Vocal Cord Synechia
Vocal cord synechia is a strand of scar tissue that tethers the vocal cords to each other. It can prevent the vocal cords from opening fully for breathing.
A synechia can also form in other parts of the body (Note the subglottic synechia shown below).
Vocal Cord Synechia: Before, During, and After Surgery
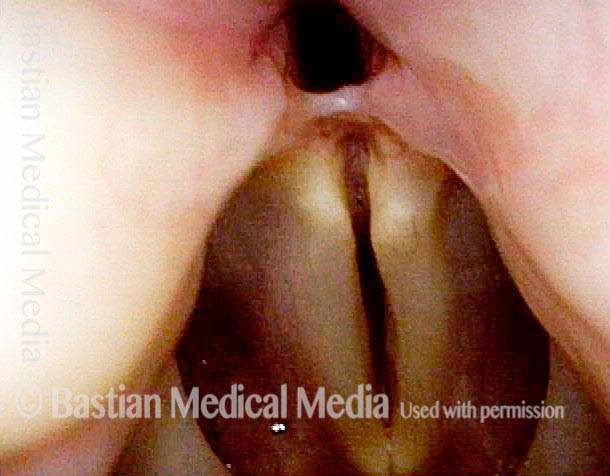
Vocal Cord Synechia (1 of 9)
Post-intubation synechia tethers the arytenoid cartilages together. This patient is tracheotomy-dependent.
Vocal Cord Synechia (1 of 9)
Post-intubation synechia tethers the arytenoid cartilages together. This patient is tracheotomy-dependent.
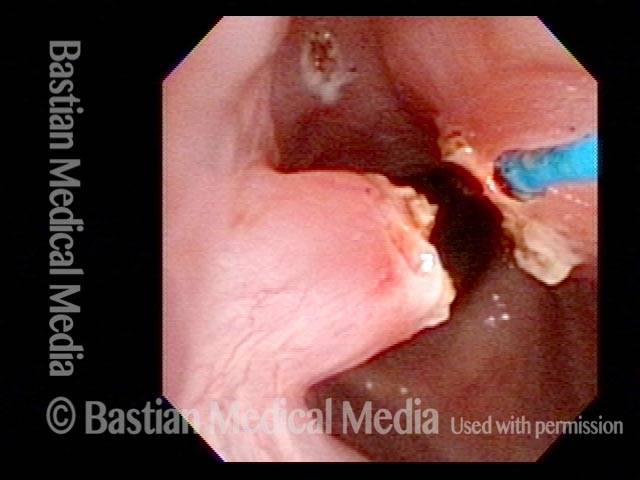
Vocal cord synechia, during surgery (2 of 9)
Operative view of synechia (“v” of the vocal cords is inverted). Notice that the vocal cords are completely approximated because the synechia has bound them together.
Vocal cord synechia, during surgery (2 of 9)
Operative view of synechia (“v” of the vocal cords is inverted). Notice that the vocal cords are completely approximated because the synechia has bound them together.
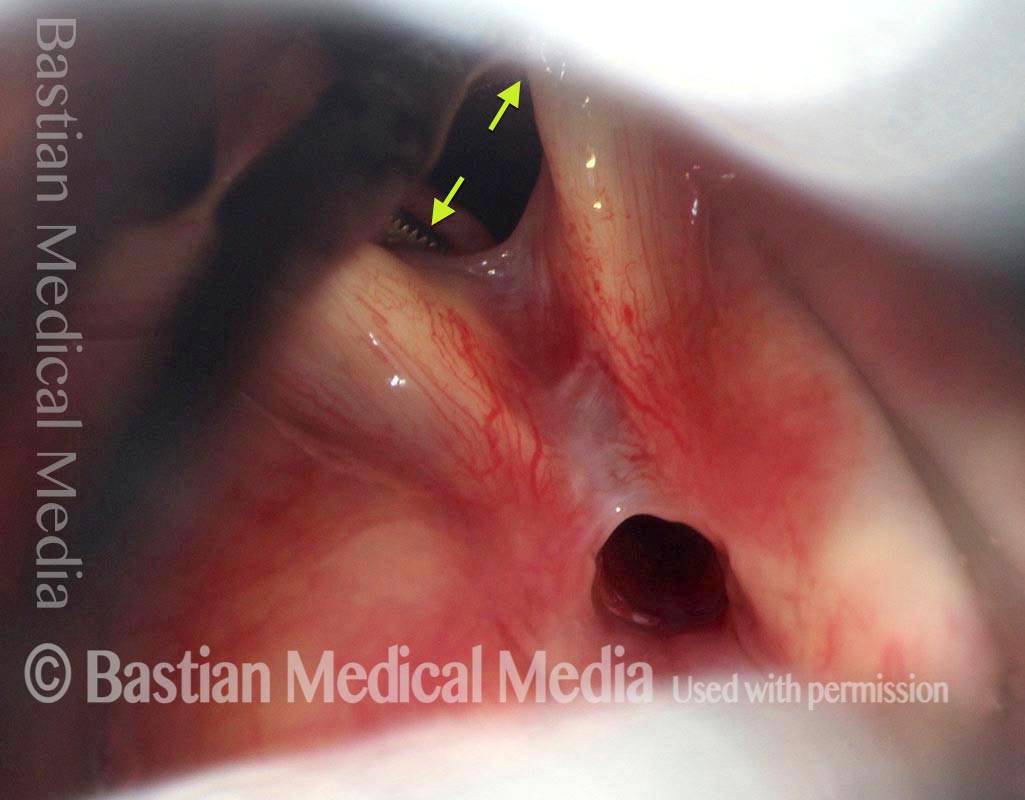
Vocal cord synechia, during surgery (3 of 9)
Tiny forceps is separating the cords (arrows) and more clearly shows the extent of the synechia.
Vocal cord synechia, during surgery (3 of 9)
Tiny forceps is separating the cords (arrows) and more clearly shows the extent of the synechia.
