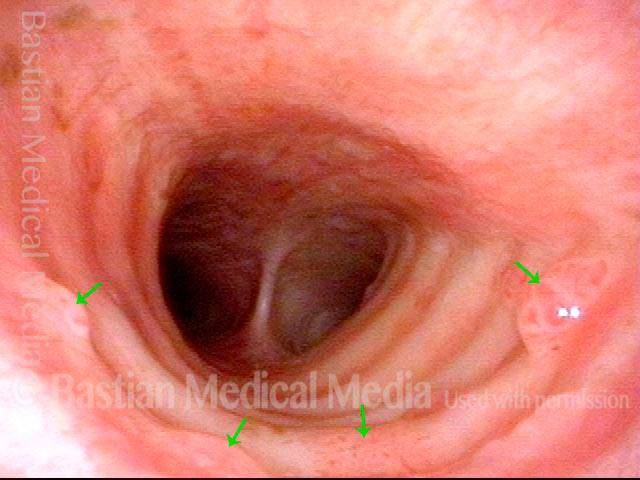
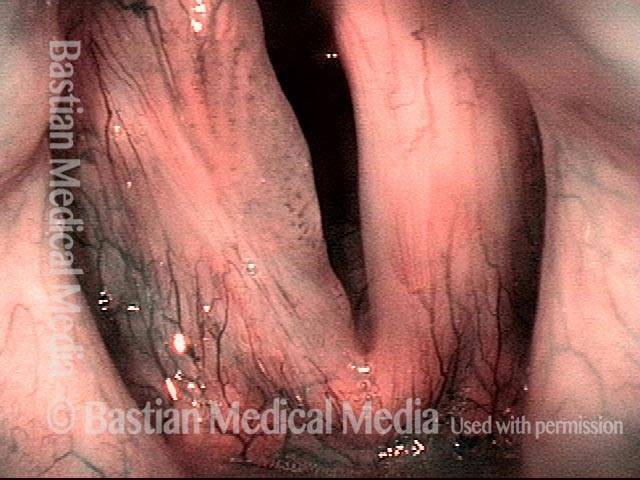
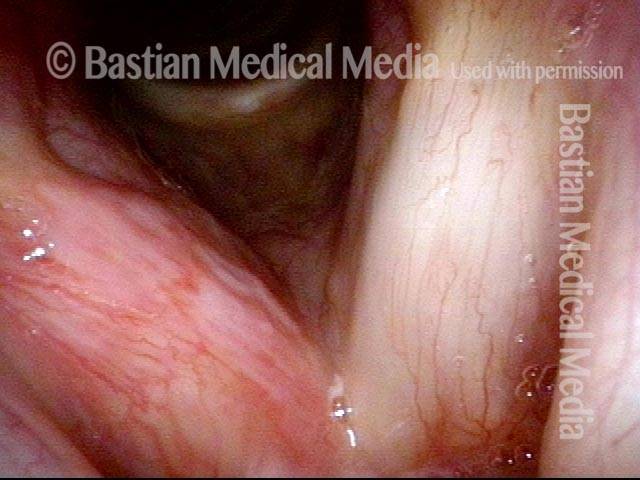
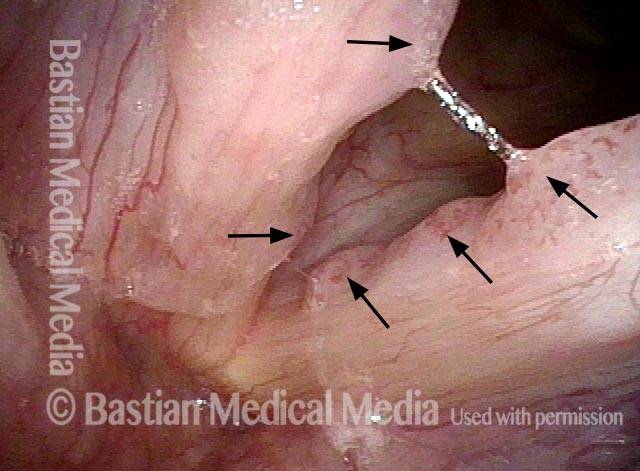
Carpet-varient papilloma (3 of 3)
Carpet-varient papilloma (3 of 3)
Papillomas, HPV Subtype 18 or 45
Papillomas: HPV Subtype 18 or 45 (1 of 2)
Papillomas: HPV Subtype 18 or 45 (1 of 2)
Papillomas: HPV Subtype 18 or 45 (2 of 2)
Papillomas: HPV Subtype 18 or 45 (2 of 2)
Lesions of HPV Subtype 16
Lesions of HPV Subtype 16 (1 of 3)
Lesions of HPV Subtype 16 (1 of 3)
Lesions of HPV Subtype 16 (2 of 3)
Lesions of HPV Subtype 16 (2 of 3)
Lesions of HPV Subtype 16 (3 of 3)
Lesions of HPV Subtype 16 (3 of 3)
Cancer, HPV Subtype 16, Before and After Radiation
Cancer: HPV Subtype 16 (1 of 5)
Cancer: HPV Subtype 16 (1 of 5)
Cancer: HPV Subtype 16, after radiation therapy (3 of 5)
Cancer: HPV Subtype 16, after radiation therapy (3 of 5)
Cancer: HPV Subtype 16, after radiation therapy (4 of 5)
Cancer: HPV Subtype 16, after radiation therapy (4 of 5)
Cancer: HPV Subtype 16, after radiation therapy (5 of 5)
Cancer: HPV Subtype 16, after radiation therapy (5 of 5)
Papillomas, HPV Subtype 45
Papillomas: HPV Subtype 45 (1 of 2)
Papillomas: HPV Subtype 45 (1 of 2)
Papillomas: HPV Subtype 45 (2 of 2)
Papillomas: HPV Subtype 45 (2 of 2)
Mid-Tracheal Papilloma, Treated By Thulium Laser
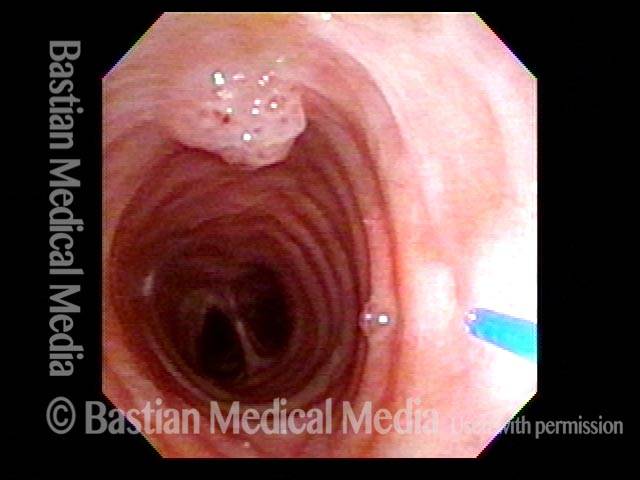
Mid-tracheal papilloma, being treated by thulium laser (1 of 5)
Mid-tracheal papilloma, being treated by thulium laser (1 of 5)
Months after treatment: no papilloma (5 of 5)
Months after treatment: no papilloma (5 of 5)
Mid-tracheal papilloma, being treated by thulium laser (2 of 5)
Mid-tracheal papilloma, being treated by thulium laser (2 of 5)
Mid-tracheal papilloma, being treated by thulium laser (3 of 5)
Mid-tracheal papilloma, being treated by thulium laser (3 of 5)
