Idiopathic Subglottic Stenosis (Inflammatory Stenosis)
Idiopathic (unknown cause) subglottic stenosis is narrowing in a lumen or passageway caused by an inflammatory process. It is a frustrating breathing problem seen mostly in women. It appears to be an autoimmune disorder that we have thought for many years to be an incomplete expression (forme fruste) of Wegener’s Granulomatosis, aka Granulomatosis with Polyangiitis (GPA).
Treatment
In a caseload of perhaps 125 patients, it appears that standard of care remains occasional outpatient dilation, steroid injection, and mitomycin C application. Most patients go a year or more between dilations.
The rub: occasionally, dilations need to be done more frequently in an “active” case, or there may be reasons to avoid the brief general anesthesia required for dilation such as: morbid obesity, difficult jaw/tooth/neck anatomy, or even a phobia of general anesthesia.
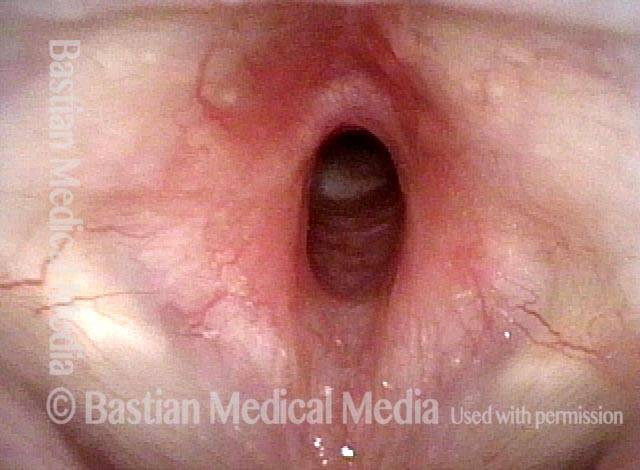
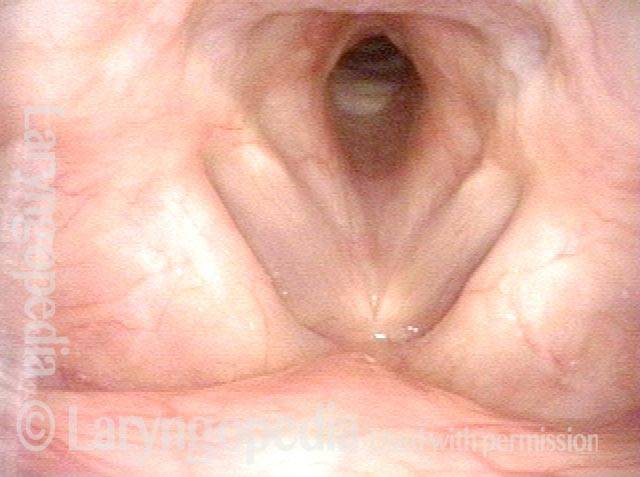
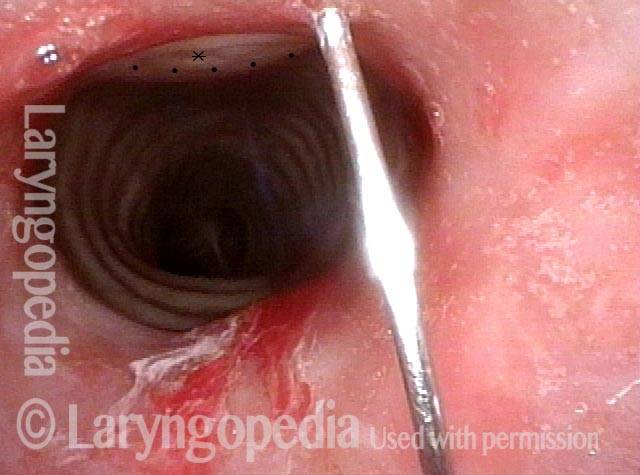
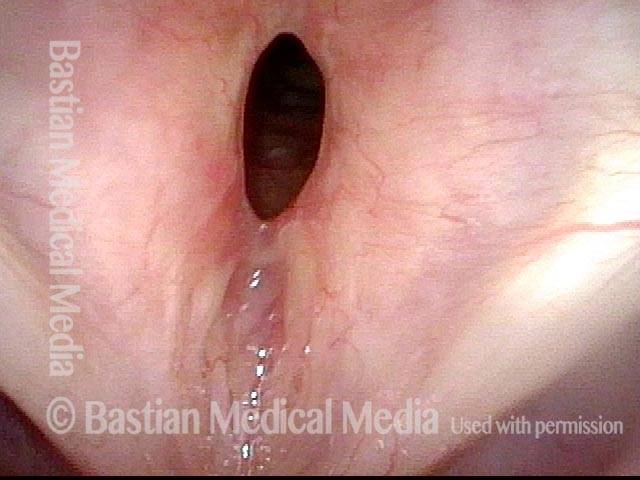