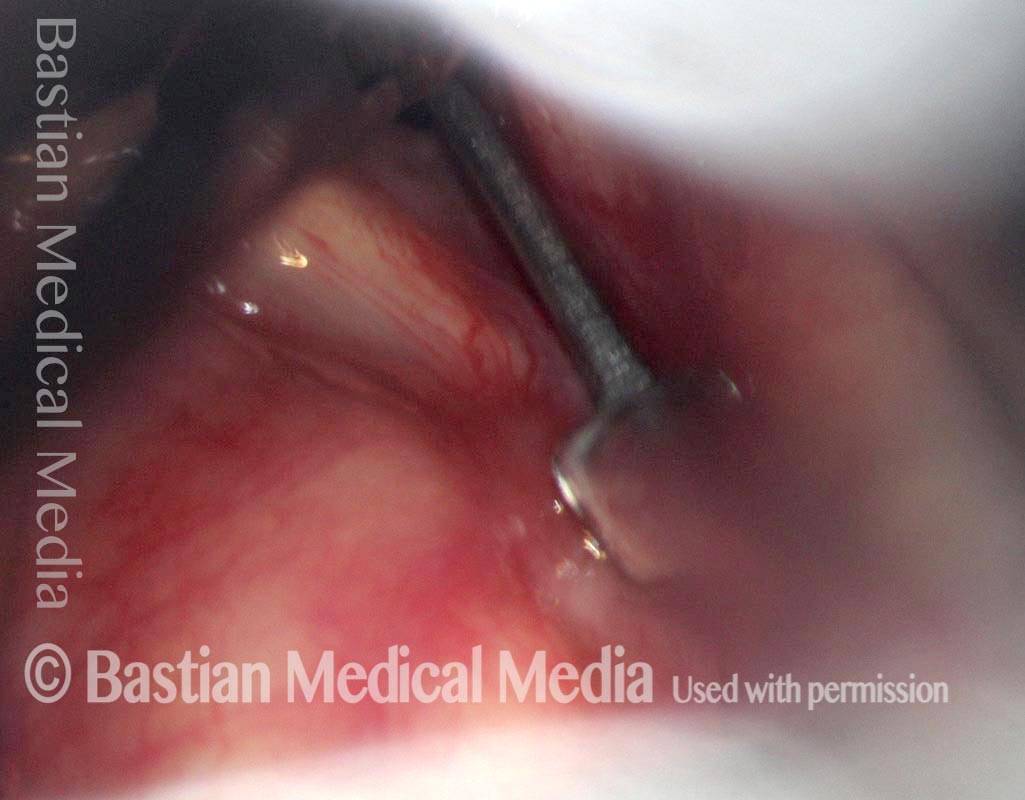
Vocal cord synechia, during surgery (4 of 9)
Micro-scissors in position to divide the synechia cleanly. For perspective, the blade of the scissors is only a few millimeters long.
Vocal cord synechia, during surgery (4 of 9)
Micro-scissors in position to divide the synechia cleanly. For perspective, the blade of the scissors is only a few millimeters long.
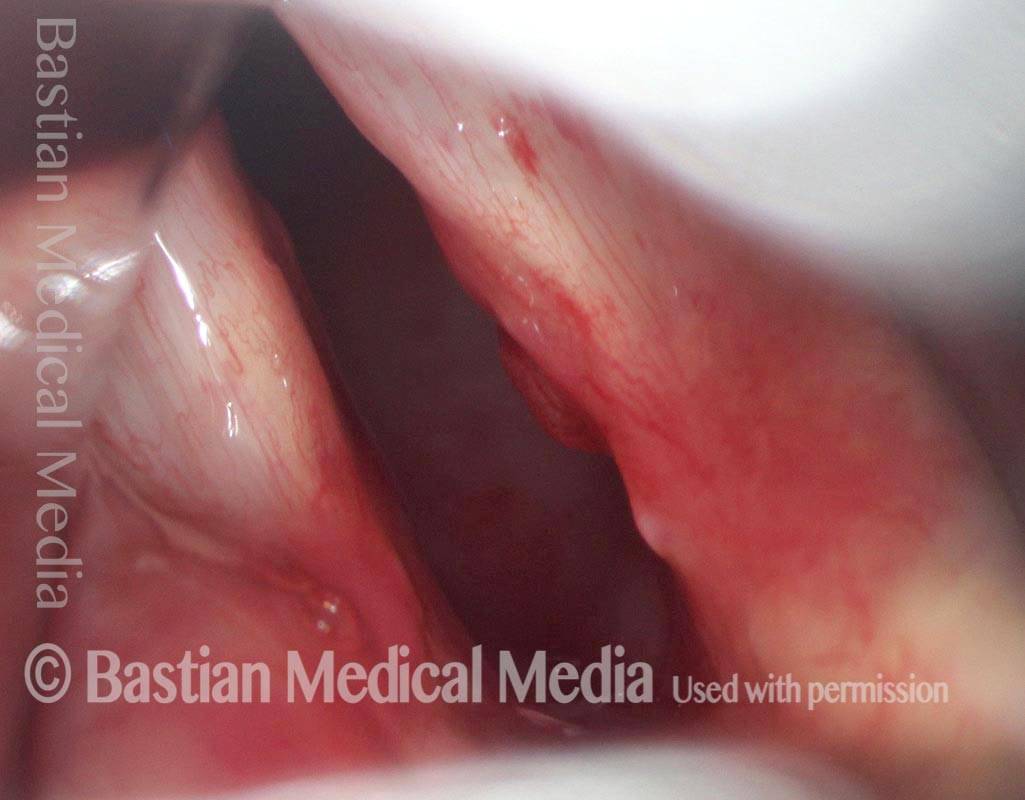
Vocal cord synechia, during surgery (5 of 9)
After division of the synechia and topical application of an anti-scarring agent.
Vocal cord synechia, during surgery (5 of 9)
After division of the synechia and topical application of an anti-scarring agent.
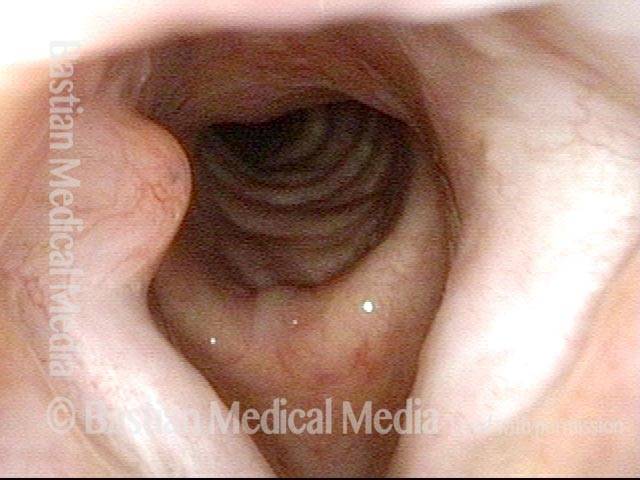
Vocal cord synechia, after surgery (6 of 9)
Five days after surgery. Vocal cords are able to separate for breathing, and the tracheotomy tube can be removed. Compare with photo 1.
Vocal cord synechia, after surgery (6 of 9)
Five days after surgery. Vocal cords are able to separate for breathing, and the tracheotomy tube can be removed. Compare with photo 1.
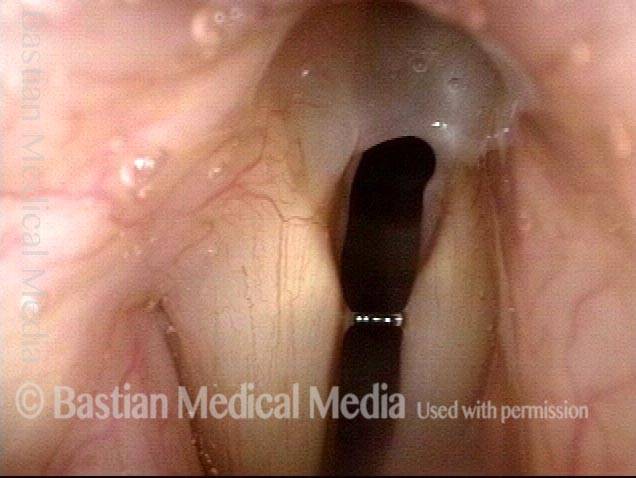
Vocal Cord Synechia, after surgery (7 of 9)
Completely healed larynx after release of synechia. Abduction completely restored.
