Polypoid Degeneration (aka Reinke’s Edema, Smoker’s Polyps)
Polypoid degeneration is diffuse swelling of the vocal cords, due to build-up of edema fluid within the mucosa. It is also referred to as Reinke’s edema or smoker’s polyps. This condition is most often seen in long-term smokers who are also somewhat talkative. In other words, polypoid degeneration is rare in talkative non-smokers and also rare in taciturn smokers.
Symptoms of Polypoid Degeneration
Polypoid degeneration tends to virilize (masculinize) the quality and capabilities of the voice, and this effect is most noticeable in women. Also, in more severe cases, polypoid degeneration can induce involuntary inspiratory phonation or a fluttering, almost snoring sound during sudden inhalation.
Diagnosis of Polypoid Degeneration
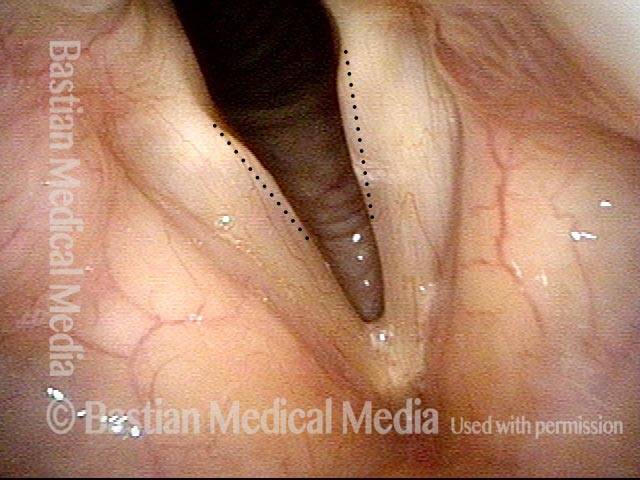
Polypoid degeneration typically appears as pale, watery bags of fluid attached to the superior surface and margins of the vocal cords. In less severe cases, the swelling might be more subtle, but if the patient