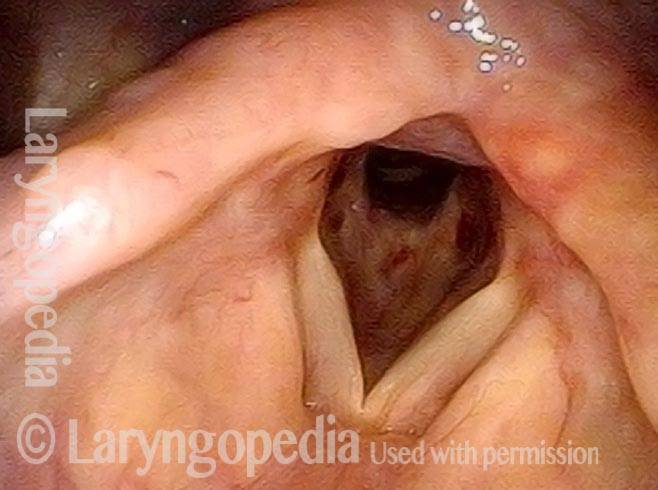
Rheumatoid arthritis (1 of 4)
Rheumatoid arthritis (1 of 4)
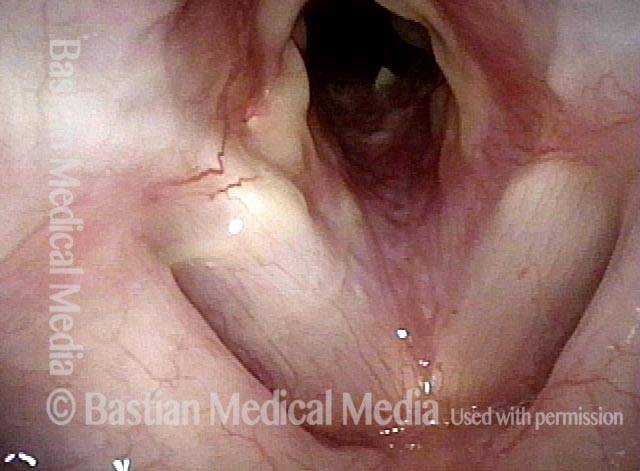
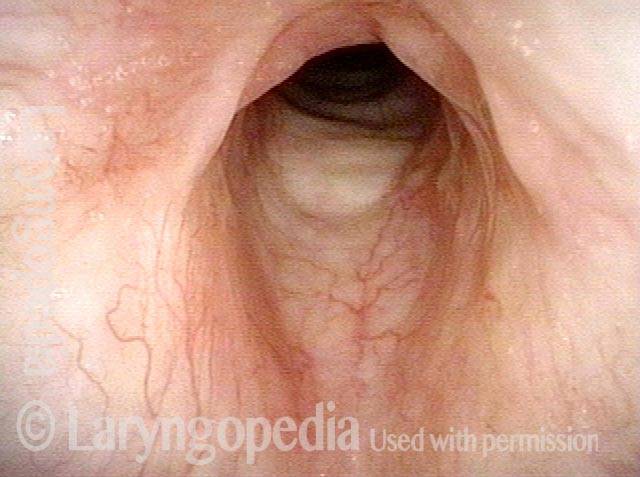
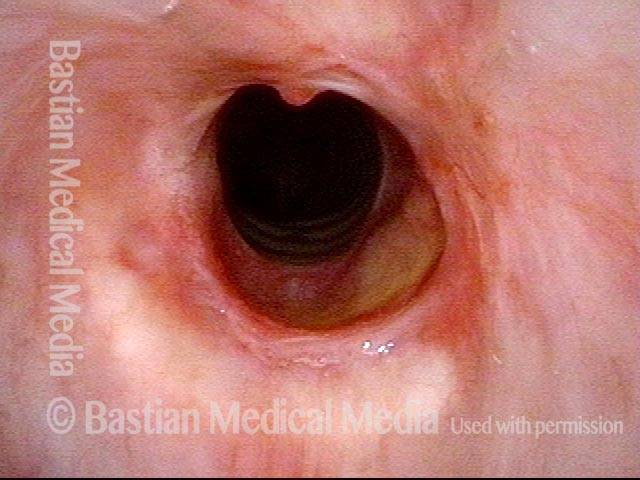
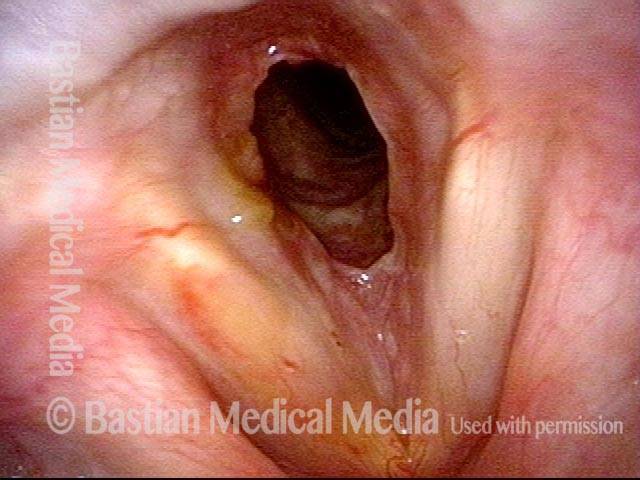
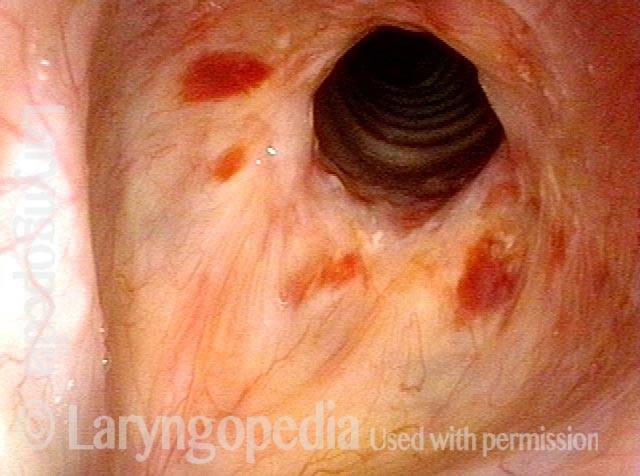
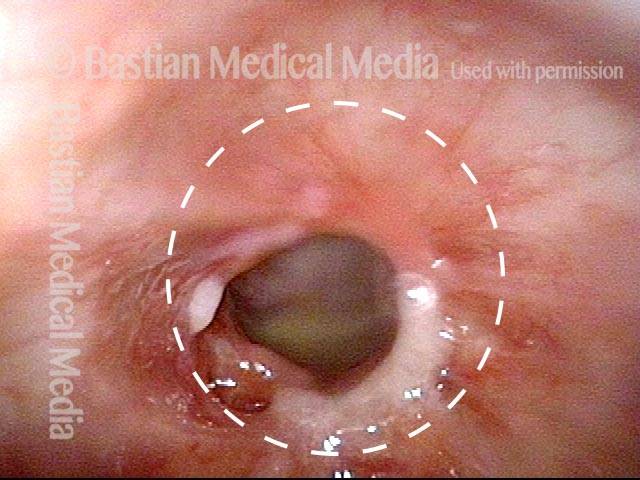
Inflammatory subglottic stenosis (2 of 4)
Inflammatory subglottic stenosis (2 of 4)
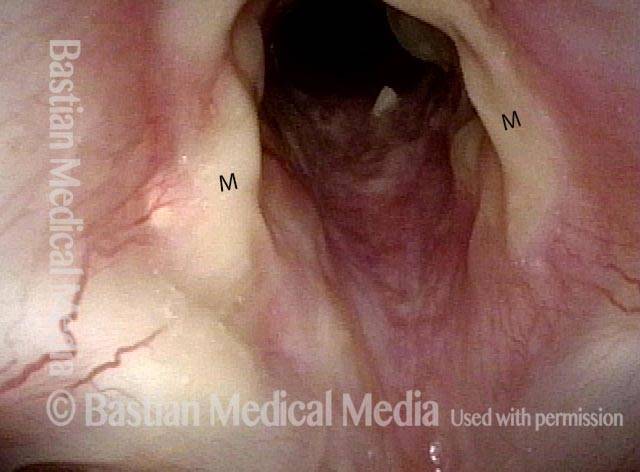
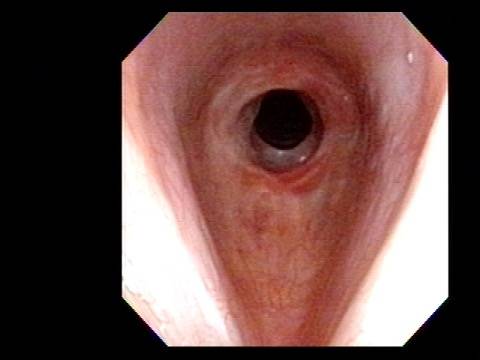
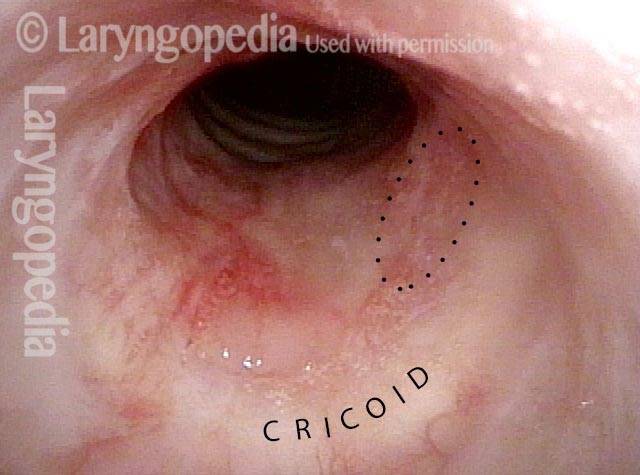