Vocal Cord Synechia, after surgery (7 of 9)
Completely healed larynx after release of synechia. Abduction completely restored.
Vocal cord synechia, after surgery (8 of 9)
As the vocal cords are coming together for phonation (not yet completely adducted).
Vocal cord synechia, after surgery (8 of 9)
As the vocal cords are coming together for phonation (not yet completely adducted).
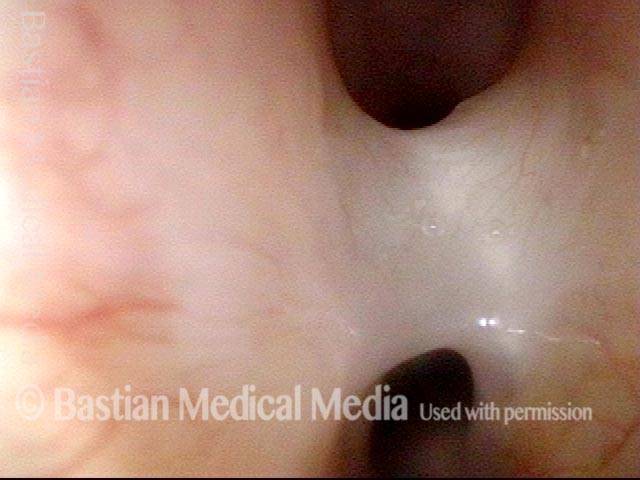
Vocal cord synechia, after surgery (9 of 9)
Closer view. Can hardly see where the synechia was. Compare again with photo 1.
Vocal cord synechia, after surgery (9 of 9)
Closer view. Can hardly see where the synechia was. Compare again with photo 1.
Ossified Synechia Resists Thulium Laser
Ossified synechia (1 of 8)
This 75-year-old woman suffered complications after open heart surgery, and was intubated for three weeks. Nearly two years later, she remains short of breath and bothered by difficulty mobilizing secretions. On initial examination, a synechia was identified; at patient request, microlaryngoscopy was scheduled both to divide the synechia and to inject voice gel into the deficient posterior commissure. At surgery, a view sufficient to divide the synechia was not possible. The patient was rescheduled for office-based thulium laser division of the synechia.
Ossified synechia (1 of 8)
This 75-year-old woman suffered complications after open heart surgery, and was intubated for three weeks. Nearly two years later, she remains short of breath and bothered by difficulty mobilizing secretions. On initial examination, a synechia was identified; at patient request, microlaryngoscopy was scheduled both to divide the synechia and to inject voice gel into the deficient posterior commissure. At surgery, a view sufficient to divide the synechia was not possible. The patient was rescheduled for office-based thulium laser division of the synechia.
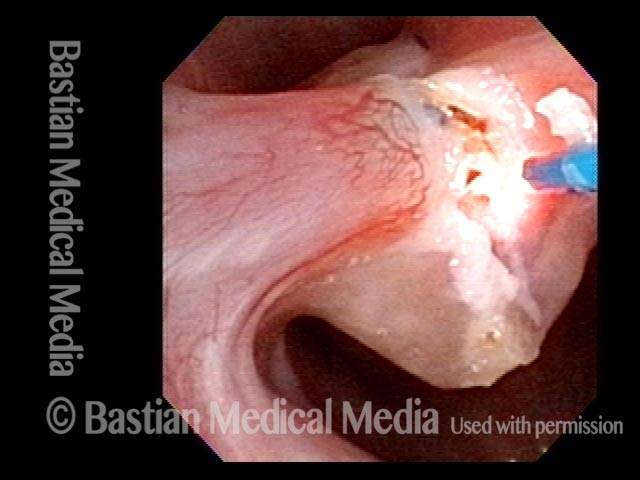
Ossified Synechia, during first laser treatment (2 of 8)
Close-range view of the synechia. The tip of the glass fiber through which laser energy will be delivered is seen just inferior to the synechia.
Ossified Synechia, during first laser treatment (2 of 8)
Close-range view of the synechia. The tip of the glass fiber through which laser energy will be delivered is seen just inferior to the synechia.
Ossified synechia, during first laser treatment (3 of 8)
As the synechia is divided, a core of bone formation is exposed. More than half of the laser energy has been delivered to this spar of bone, yet it will not yield. The tip of the scope has also been flexed against the synechia to no avail. A second attempt with higher energy laser has been scheduled.
Ossified synechia, during first laser treatment (3 of 8)
As the synechia is divided, a core of bone formation is exposed. More than half of the laser energy has been delivered to this spar of bone, yet it will not yield. The tip of the scope has also been flexed against the synechia to no avail. A second attempt with higher energy laser has been scheduled.
Ossified synechia, 4 months later (4 of 8)
Four months later. The synechia remains, and there is residual granulation tissue on its undersurface. It’s not yet known whether the spar of bone is still present. Compare with photo 2.
Ossified synechia, 4 months later (4 of 8)
Four months later. The synechia remains, and there is residual granulation tissue on its undersurface. It’s not yet known whether the spar of bone is still present. Compare with photo 2.
Ossified synechia, 4 months later (5 of 8)
Now, with the thulium laser, beginning a second attempt at dividing the synechia.
Ossified synechia, 4 months later (5 of 8)
Now, with the thulium laser, beginning a second attempt at dividing the synechia.
Ossified synechia, 4 months later (6 of 8)
The spar of bone is not found within the synechia (apparently turned to ash during the original procedure four months earlier), and now the scar band is divided. The patient could feel the difference in her breathing immediately.
Ossified synechia, 4 months later (6 of 8)
The spar of bone is not found within the synechia (apparently turned to ash during the original procedure four months earlier), and now the scar band is divided. The patient could feel the difference in her breathing immediately.
Synechia gone, 6 months later (7 of 8)
Six months after the initial laser treatment for this patient’s bone-containing synechia. The synechia is now gone, with only a small residual projection remaining, left of photo. The vocal cords also separate more widely, to a wider “V”.
Synechia gone, 6 months later (7 of 8)
Six months after the initial laser treatment for this patient’s bone-containing synechia. The synechia is now gone, with only a small residual projection remaining, left of photo. The vocal cords also separate more widely, to a wider “V”.
Synechia gone, 6 months later (8 of 8)
During phonation. The divots from pressure necrosis of the endotracheal tube remain evident. In spite of them, the patient’s voice is excellent.
Synechia gone, 6 months later (8 of 8)
During phonation. The divots from pressure necrosis of the endotracheal tube remain evident. In spite of them, the patient’s voice is excellent.
Vocal Cord Synechia
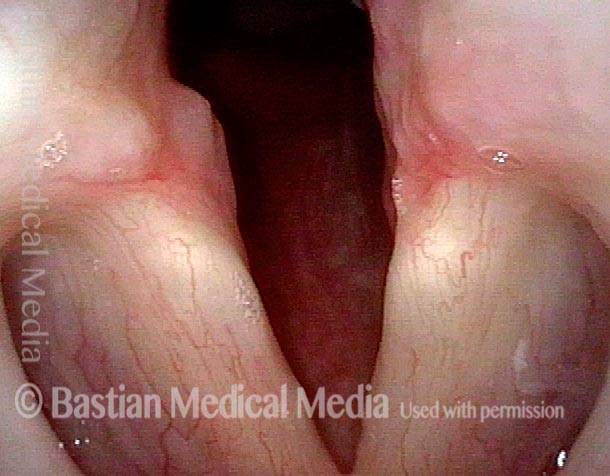
Vocal cord synechia (1 of 4)
Note that the vocal cords cannot fully abduct, due to the presence of a synechia, which tethers them to each other posteriorly.