Mid-tracheal papilloma, being treated by thulium laser (4 of 5)
Mid-tracheal papilloma, being treated by thulium laser (4 of 5)
Subtle Papillomas, HPV Subtype 6
Subtle papillomas, HPV subtype 6 (1 of 3)
Subtle papillomas, HPV subtype 6 (1 of 3)
Subtle papillomas, HPV subtype 6 (2 of 3)
Subtle papillomas, HPV subtype 6 (2 of 3)
Subtle papillomas, HPV subtype 6 (3 of 3)
Subtle papillomas, HPV subtype 6 (3 of 3)
HPV Vascular Effect
Two papillomas (1 of 3)
Two papillomas (1 of 3)
Stippled vascularity (2 of 3)
Stippled vascularity (2 of 3)
HPV vascular effect (3 of 3)
HPV vascular effect (3 of 3)
Laryngeal Papillomas Rarely Can be Found by … Accident
Papilloma finding (1 of 4)
Papilloma finding (1 of 4)
Narrow band light (2 of 4)
Narrow band light (2 of 4)
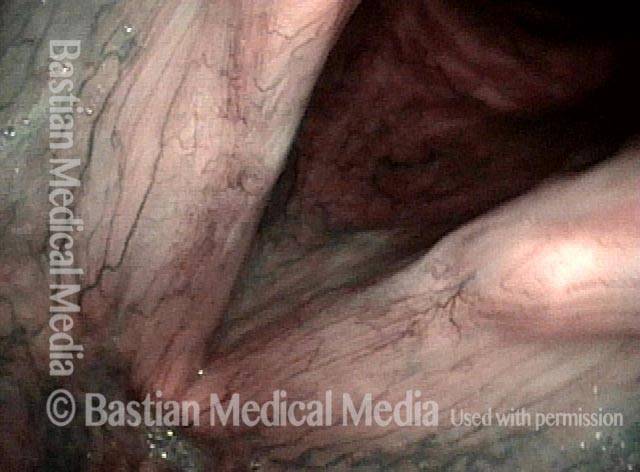
Closed phase (3 of 4)
Closed phase (3 of 4)
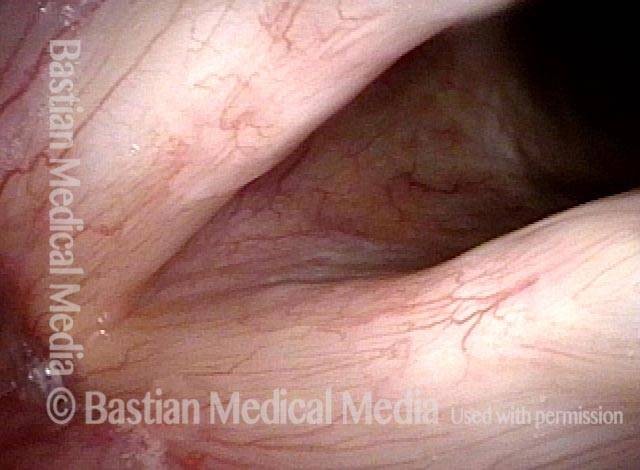
Open phase (4 of 4)
Open phase (4 of 4)
Winning Papilloma Battles, but not Winning the War….Yet
Left vocal cord lesion (1 of 8)
Left vocal cord lesion (1 of 8)
Narrow band light (2 of 8)
Narrow band light (2 of 8)
One week after removal (3 of 8)
One week after removal (3 of 8)
2 months after removal (4 of 8)
2 months after removal (4 of 8)
7 months after removal (5 of 8)
7 months after removal (5 of 8)
Papilloma and mucus (6 of 8)
Papilloma and mucus (6 of 8)
Stippled vascularity (7 of 8)
Stippled vascularity (7 of 8)
HPV disease (8 of 8)
HPV disease (8 of 8)
What “Cured” this Case of RRP? Surgery? Cidofovir? The Patient’s Immune System? All Three?
Papilloma (1 of 8)
Papilloma (1 of 8)
Stippling (2 of 8)
Stippling (2 of 8)
One week after surgical removal (3 of 8)
One week after surgical removal (3 of 8)
Cidofovir injection (4 of 8)
Cidofovir injection (4 of 8)
Six months after surgical removal (5 of 8)
Six months after surgical removal (5 of 8)
One week after second removal (6 of 8)
