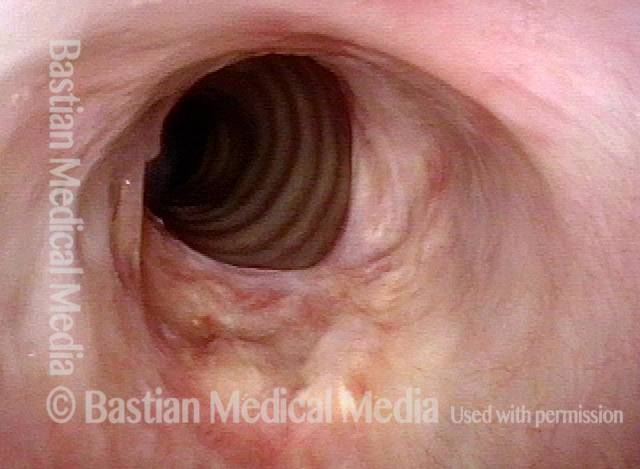
Arytenoid Chondritis / Perichondritis
An infectious or inflammatory response with ongoing ulceration or granulation on the superstructure of the arytenoid cartilage. Here we are talking of the arytenoid cartilage and/ or its thin “envelope” of fibrous tissue called perichondrium. The root chondr- refers to cartilage.
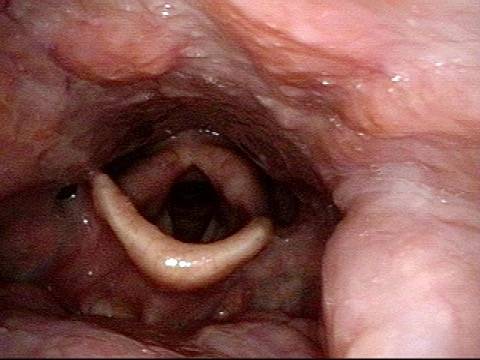
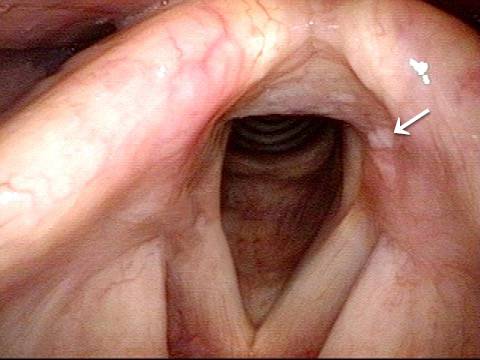
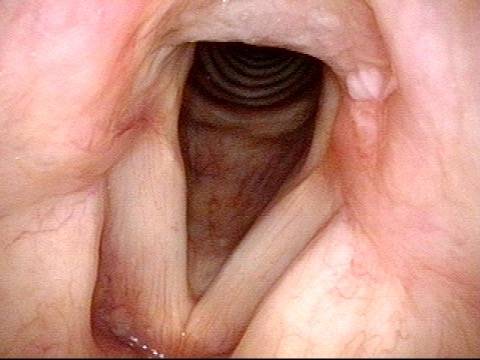
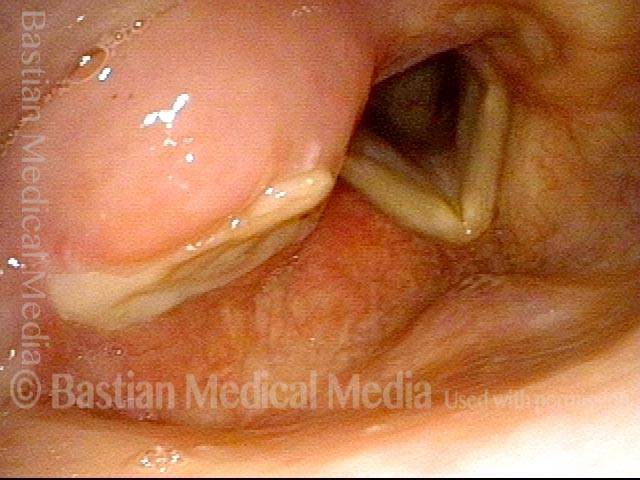