Vocal cord synechia (1 of 4)
Note that the vocal cords cannot fully abduct, due to the presence of a synechia, which tethers them to each other posteriorly.
Vocal cord synechia (2 of 4)
Same patient during phonation.
Vocal cord synechia (2 of 4)
Same patient during phonation.
Vocal cord synechia (3 of 4)
Same patient at closer range.
Vocal cord synechia (3 of 4)
Same patient at closer range.
Vocal cord synechia (4 of 4)
Same patient. Synechia in full view.
Vocal cord synechia (4 of 4)
Same patient. Synechia in full view.
Intubation Injury, Including a Subglottic Synechia
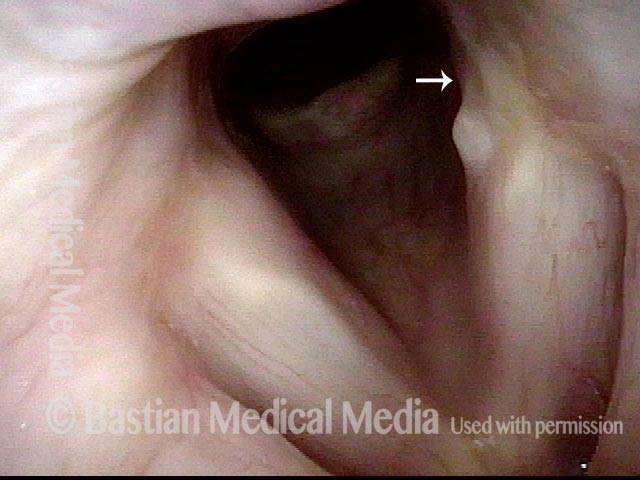
Intubation injury, including a subglottic synechia (1 of 2)
View of the vocal cords, in abducted position, in a patient with voice change after long-term intubation due to brain injury. Injury of the left posterior vocal cord (right of image) can be seen, where pressure from the breathing tube caused an erosion or divot (arrow). The synechia is not yet visible from this viewing perspective.
Intubation injury, including a subglottic synechia (1 of 2)
View of the vocal cords, in abducted position, in a patient with voice change after long-term intubation due to brain injury. Injury of the left posterior vocal cord (right of image) can be seen, where pressure from the breathing tube caused an erosion or divot (arrow). The synechia is not yet visible from this viewing perspective.
Intubation injury, including a subglottic synechia (2 of 2)
Same patient, just below the level of the cords. This synechia, located posteriorly, is additional evidence of breathing tube injury.
Intubation injury, including a subglottic synechia (2 of 2)
Same patient, just below the level of the cords. This synechia, located posteriorly, is additional evidence of breathing tube injury.
Synechia Hidden by Overhanging Arytenoid Superstructure
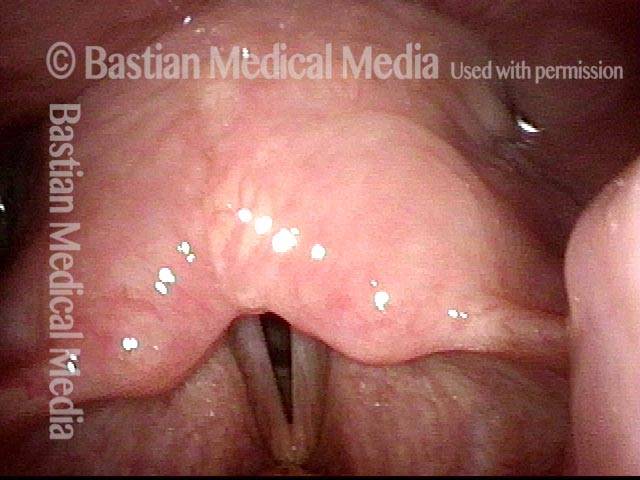
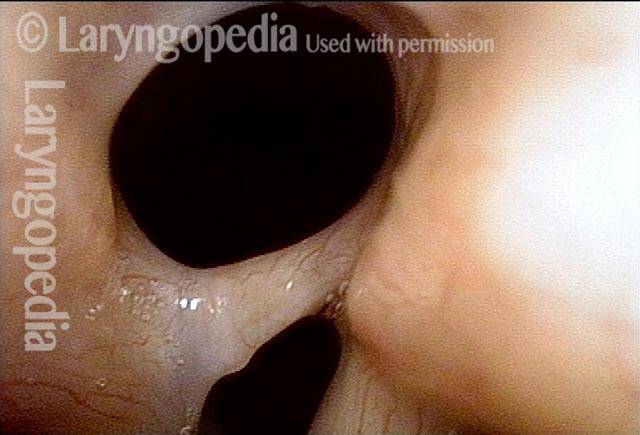
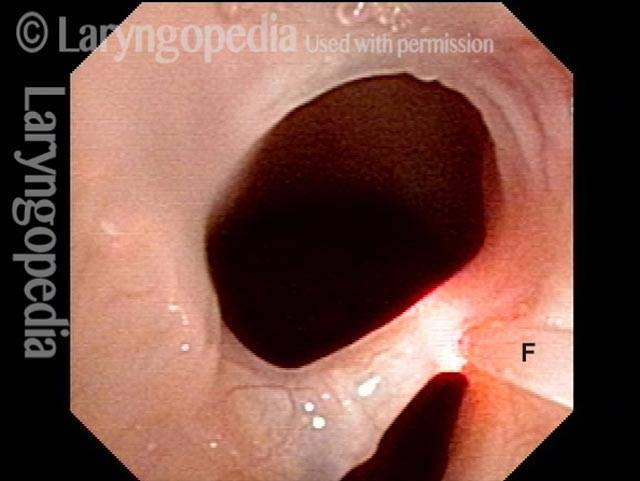
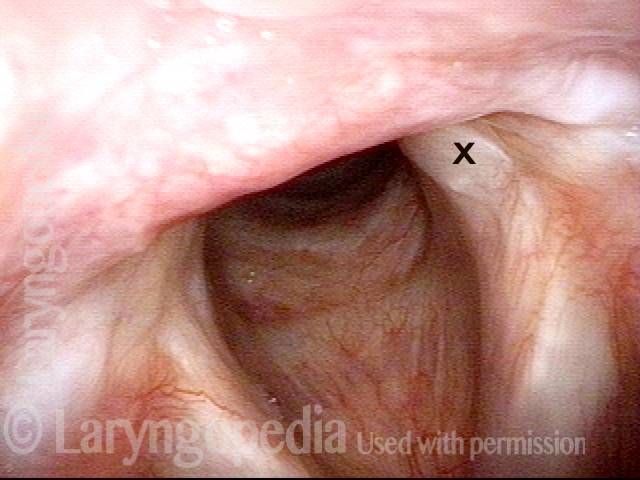
Synechia hidden by overhanging arytenoid superstructure (1 of 4)
Maximum possible abduction of the vocal cords, as seen a few months after an illness that required endotracheal intubation for 3 weeks. This person experienced noisy breathing with any significant exertion.