One week after second removal (6 of 8)
4 months later, healed (7 of 8)
4 months later, healed (7 of 8)
3 years later, no sign of papilloma (8 of 8)
3 years later, no sign of papilloma (8 of 8)
RRP Cure? Or Just Long Term Remission?
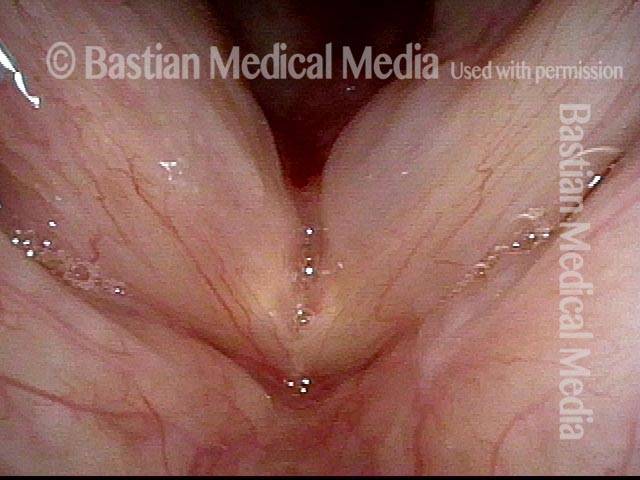
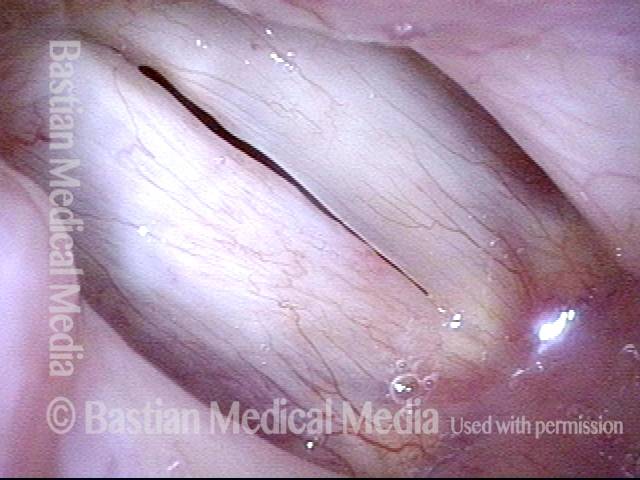
Chronic hoarseness (1 of 4)
Chronic hoarseness (1 of 4)
4 months later (2 of 4)
4 months later (2 of 4)
8 months from start of treatment (3 of 4)
8 months from start of treatment (3 of 4)
Narrow band lighting (4 of 4)
Narrow band lighting (4 of 4)
Polyps Need A Close Look: Here’s One Reason Why
“Polyps” diagnosis (1 of 4)
“Polyps” diagnosis (1 of 4)
Papillomas (2 of 4)
Papillomas (2 of 4)
Vascular stippling (3 of 4)
Vascular stippling (3 of 4)
Prephonatory instant (4 of 4)
Prephonatory instant (4 of 4)
Long-term Remission or even “cure” of RRP/Laryngeal Papilloma
Chronic hoarseness (1 of 6)
Chronic hoarseness (1 of 6)
Narrow band light (2 of 6)
Narrow band light (2 of 6)
Higher magnification (3 of 6)
Higher magnification (3 of 6)
Higher magnification, narrow band lighting (4 of 6)
Higher magnification, narrow band lighting (4 of 6)
Post-operation (5 of 6)
Post-operation (5 of 6)
Post-operation, narrow band lighting (6 of 6)
Post-operation, narrow band lighting (6 of 6)
Injected Local Anesthetic Causes Blanching
Infiltrating anesthetic (1 of 3)
Infiltrating anesthetic (1 of 3)
Blanching (2 of 3)
Blanching (2 of 3)
Subglottis being injected (3 of 3)
Subglottis being injected (3 of 3)
Local Rather than Topical Anesthesia can Permit Fairly Major Tracheal Surgery
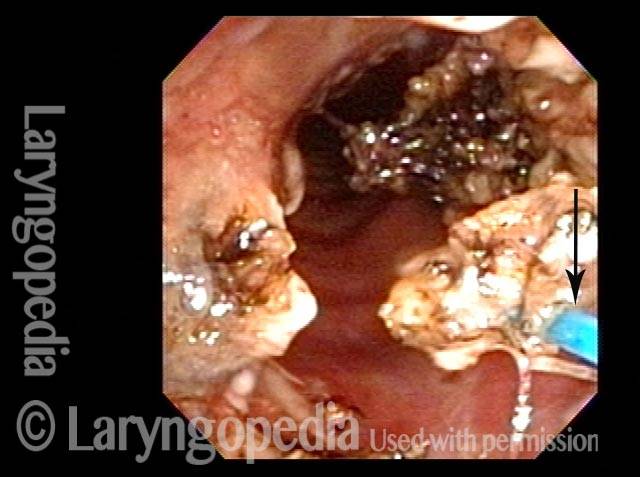
Obstructive papillomas (1 of 4)
Obstructive papillomas (1 of 4)
Local injections (2 of 4)
Local injections (2 of 4)
Removal of papilloma (3 of 4)
Removal of papilloma (3 of 4)
Improved breathing with papilloma removal (4 of 4)