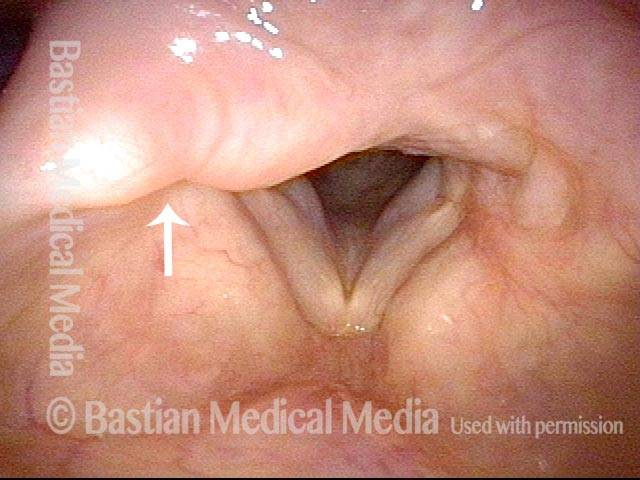
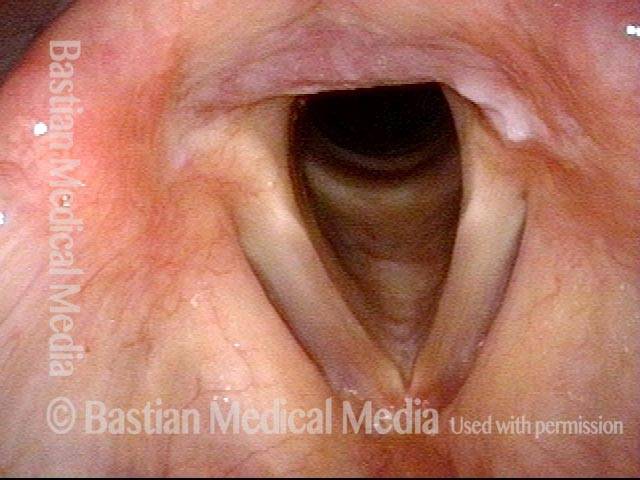
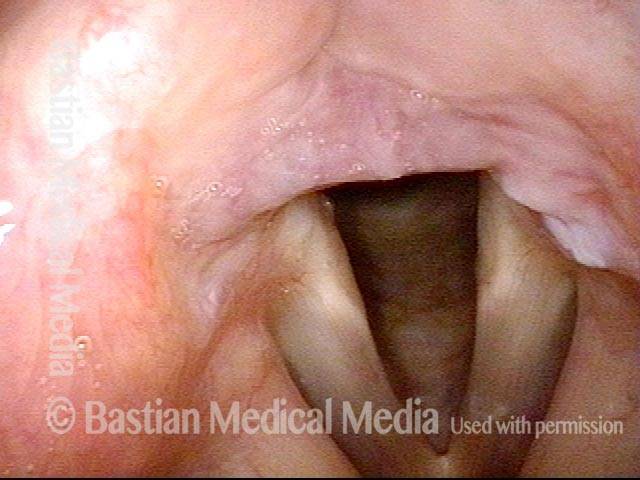
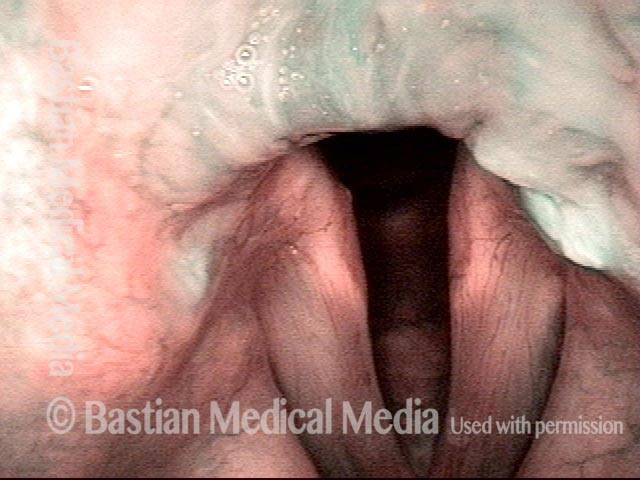
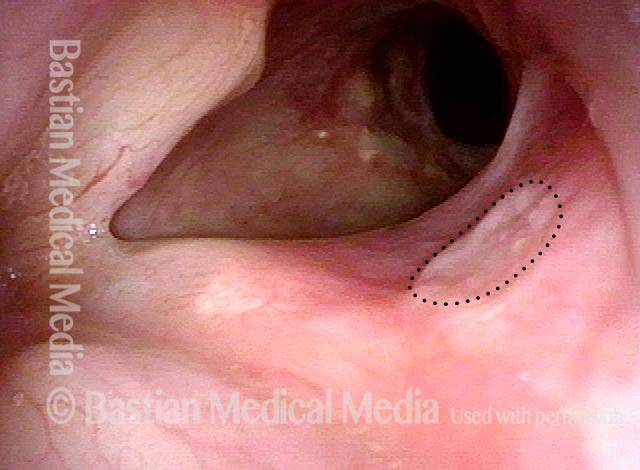
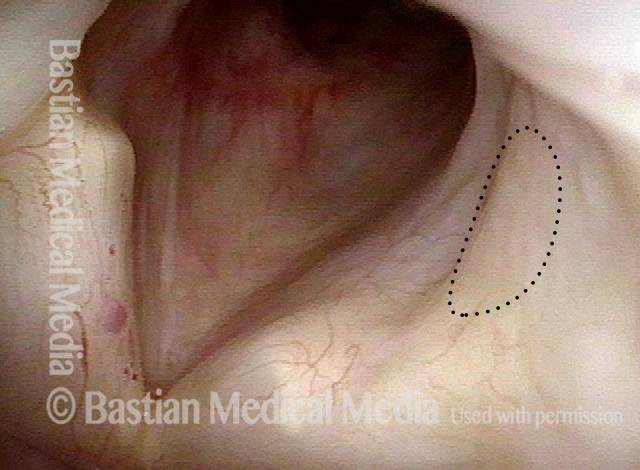
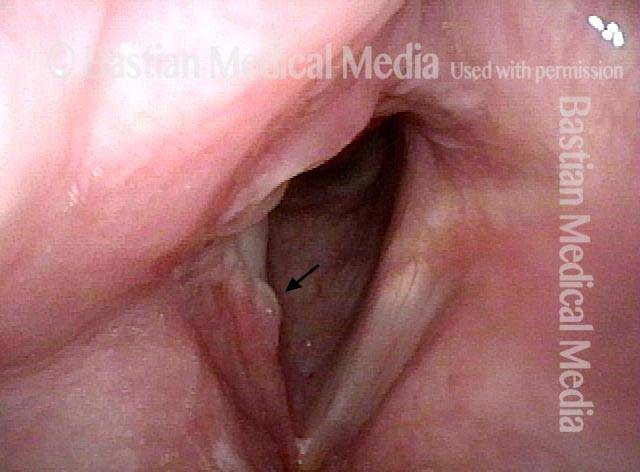
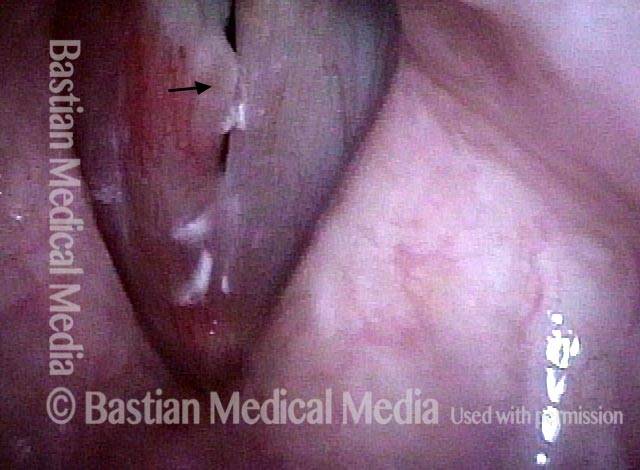
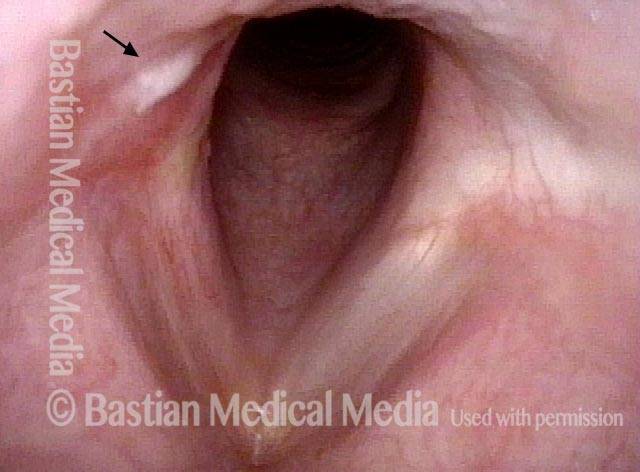
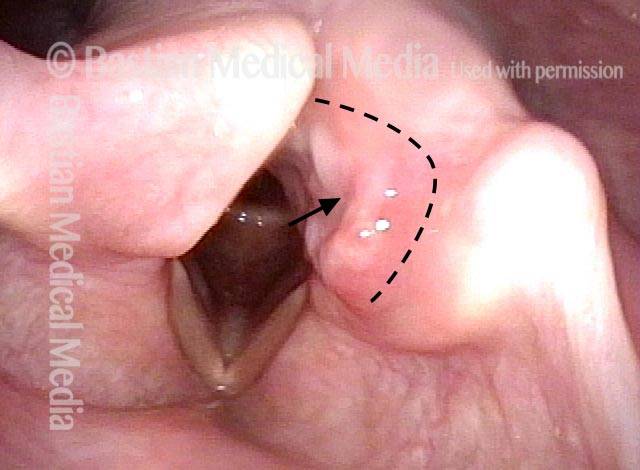
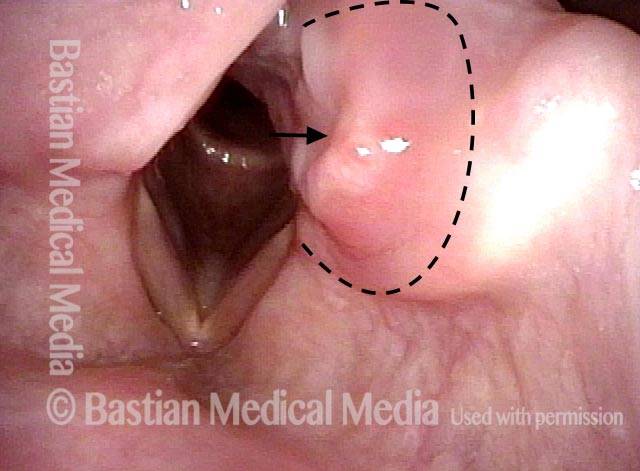
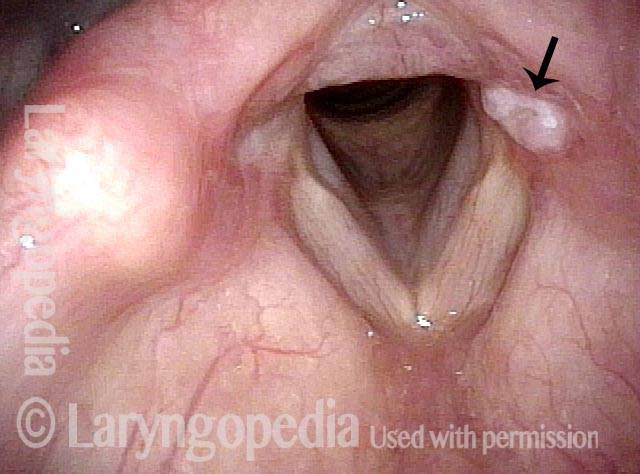
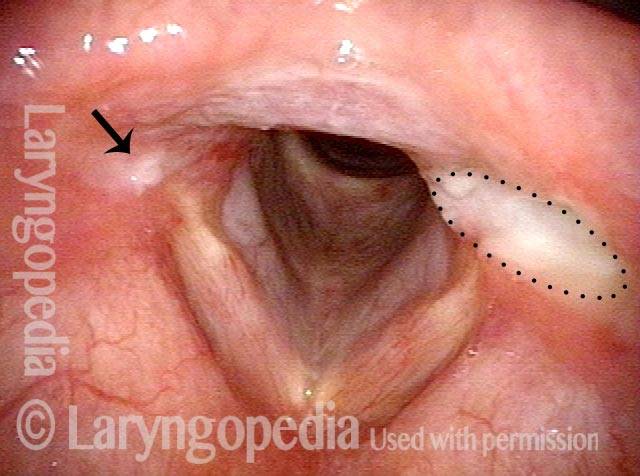