Synechia hidden by overhanging arytenoid superstructure (1 of 4)
Maximum possible abduction of the vocal cords, as seen a few months after an illness that required endotracheal intubation for 3 weeks. This person experienced noisy breathing with any significant exertion.
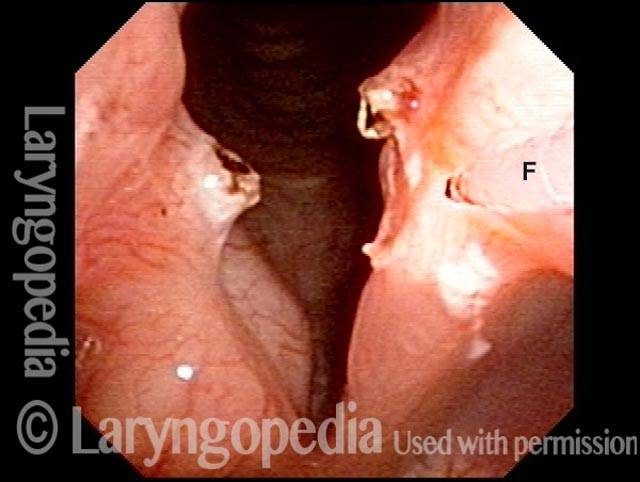
Synechia hidden by overhanging arytenoid superstructure (2 of 4)
With elicited sudden inhalation the inspiratory air draws the vocal cords together, and the result is involuntary inspiratory phonation.
Synechia hidden by overhanging arytenoid superstructure (2 of 4)
With elicited sudden inhalation the inspiratory air draws the vocal cords together, and the result is involuntary inspiratory phonation.
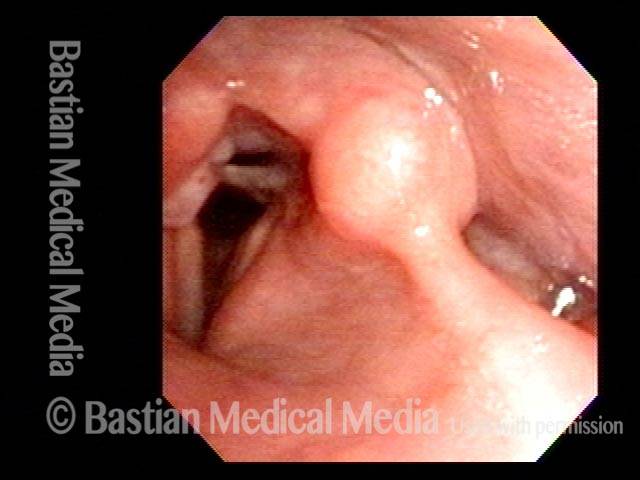
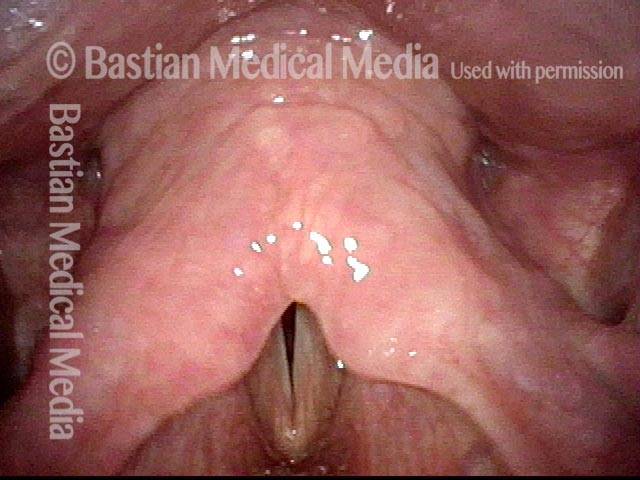
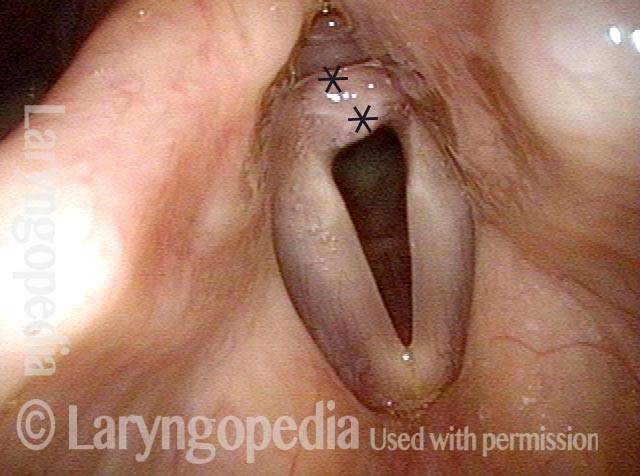
Synechia hidden by overhanging arytenoid superstructure (3 of 4)
Close-up view of the posterior vocal cords reveal a synechia or scar band tethering the vocal cords to each other and preventing their abduction. This kind of injury can exist in isolation; it can also occur together with cricoarytenoid joint ankylosis.
Synechia hidden by overhanging arytenoid superstructure (3 of 4)
Close-up view of the posterior vocal cords reveal a synechia or scar band tethering the vocal cords to each other and preventing their abduction. This kind of injury can exist in isolation; it can also occur together with cricoarytenoid joint ankylosis.
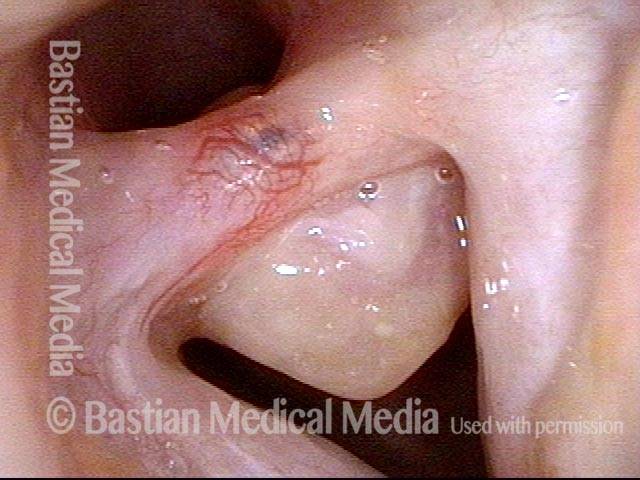
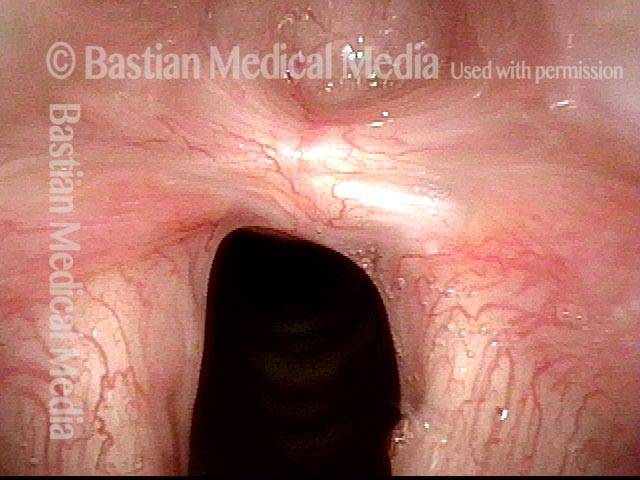
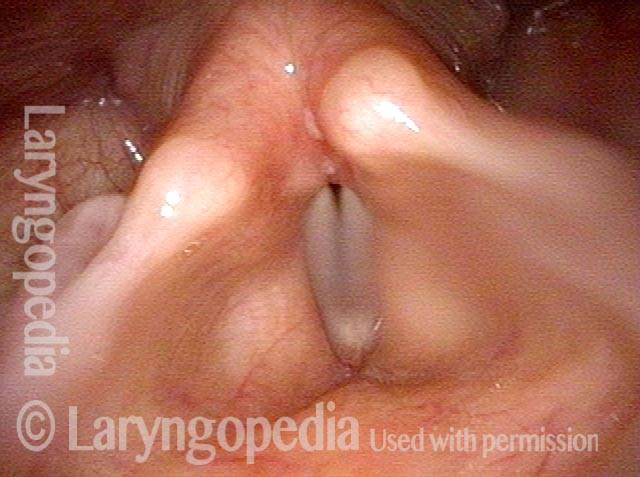
Synechia hidden by overhanging arytenoid superstructure (4 of 4)
An even closer view of the synechia.