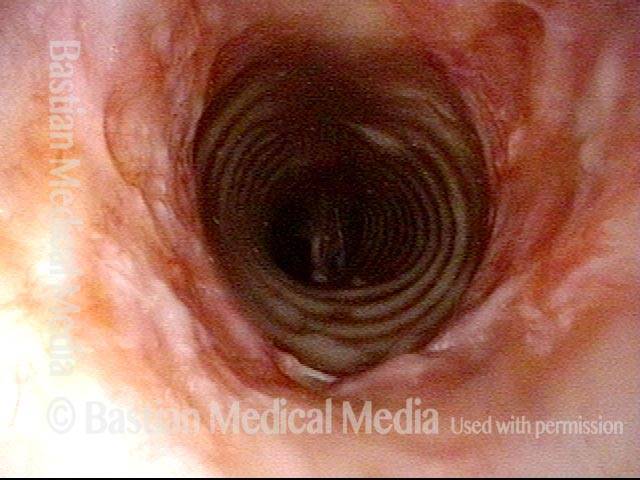
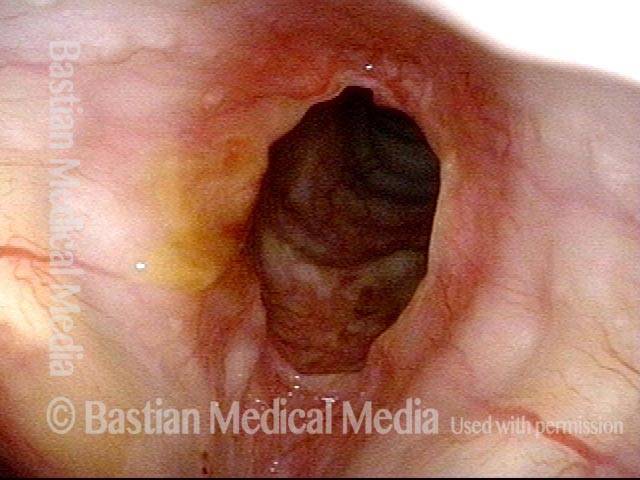
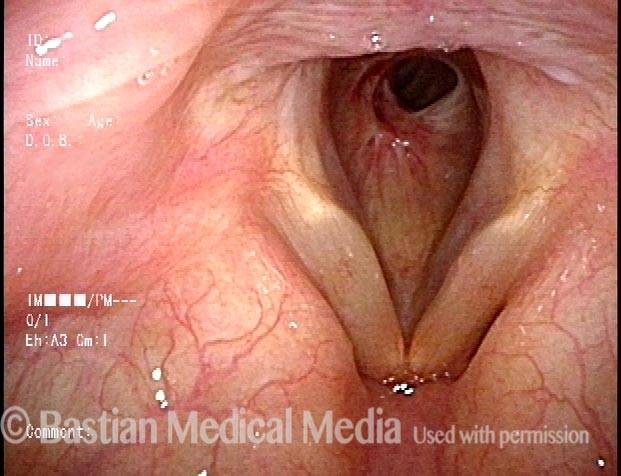
One week after dilation (3 of 4)
One week after dilation (3 of 4)
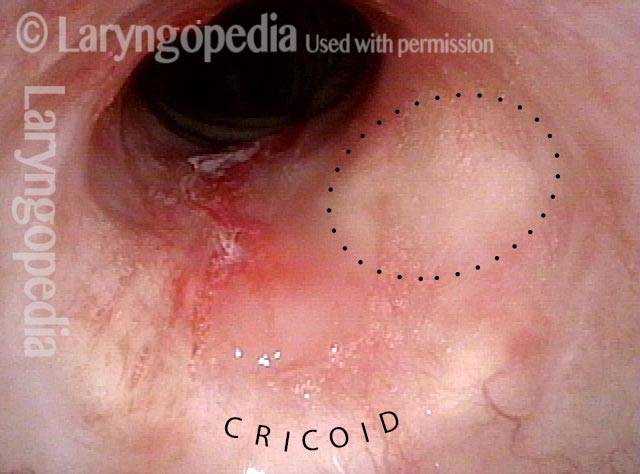
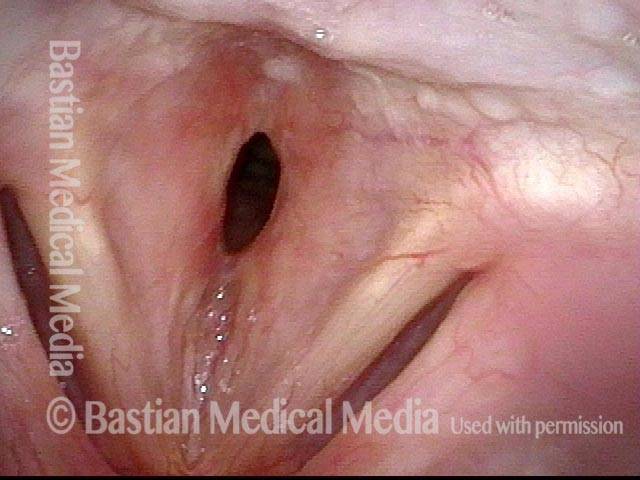
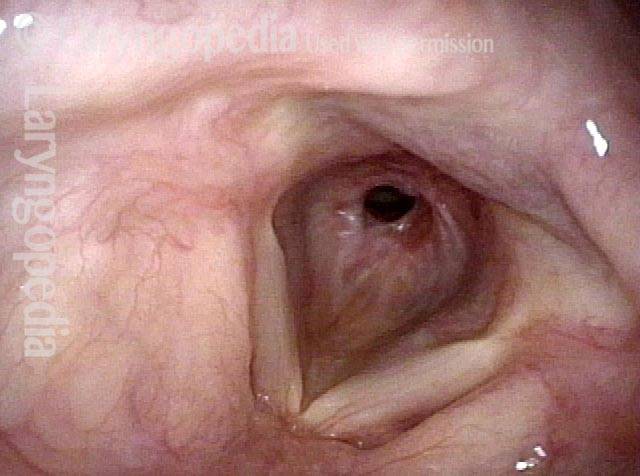
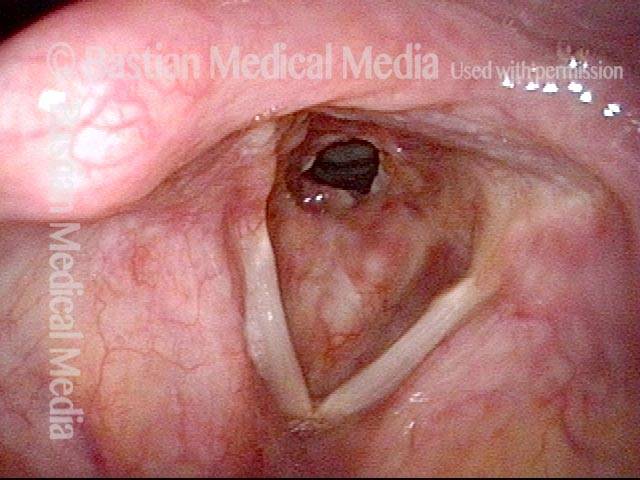
Mucus (4 of 4)
Mucus (4 of 4)
“Office” Treatment Option for Inflammatory Subglottic Stenosis
In such situations, one naturally casts about for alternatives. Low dose methotrexate has not been very effective in our experience. And we work with a motivated rheumatologist open to considering rituximab, even with a negative ANCA study. Or the laryngologist might consider an office-based airway procedure as illustrated in the photos below. This particular person only requires dilation every 18 months or so, but it represents a major stressor for her given her fears, her size, and somewhat challenging anatomy. She is one of several offered the treatment shown below: steroid injection in the voice laboratory, followed by laser treatment.