is instructed to inhale while making voice, then the polypoid tissue will be drawn away from the cords into the glottic aperture, giving each vocal cord margin a convex contour and thereby becoming more noticeable (see two such examples in the photos below).
Treatment for Polypoid Degeneration
The patient is encouraged to give up smoking. Short-term voice therapy can help in some cases, reducing the turgidity of the polypoid tissue and thereby improving the voice to a small but noticeable extent. However, the polypoid degeneration itself is permanent, so if the voice quality remains unacceptable to the patient even after voice therapy, then surgery is necessary.
For surgery on polypoid degeneration, it was once common to strip away the polypoid tissue, but this approach often leads to an unacceptably high-pitched, thin-sounding, and husky voice. A better method is to reduce the tissue more conservatively, potentially leaving some fractional residual polypoid tissue. This way, although the voice might remain mildly virilized, it also retains a richer and more effortless quality.
Smoker’s Polyps, before and after Surgery (audio with photos)
Voice sample of a patient with smoker’s polyps, BEFORE surgery (see this patient’s photos just below): Same patient, two months AFTER surgery (the occasional syllable dropouts are due to the recentness of surgery):Smoker’s polyps, BEFORE surgery (1 of 4)
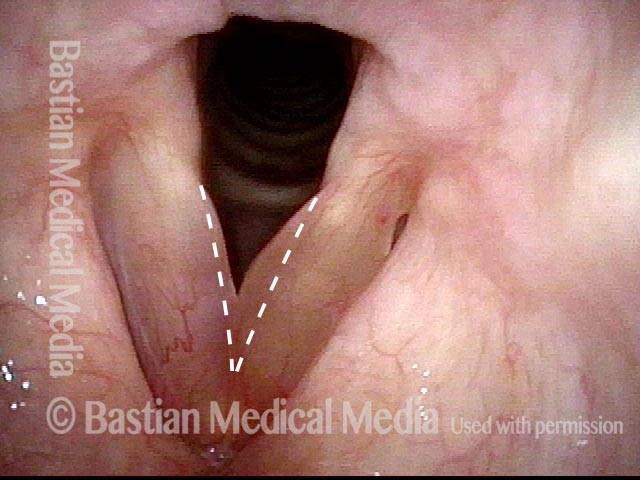
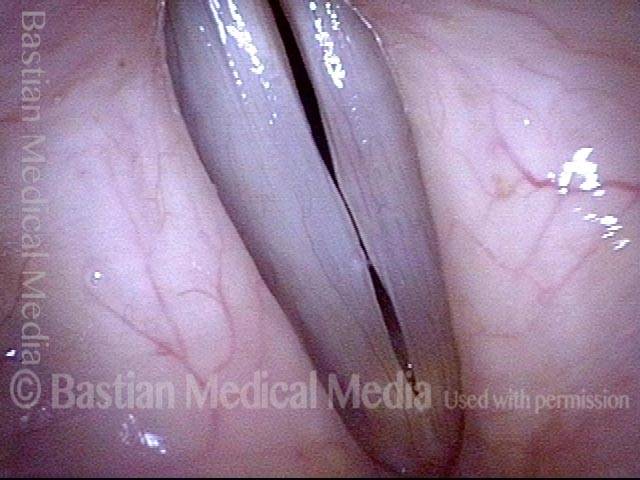
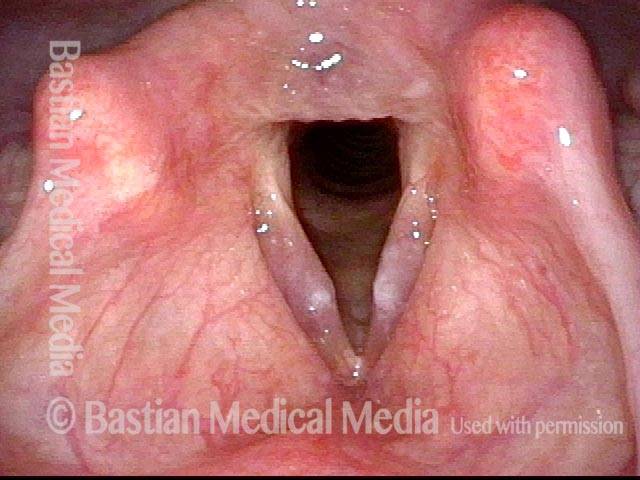
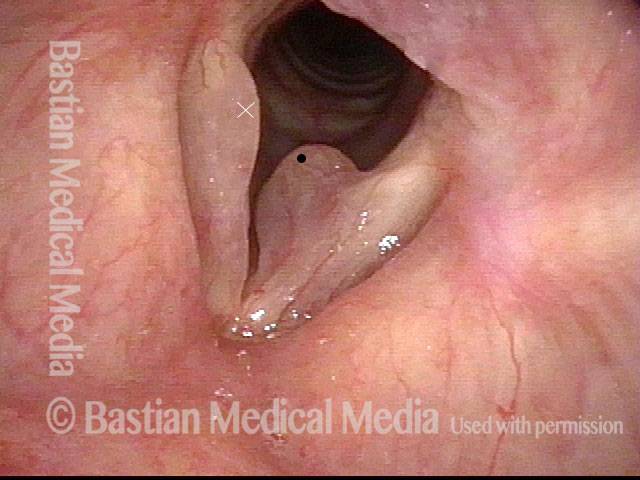
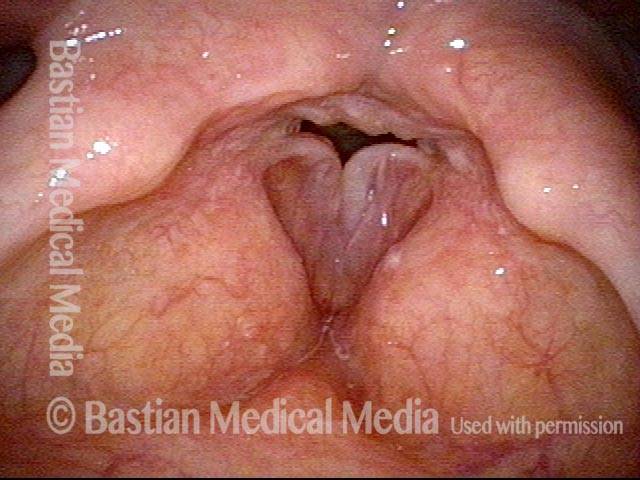
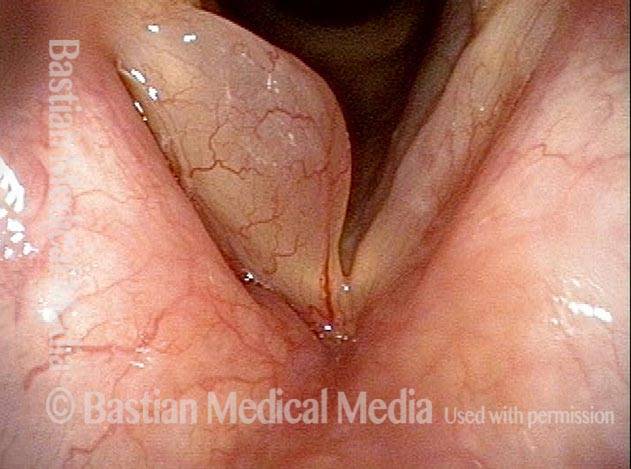
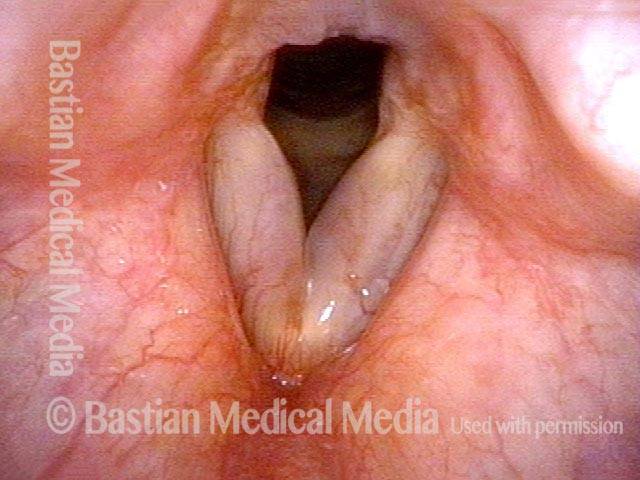
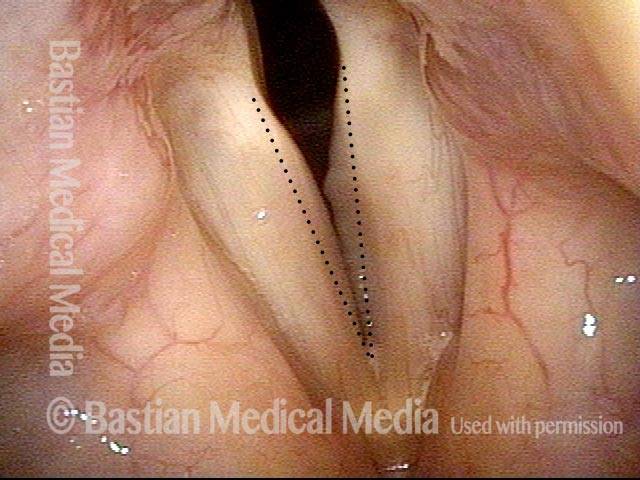
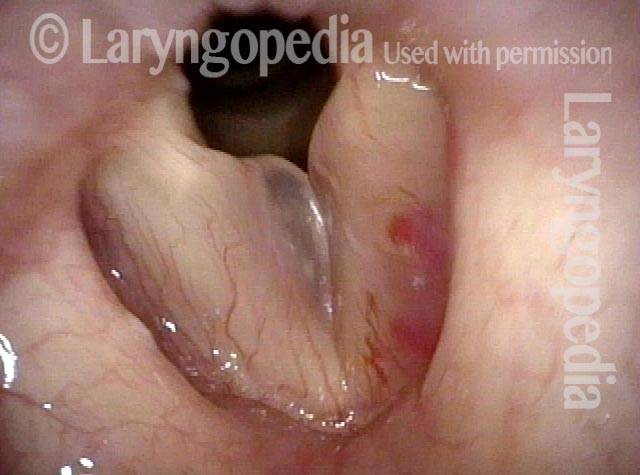
Smoker’s polyps, BEFORE surgery (1 of 4)
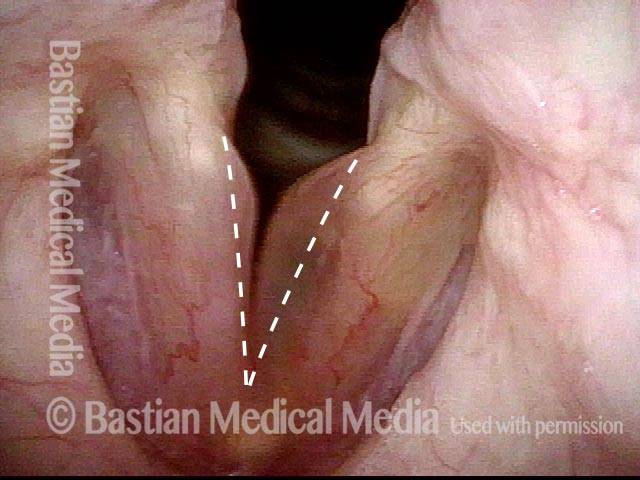
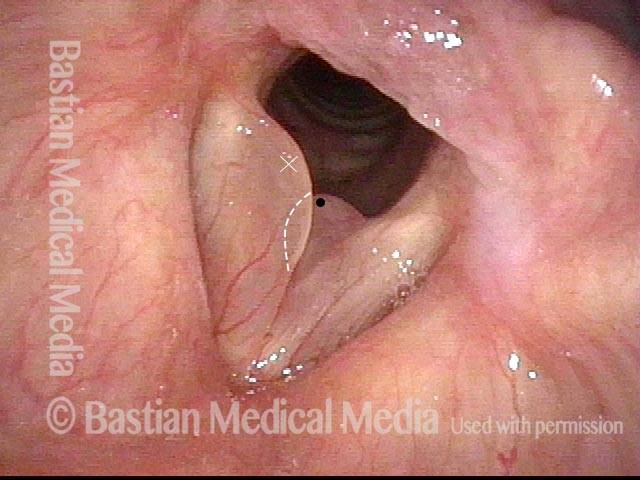
Smoker’s polyps, BEFORE surgery (2 of 4)
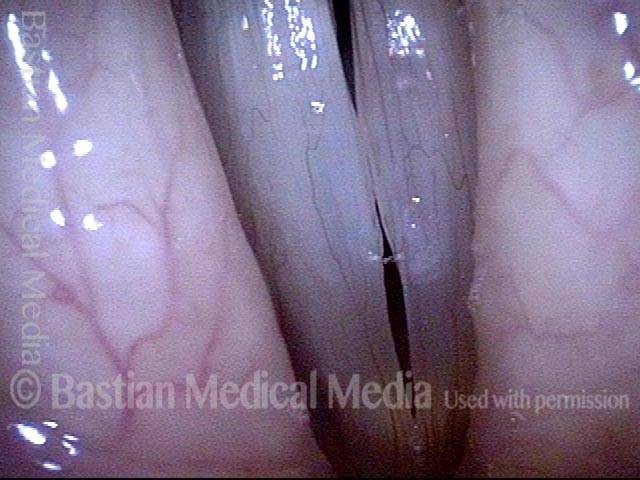
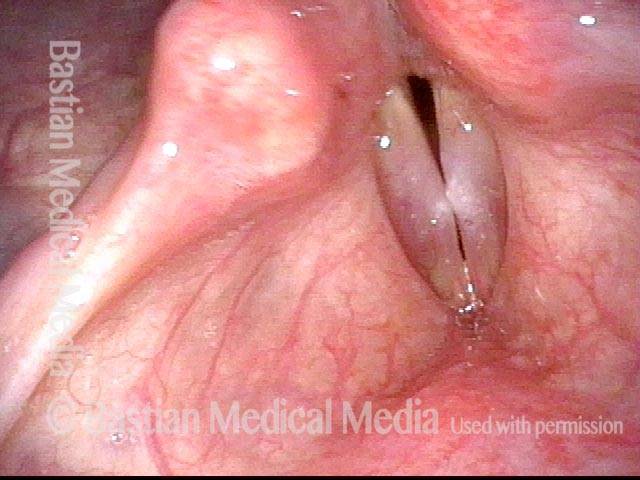
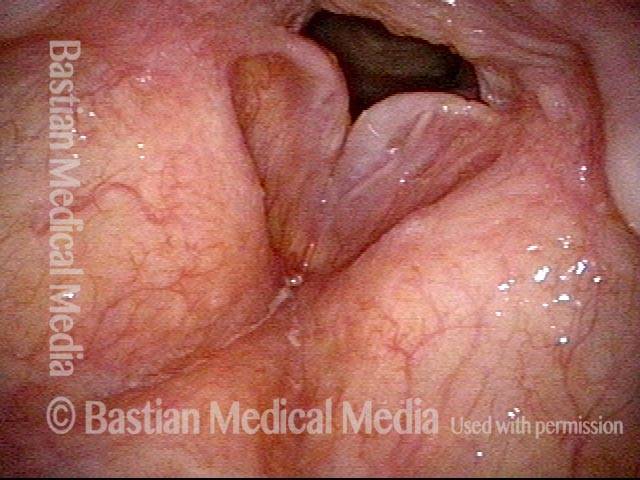