Synechia hidden by overhanging arytenoid superstructure (4 of 4)
An even closer view of the synechia.
Nasal and Inter-arytenoid Synechiae, with Subglottic Stenosis in Forme Fruste Wegener’s
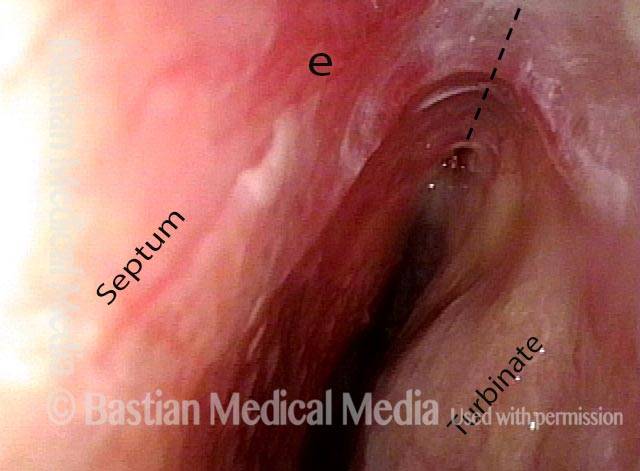
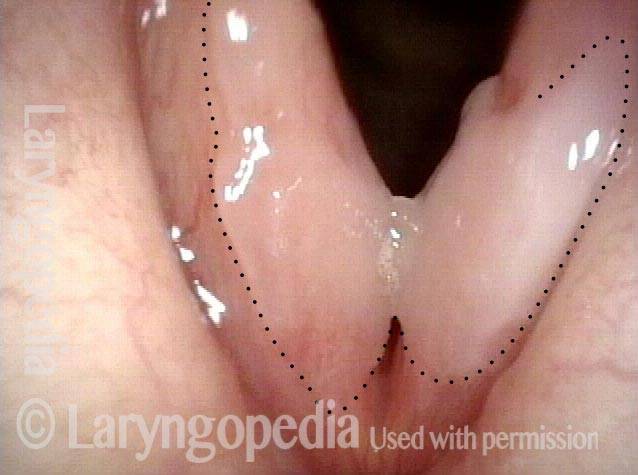
Nasal cavity (1 of 4)
View in left nasal cavity, showing inflammatory adhesion between septum and turbinate/ lateral wall of nose. Note intense erythema at “e.” Dotted line shows where normal separation would be seen.
Nasal cavity (1 of 4)
View in left nasal cavity, showing inflammatory adhesion between septum and turbinate/ lateral wall of nose. Note intense erythema at “e.” Dotted line shows where normal separation would be seen.
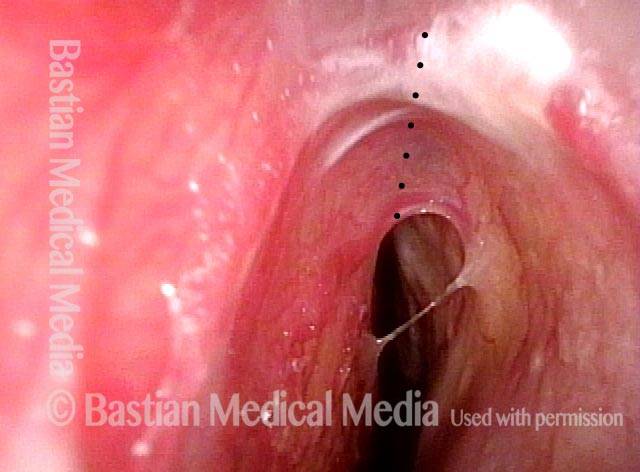
Closer view (2 of 4)
Closer, brighter view, again with dotted line where there should be no tissue bridge, but instead separation between septum and turbinates. This adhesion is asymptomatic, and therefore does not need to be treated.
Closer view (2 of 4)
Closer, brighter view, again with dotted line where there should be no tissue bridge, but instead separation between septum and turbinates. This adhesion is asymptomatic, and therefore does not need to be treated.
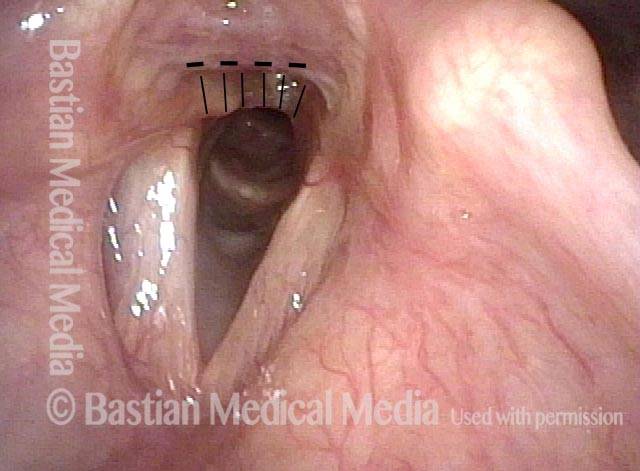
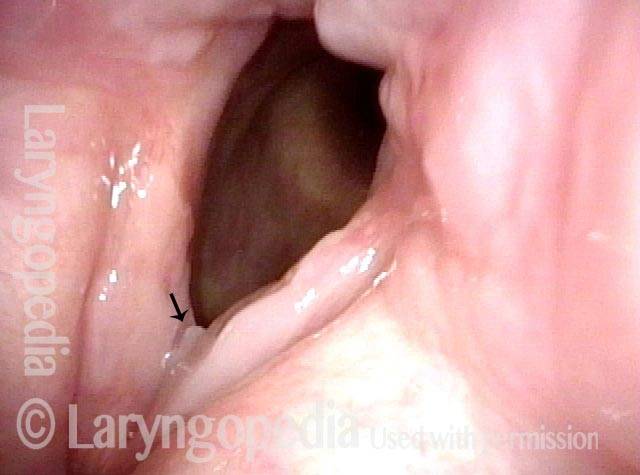
Panoramic view (3 of 4)
Panoramic view of larynx, showing adhesion between arytenoid cartilages indicated by vertical hashed lines. Horizontal dashed line is for reference with the next photo.