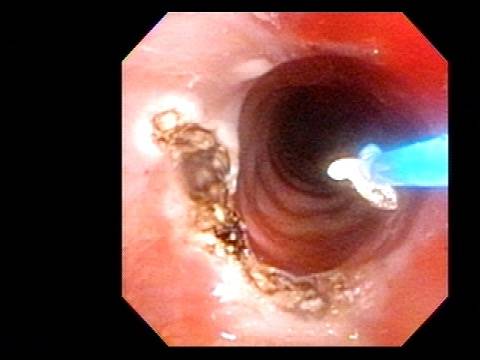
Our thought is that in some, it may be the ridges and air turbulence that creates the feeling of airway restriction, or that these rings of stenosis “catch” mucus. In the case below, the clinician was almost dubious that what was accomplished would make that much difference to the person’s breathing. But upon calling her a week after the procedure below, and asking if the improvement was nil, subtle, small, medium, or large, she replied “large…a huge improvement.”
60% Stenosis (1 of 5)
60% Stenosis (1 of 5)
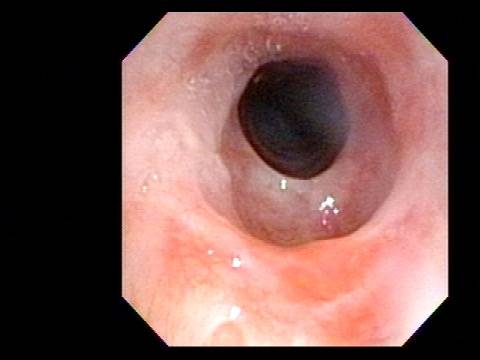
Narrowing & erythema (2 of 5)
Narrowing & erythema (2 of 5)
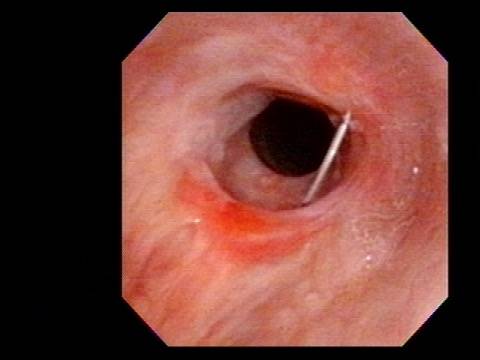
Triamcinolone is injected (3 of 5)
Triamcinolone is injected (3 of 5)
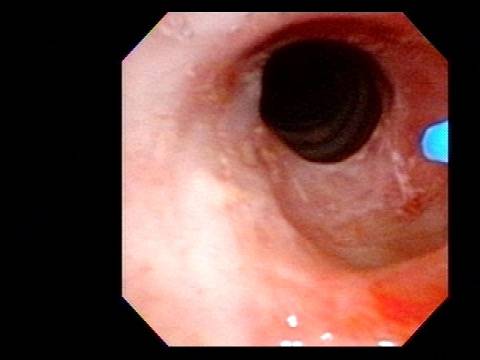
Laser ablation (4 of 5)
Laser ablation (4 of 5)
Stenosis is coagulated (5 of 5)
Stenosis is coagulated (5 of 5)
Idiopathic Subglottic Stenosis Has Different Levels
Post dilation (1 of 4)
Post dilation (1 of 4)
Closer view (2 of 4)
Closer view (2 of 4)
Rich vascular pattern (3 of 4)
Rich vascular pattern (3 of 4)
“Sharing” the airway (4 of 4)
“Sharing” the airway (4 of 4)
Another way to Inject Idiopathic Subglottic Stenosis
Idiopathic inflammatory subglottic stenosis (1 of 3)
Idiopathic inflammatory subglottic stenosis (1 of 3)
Priot to injection (2 of 3)
Priot to injection (2 of 3)
Injection (3 of 3)
Injection (3 of 3)
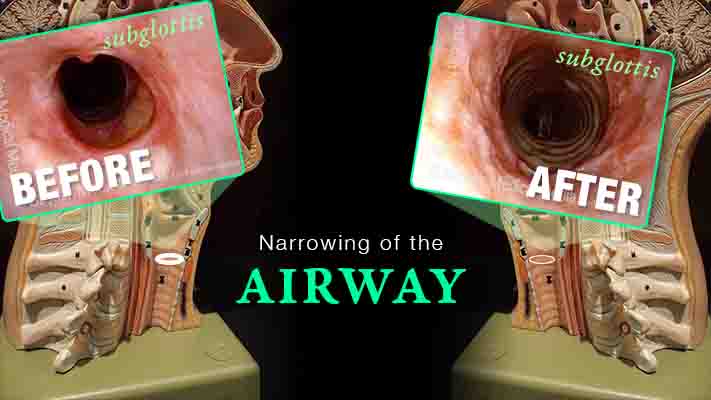
Subglottic Stenosis, after Treatment
Subglottic stenosis, before treatment (1 of 2)
Subglottic stenosis, before treatment (1 of 2)
Subglottic stenosis, after treatment (2 of 2)
Subglottic stenosis, after treatment (2 of 2)
Subglottic Stenosis, before and after Dilation
Subglottic stenosis, before dilation (1 of 2)
Subglottic stenosis, before dilation (1 of 2)
Subglottic stenosis, after dilation (2 of 2)