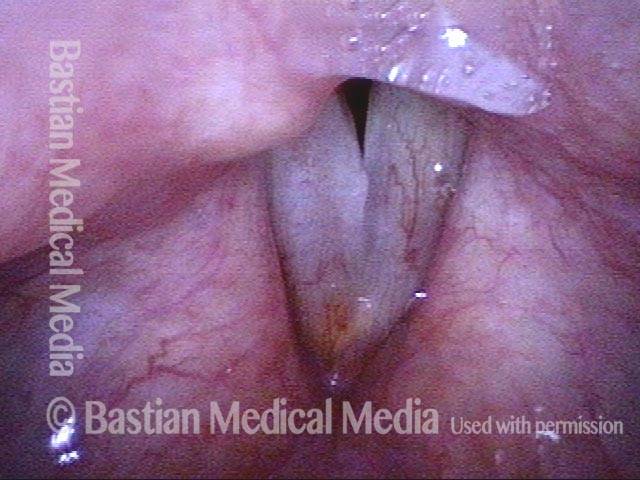
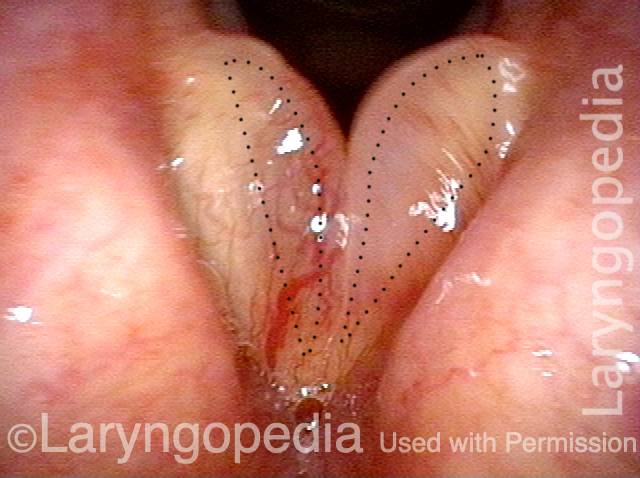
Smoker’s polyps, BEFORE surgery (2 of 4)
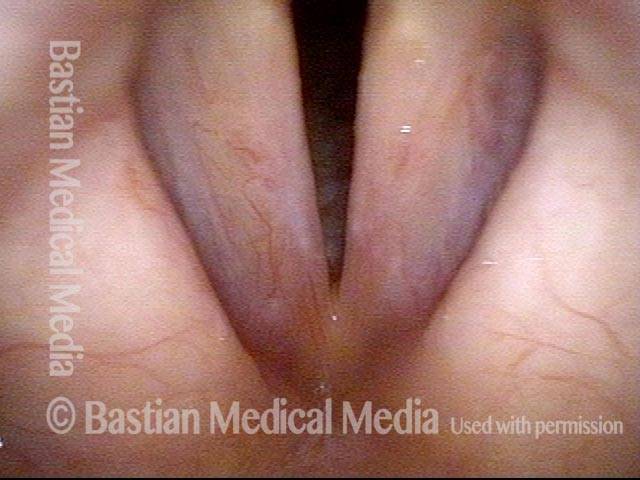
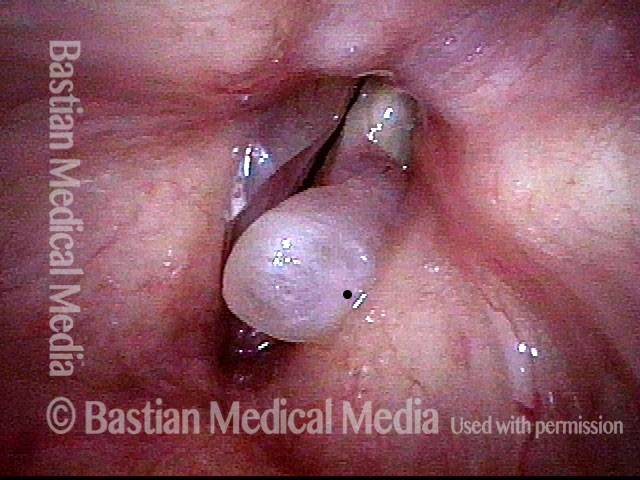
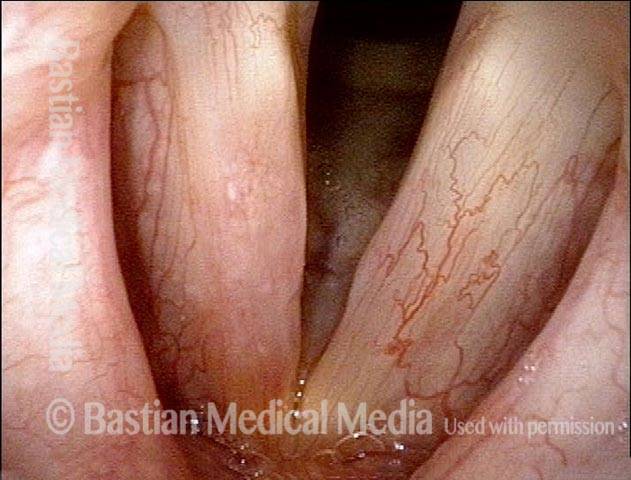
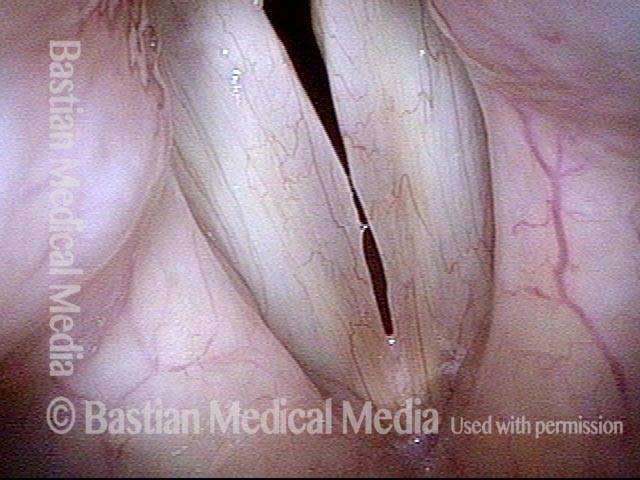
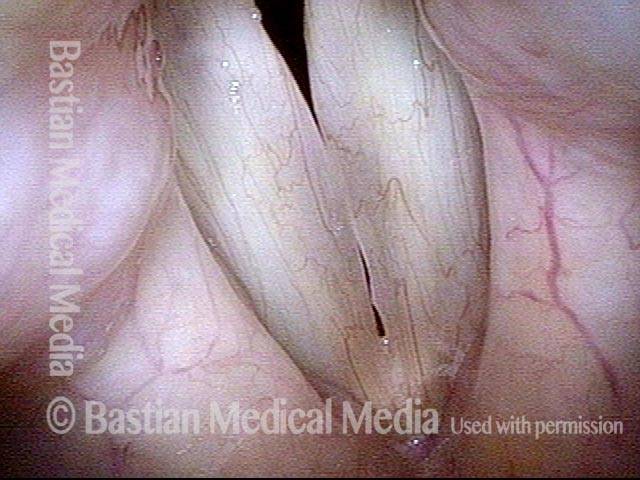
Smoker’s polyps, AFTER surgery (3 of 4)
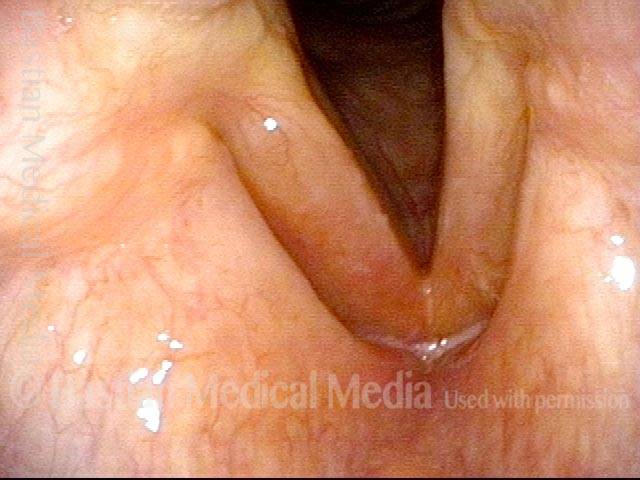
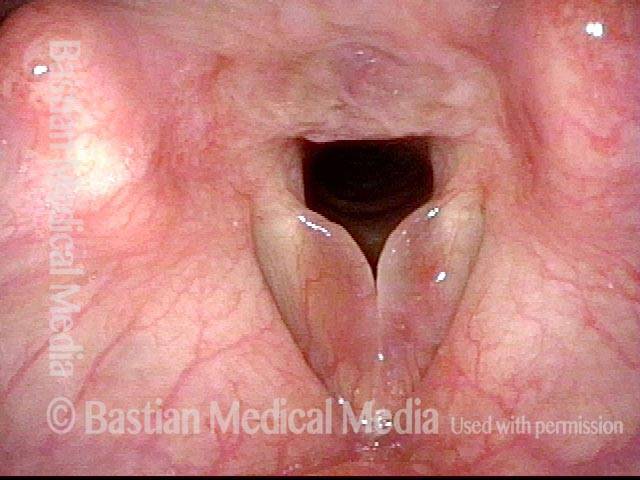
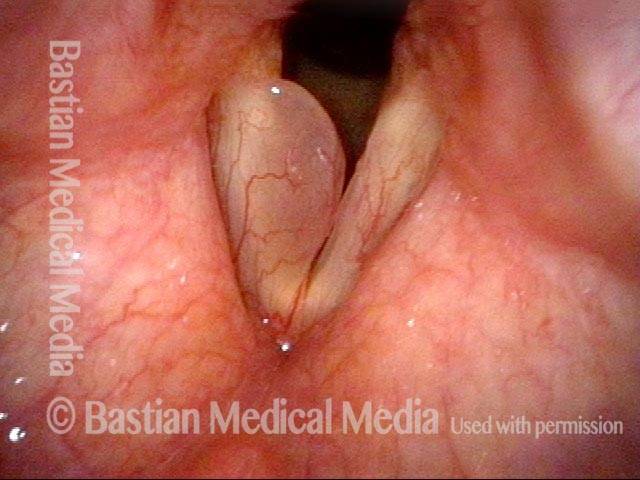
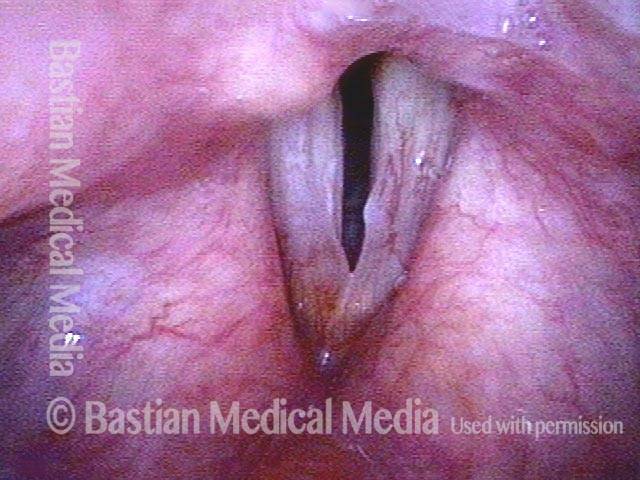
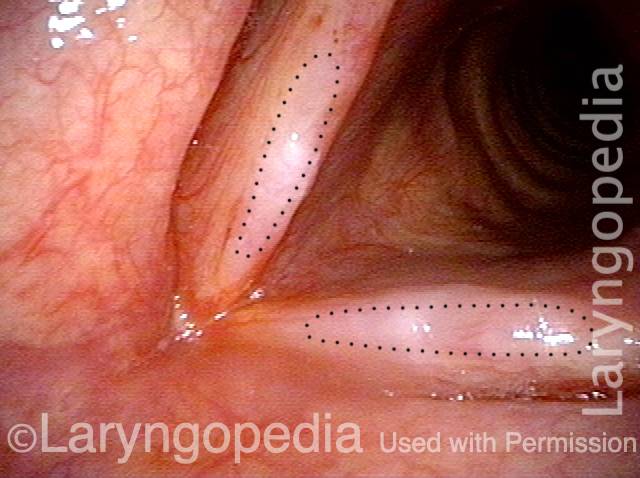
Smoker’s polyps, AFTER surgery (3 of 4)
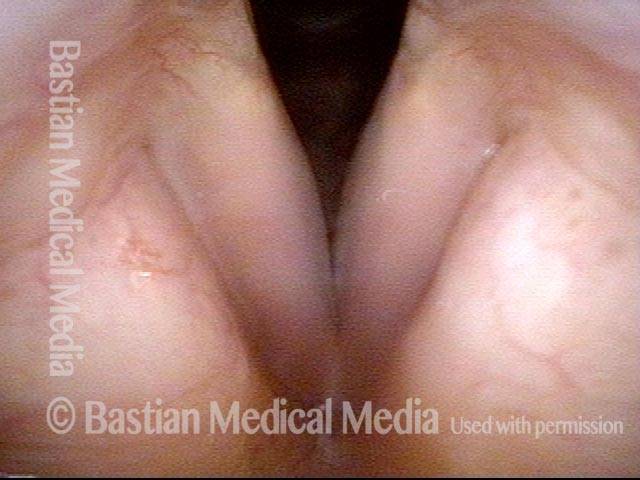
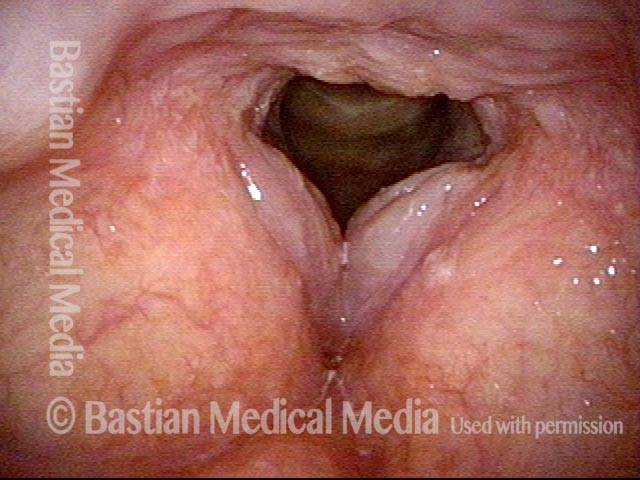
Smoker’s polyps, AFTER surgery (4 of 4)
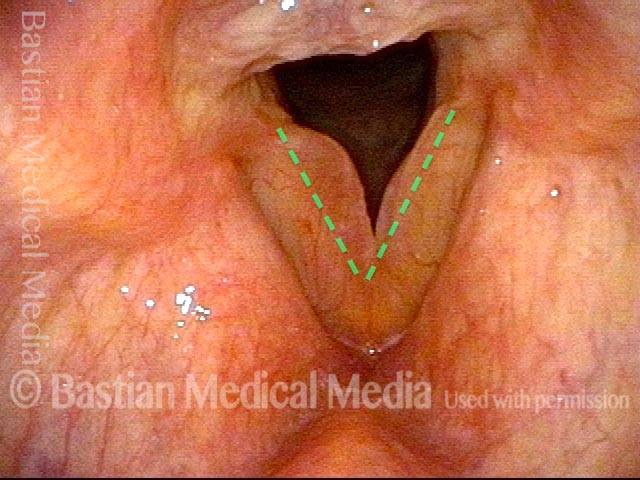
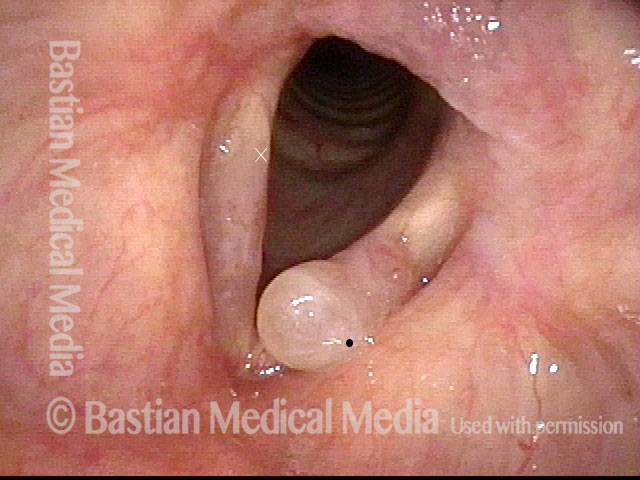
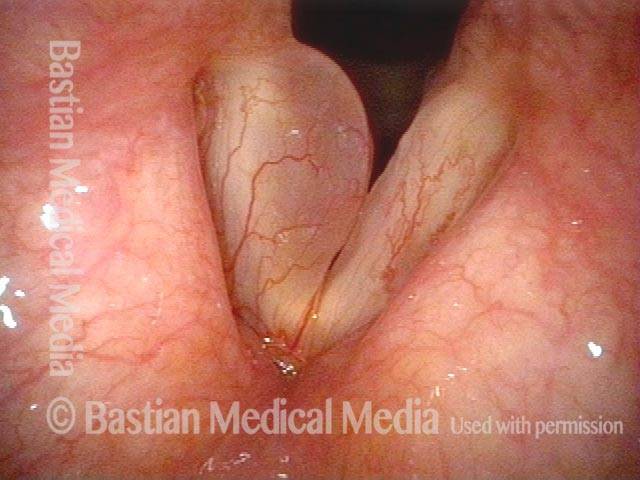
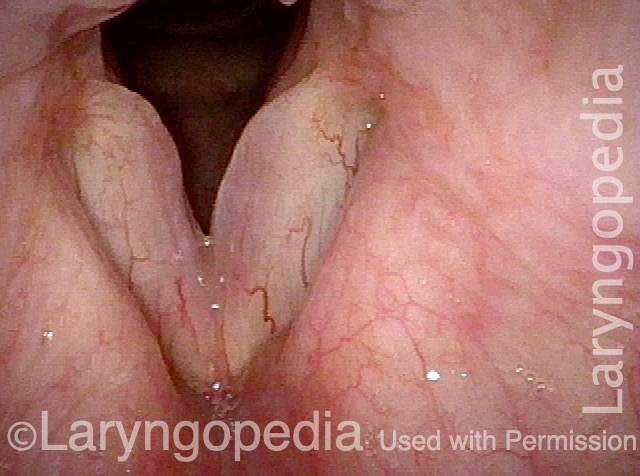
Smoker’s polyps, AFTER surgery (4 of 4)
Polypoid Vocal Nodules
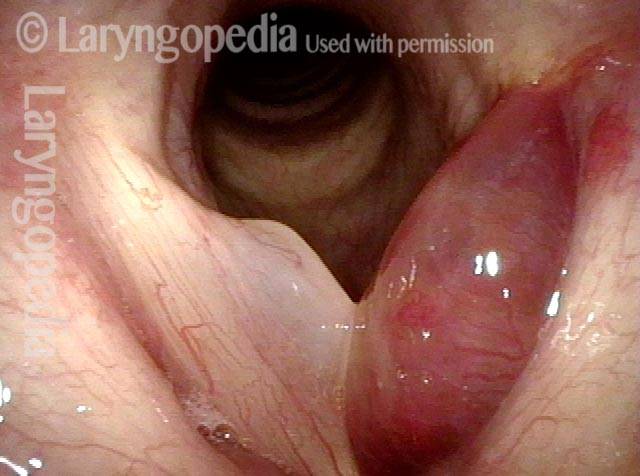
Polypoid vocal nodules (1 of 4)
Polypoid vocal nodules (1 of 4)