Panoramic view (3 of 4)
Panoramic view of larynx, showing adhesion between arytenoid cartilages indicated by vertical hashed lines. Horizontal dashed line is for reference with the next photo.
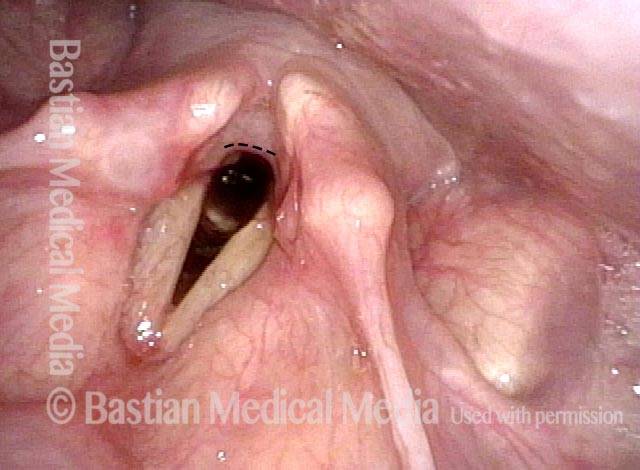
Post dilation (4 of 4)
After dilation, the interarytenoid synechia is no longer seen. Subglottic stenosis is present but not shown in this series.
Post dilation (4 of 4)
After dilation, the interarytenoid synechia is no longer seen. Subglottic stenosis is present but not shown in this series.
Ulcerative Laryngitis and Resulting Synechia – Fixed!
Synechia (1 of 3)
This woman developed a sore throat and lost her voice a week after a chemotherapy treatment for her metastatic breast cancer. Here, 6 weeks later, note the hazy area representing resolving “ulcerative” laryngitis (surrounded by tiny dotted line). There is a synechia attaching the cords together.
Synechia (1 of 3)
This woman developed a sore throat and lost her voice a week after a chemotherapy treatment for her metastatic breast cancer. Here, 6 weeks later, note the hazy area representing resolving “ulcerative” laryngitis (surrounded by tiny dotted line). There is a synechia attaching the cords together.
Attempted to detach (2 of 3)
The flexible scope has been used once to “twang upwards” from below in order to detach the cords from each other. At the arrow, slight separation can be seen.
Attempted to detach (2 of 3)
The flexible scope has been used once to “twang upwards” from below in order to detach the cords from each other. At the arrow, slight separation can be seen.
Successfully detached (3 of 3)
Just after the second attempt. That is, for the second time, the scope was passed below the cords, angulated sharply underneath the synechia, and then pulled upwards. The adhesion has been released. Voice is instantly and dramatically restored (though still hoarse, of course).
Successfully detached (3 of 3)
Just after the second attempt. That is, for the second time, the scope was passed below the cords, angulated sharply underneath the synechia, and then pulled upwards. The adhesion has been released. Voice is instantly and dramatically restored (though still hoarse, of course).
Posterior Commissure Synechiae
Tethered vocal cords (1 of 5)
This man has right vocal cord paralysis and a history decades ago of Teflon injection into the right vocal cord, resulting in posterior commissure synechiae. He is short of breath, partly due to the tissue band and partly because it tethers the vocal cords closer together than they would otherwise need to be as seen in photo 4 after the band is removed. See also photo 5.
Tethered vocal cords (1 of 5)
This man has right vocal cord paralysis and a history decades ago of Teflon injection into the right vocal cord, resulting in posterior commissure synechiae. He is short of breath, partly due to the tissue band and partly because it tethers the vocal cords closer together than they would otherwise need to be as seen in photo 4 after the band is removed. See also photo 5.
Before laser removal (3 of 5)
The thulium laser fiber (F) is touching the synechiae, with laser energy about to be delivered.
Before laser removal (3 of 5)
The thulium laser fiber (F) is touching the synechiae, with laser energy about to be delivered.
Immediately after laser (4 of 5)
This is just after the thulium laser division of the band using topical anesthesia only, with patient sitting in a chair.
Immediately after laser (4 of 5)
This is just after the thulium laser division of the band using topical anesthesia only, with patient sitting in a chair.
One month post-op (5 of 5)
A month later, no residue of the synechiae is seen, and the vocal cords can spring farther apart than in photo 1.
One month post-op (5 of 5)
A month later, no residue of the synechiae is seen, and the vocal cords can spring farther apart than in photo 1.
Difficulty Breathing After A 3-day Intubation
Noisy, restricted breathing following intubation (1 of 5)
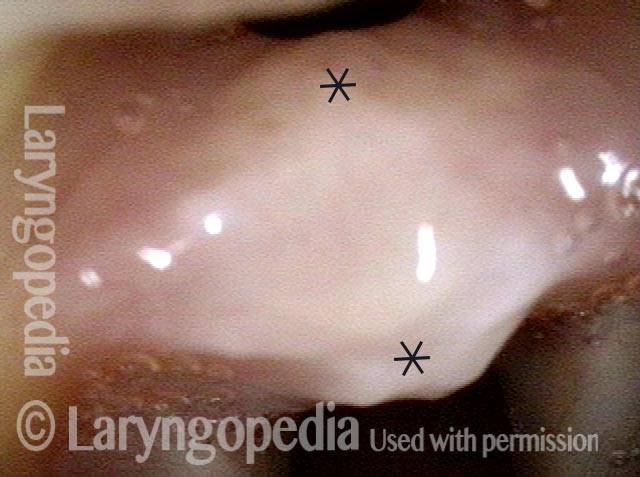
This teenager was intubated for 3 days due to tongue swelling. Breathing became noisy and restricted approximately 6 weeks later. Note that the vocal cords do not abduct fully and there is what appears to be granulation tissue at the posterior commissure (anterior asterisk).
Noisy, restricted breathing following intubation (1 of 5)
This teenager was intubated for 3 days due to tongue swelling. Breathing became noisy and restricted approximately 6 weeks later. Note that the vocal cords do not abduct fully and there is what appears to be granulation tissue at the posterior commissure (anterior asterisk).
Normal voice (2 of 5)
The vocal cords can come into contact as shown here, consistent with her normal-sounding voice.
Normal voice (2 of 5)
The vocal cords can come into contact as shown here, consistent with her normal-sounding voice.
At close range (3 of 5)
At very close range within the posterior commissure, a small tract is seen posterior to the “granulation” which is now seen more clearly to be a broad-based synechiae with asterisks marking anterior and posterior limits.
At close range (3 of 5)
At very close range within the posterior commissure, a small tract is seen posterior to the “granulation” which is now seen more clearly to be a broad-based synechiae with asterisks marking anterior and posterior limits.