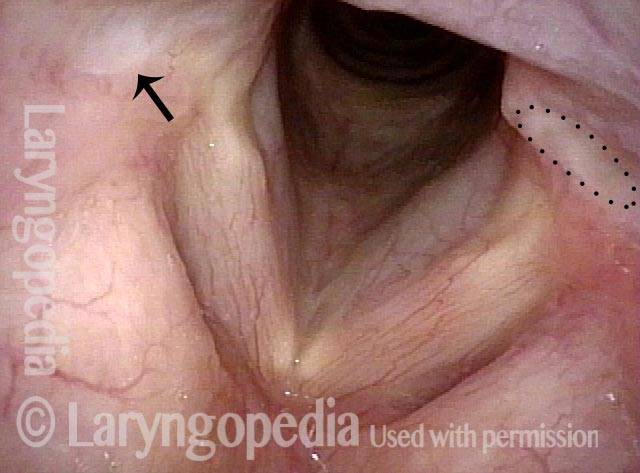
A similar and much more common disorder, contact granuloma or contact ulcer, occurs on the medial surface of the arytenoid cartilage, but low and at the level of the vocal process. When arytenoid chondritis or perichondritis occurs, on the anterior or high medial face of the cartilage as seen the the photo series below, it causes significant chronic and typically very focal pain that the person can point to with one finger.
We have never diagnosed the underlying cause of arytenoid perichondritis. It can be helpful to think of this as a “festering” kind of process, almost as if there is an embedded sliver that won’t let the area heal easily. If in fact it does heal, it can take many months. In one case, a patient was seen for the first time 2 years after symptom onset and a sequestrum was extruding from the area. When the patient is sufficiently tired of the pain and tired of waiting for resolution, the surgeon can offer definitive removal of the area of perichondrium and an area of cartilage beneath and then typically the area will heal, though often only after a time of re-granulation.
Arytenoid Perichondritis—an Issue of “Festering”
This middle-aged man has had a chronically sore throat on the left for at least 6 months. When asked to indicate where, he doesn’t gesture towards the throat as a whole, but points with one finger to the upper part of the thyroid cartilage fairly far laterally. He doesn’t remember being ill, or any other explanation. After seeing the lesion below, read the introductory article of this post for treatment of this condition.