Incomplete closure (2 of 4)
Incomplete closure (2 of 4)
Polypoid vocal nodules (3 of 4)
Polypoid vocal nodules (3 of 4)
Polypoid vocal nodules (4 of 4)
Polypoid vocal nodules (4 of 4)
Smoker’s Polyps / Reinke’s Edema / Polypoid Degeneration
Smoker’s polyp / Reinke’s edema (1 of 2)
Smoker’s polyp / Reinke’s edema (1 of 2)
Smoker’s polyp / Reinke’s edema (2 of 2)
Smoker’s polyp / Reinke’s edema (2 of 2)
Example 2
Smoker’s polyps / Reinke’s edema (1 of 3)
Smoker’s polyps / Reinke’s edema (1 of 3)
Smoker’s polyps / Reinke’s edema (2 of 3)
Smoker’s polyps / Reinke’s edema (2 of 3)
Smoker’s polyps / Reinke’s edema (3 of 3)
Smoker’s polyps / Reinke’s edema (3 of 3)
Smoker’s Polyps in Various “Poses”
Smoker’s polyps in various “poses” (1 of 4)
Smoker’s polyps in various “poses” (1 of 4)
Polyp begins to fall off (2 of 4)
Polyp begins to fall off (2 of 4)
Polyps displace (3 of 4)
Polyps displace (3 of 4)
Edematous tissue causes a rough voice (4 of 4)
Edematous tissue causes a rough voice (4 of 4)
Smoker’s Polyps with Leukoplakia