Improved breathing with papilloma removal (4 of 4)
Identification of 11 Different HPV Subtypes in Adult Patients With RRP
Define the HPV subtypes seen in a large adult population with traditionally defined recurrent respiratory papillomatosis.
Age at diagnosis, but not HPV type, is strongly associated with clinical course in recurrent respiratory papillomatosis
A critical age at diagnosis which demarcates a more aggressive from less aggressive clinical course is identified...
Office Coagulation of Laryngeal Papillomas
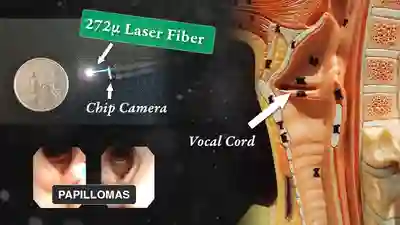
This man has had RRP (laryngeal papillomas) for many years. He has had laser ablations both in the O.R. under general anesthesia, and in an “office” laser room.
This video is an operative sequence in the latter setting. He is sitting in a chair and tolerating this procedure with the assistance of topical anesthesia and bilateral superior laryngeal nerve blocks, after which he can even drive himself home. In addition to thulium laser coagulation of the papillomas, this video also illustrates how patient movement and obscuring secretions must be managed.

Papillomas of the Larynx and Trachea
This video shows wart-like growths in the voicebox and windpipe (larynx and trachea) caused by chronic infection with the human papillomavirus (HPV).
Pulsed-KTP Laser Coagulation of Vocal Cord Papillomas
See a video demonstration of laser coagulation of vocal cord papillomas.
The Perfect Patient!!! | Topical Anesthesia for Laryngeal Surgery
This patient is sitting in a chair under topical anesthesia. He is able to minimize movement of his vocal cords, and is therefore a “perfect” candidate for office-based thulium laser ablation of residual laryngeal papilloma.
RRP – What Is It?
In this video, Dr. Robert Bastian discusses chronic human papilloma virus (HPV) infection of the larynx (especially vocal cords), causing hoarseness.