Subglottic stenosis, after dilation (2 of 2)
Example 2
Subglottic stenosis (1 of 5)
Subglottic stenosis (1 of 5)
Subglottic stenosis, worsened (2 of 5)
Subglottic stenosis, worsened (2 of 5)
Subglottic stenosis, worsened (3 of 5)
Subglottic stenosis, worsened (3 of 5)
Subglottic stenosis, after dilation (4 of 5)
Subglottic stenosis, after dilation (4 of 5)
Subglottic stenosis, after dilation (5 of 5)
Subglottic stenosis, after dilation (5 of 5)
Stenosis Before and After Dilation for Forme Fruste Wegener’s
Subglottic stenosis (1 of 5)
Subglottic stenosis (1 of 5)
Inflammation (2 of 5)
Inflammation (2 of 5)
Flexible scope (3 of 5)
Flexible scope (3 of 5)
Post-dilation (4 of 5)
Post-dilation (4 of 5)
Post-operative bruising (5 of 5)
Post-operative bruising (5 of 5)
Subglottic / Tracheal Stenosis
Wegener’s granulomatosis (1 of 4)
Wegener’s granulomatosis (1 of 4)
Subglottic / Tracheal stenosis (2 of 4)
Subglottic / Tracheal stenosis (2 of 4)
Subglottic / Tracheal stenosis (3 of 4)
Subglottic / Tracheal stenosis (3 of 4)
Inflammed Stenosis (4 of 4)
Inflammed Stenosis (4 of 4)
Subglottic Stenosis, Due to Wegener’s Granulomatosis
Subglottic stenosis, due to Wegener’s (1 of 2)
Subglottic stenosis, due to Wegener’s (1 of 2)
Subglottic stenosis, due to Wegener’s (2 of 2)
Subglottic stenosis, due to Wegener’s (2 of 2)
Share this article
Inflammation Subglottic Stenosis
Are you experiencing gradual onset of noisy, even effortful breathing? One uncommon but important explanation is idiopathic, inflammatory subglottic stenosis. That just means “unknown cause, likely autoimmune narrowing just below the vocal cords and at the highest part of the windpipe.”
This video explains the disorder and its management, shows “before” and “after” photos, and reassures viewers that if yours is the usual case, there doesn’t seem to be any effect on general health or lifespan.