Long-term smoker (1 of 4)
Long-term smoker (1 of 4)
Forced inspiration (2 of 4)
Forced inspiration (2 of 4)
Rapid inspiration (4 of 4)
Rapid inspiration (4 of 4)
Smoker’s Polyps and Thulium Laser
Pre-laser surgery, respiration (1 of 12)
Pre-laser surgery, respiration (1 of 12)
Pre-laser surgery, onset of phonation (2 of 12)
Pre-laser surgery, onset of phonation (2 of 12)
Pre-laser surgery (3 of 12)
Pre-laser surgery (3 of 12)
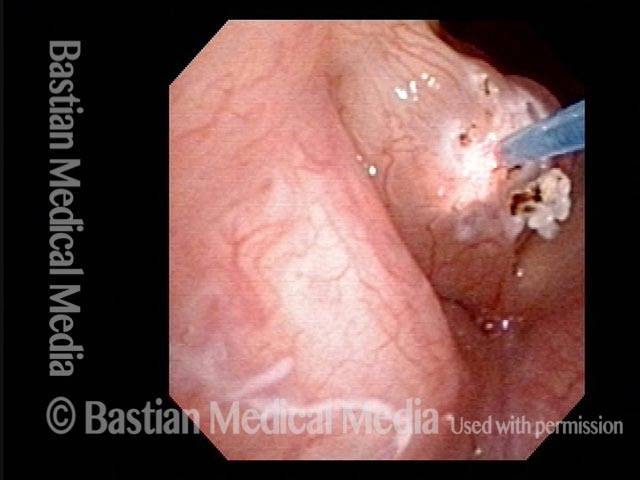
During laser surgery (4 of 12)
During laser surgery (4 of 12)
Post surgery, 28 days later (5 of 12)
Post surgery, 28 days later (5 of 12)
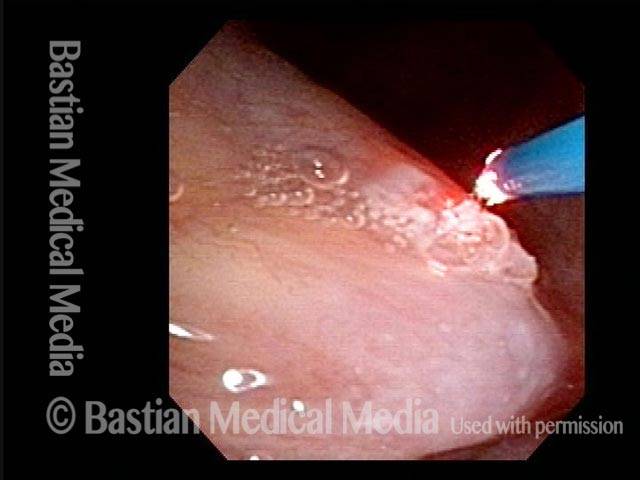
Second laser surgery (6 of 12)
Second laser surgery (6 of 12)
Post surgery, 21 days later (7 of 12)
Post surgery, 21 days later (7 of 12)
Post surgery, in-drawing of vocal cords (8 of 12)
Post surgery, in-drawing of vocal cords (8 of 12)
Post surgery, one year later (9 of 12)
Post surgery, one year later (9 of 12)
Post surgery, residual Reinke’s edema (10 of 12)
Post surgery, residual Reinke’s edema (10 of 12)