At even closer range (4 of 5)
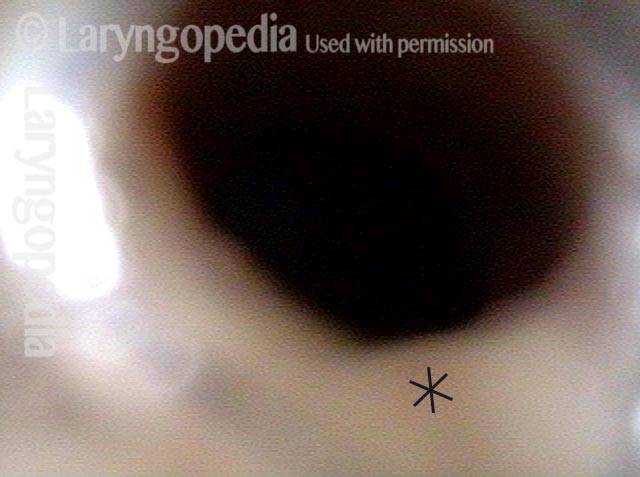
An even closer view verifies a posterior tract, and this makes it less likely that the cricoarytenoid joints are also injured.
At even closer range (4 of 5)
An even closer view verifies a posterior tract, and this makes it less likely that the cricoarytenoid joints are also injured.
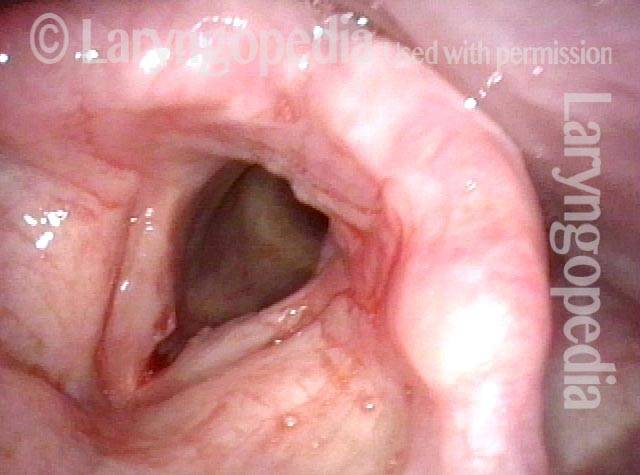
Mucosa-only scar (5 of 5)
This view is taken with the scope passed just between the vocal cords and just anterior to the synechiae and angled directly posteriorly. A small superficial-looking “mucosa-only” scar is seen bilaterally, surrounded by dotted line. It can be confidently predicted that when the synechiae is released, the arytenoid cartilages will likely be able to abduct fully.
Mucosa-only scar (5 of 5)
This view is taken with the scope passed just between the vocal cords and just anterior to the synechiae and angled directly posteriorly. A small superficial-looking “mucosa-only” scar is seen bilaterally, surrounded by dotted line. It can be confidently predicted that when the synechiae is released, the arytenoid cartilages will likely be able to abduct fully.
Breathing Tube Injury: Synechiae
Breathing Tube Injury (1 of 4)
Some weeks after a 3-day intubation for a nonorganic breathing problem, some ongoing (and different) breathing symptoms are caused by a synechiae that will not permit full abduction of the vocal cords. The * allows comparison with photo 2.
Breathing Tube Injury (1 of 4)
Some weeks after a 3-day intubation for a nonorganic breathing problem, some ongoing (and different) breathing symptoms are caused by a synechiae that will not permit full abduction of the vocal cords. The * allows comparison with photo 2.
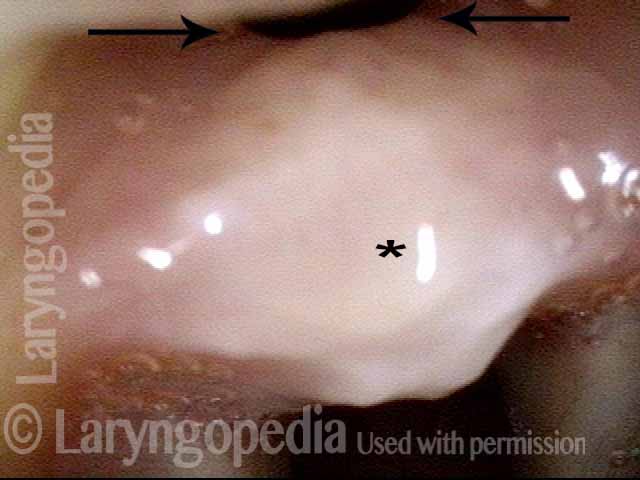
Post-intubation synechiae (2 of 4)
Extremely close visualization of the post-intubation synechiae (* to orient with photo 1). Note the opening posterior to the synechiae indicated by the arrows. This makes it less likely that there is a concomitant ankylosis (fixation) of either cricoarytenoid joint.
Post-intubation synechiae (2 of 4)
Extremely close visualization of the post-intubation synechiae (* to orient with photo 1). Note the opening posterior to the synechiae indicated by the arrows. This makes it less likely that there is a concomitant ankylosis (fixation) of either cricoarytenoid joint.
Breathing Tube Injury (3 of 4)
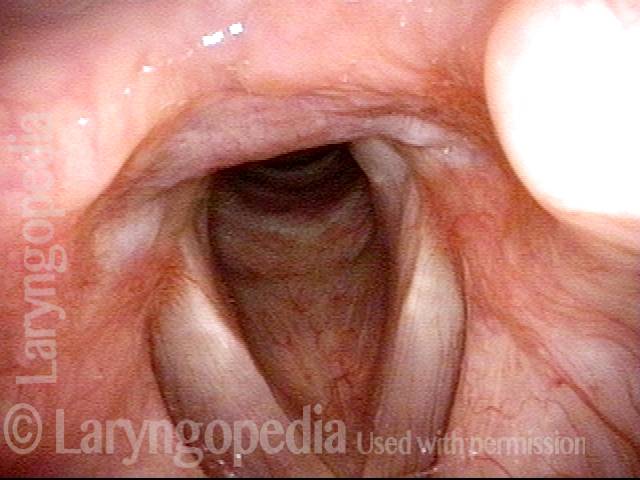
Several months after surgical release of the synechiae, notice that abduction of the vocal cords again makes a normal, wide-open “v.” Compare with photo 1 to see this clearly.
Breathing Tube Injury (3 of 4)
Several months after surgical release of the synechiae, notice that abduction of the vocal cords again makes a normal, wide-open “v.” Compare with photo 1 to see this clearly.
Breathing Tube Injury (4 of 4)
Closer visualization of the posterior commissure shows evidence of scar at the left base of the synechia. This could be easily overlooked if the patient’s history were not known.
Breathing Tube Injury (4 of 4)
Closer visualization of the posterior commissure shows evidence of scar at the left base of the synechia. This could be easily overlooked if the patient’s history were not known.
Play Video
Vocal Cord Synechia
Vocal cord synechia is a condition wherein a scar band tethers the vocal cords to each other. Therefore, the vocal cords cannot fully open for breathing. This video provides a clear example — using laryngeal videostroboscopy — of a vocal cord synechia.
Table of Contents
Tagged Airway disorders, Disorders, Photos, Videos