Post surgery, closed phase of vibration (11 of 12)
Post surgery, closed phase of vibration (11 of 12)
Post surgery, open phase of vibration (12 of 12)
Post surgery, open phase of vibration (12 of 12)
Reinke’s edema (smoking-related) and how to see it
Convexed vocal cords (1 of 4)
Convexed vocal cords (1 of 4)
Inspiratory phonation (2 of 4)
Inspiratory phonation (2 of 4)
Open phase, faint translucency (3 of 4)
Open phase, faint translucency (3 of 4)
Closed phase, faint translucency (4 of 4)
Closed phase, faint translucency (4 of 4)
Smoker’s Polyps with Two Explanations for Bruising
Bruising of left vocal cord (1 of 4)
Bruising of left vocal cord (1 of 4)
A year later (2 of 4)
A year later (2 of 4)
Inspiratory phonation (3 of 4)
Inspiratory phonation (3 of 4)
Translucent polyp, different view (4 of 4)
Translucent polyp, different view (4 of 4)
Smoker’s Polyp Reduction Improves Voice Even Though the Larynx Result May not be “Pretty”
Smokers Polyp (1 of 5)
Smokers Polyp (1 of 5)
Reine’s edema (2 of 5)
Reine’s edema (2 of 5)
A week after surgery (3 of 5)
A week after surgery (3 of 5)
Residual Reinke’s edema (4 of 5)
Residual Reinke’s edema (4 of 5)
Residual submucosal edema (5 of 5)
Residual submucosal edema (5 of 5)

Polypoid Degeneration (aka Smoker’s Polyps or Reinke’s Edema)
This video illustrates how smoker’s polyps can be seen more easily when the patient makes voice while breathing in (called inspiratory phonation). During inspiratory phonation, the polyps are drawn inward and become easier to identify.
What causes voice change in smokers?
Vocal fold changes more particularly caused by smoking include buildup of extra thickness of the mucosa from chronic edema to cause smoker’s polyps (Reinke’s edema). That condition deepens the voice as extra mass is added to the folds. Women begin to be called “sir” on the phone, and the male voice becomes hyper-masculinized.
Of course, leukoplakia (white patches) and precancerous or cancerous lesions can also degrade the voice. Clear diagnosis is always the first step for any smoker with a “gruff” voice!