Subglottic Stenosis
Subglottic stenosis is narrowing just below the vocal cords, in the lowest part of the larynx and immediately above the first tracheal ring. Examples of causes include scarring from a breathing tube used during a long ICU stay, Wegener’s Granulomatosis (aka Granulomatosis with Polyangiitis [GPA]), and idiopathic subglottic stenosis (aka limited Wegener’s Granulomatosis).
Subglottic Stenosis, after Treatment
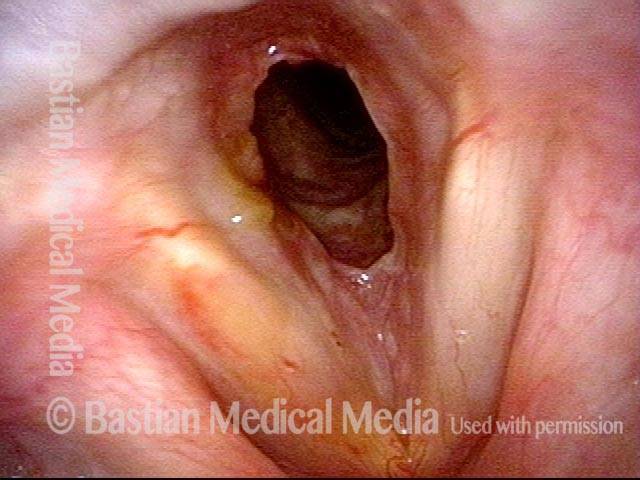
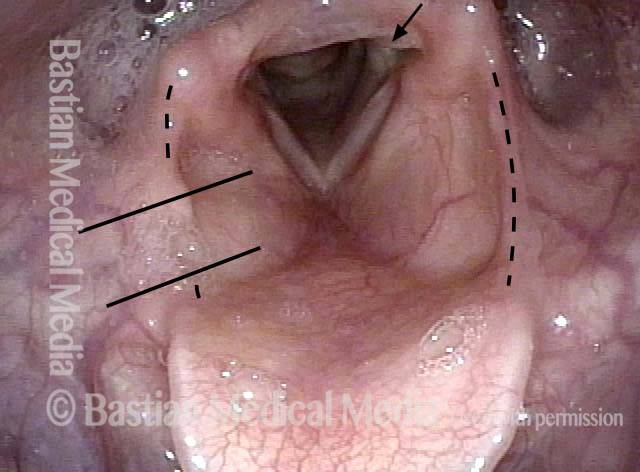
Subglottic stenosis, before treatment (1 of 2)
Subglottic stenosis, before treatment (1 of 2)
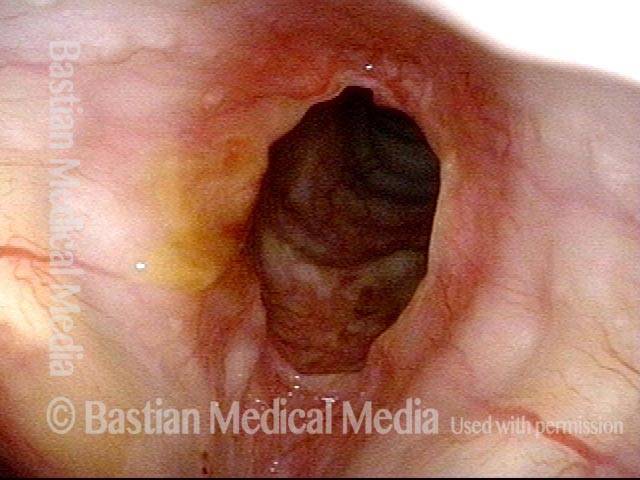
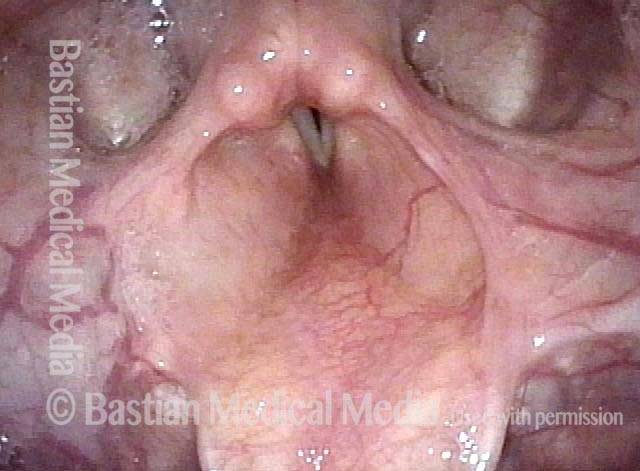
Subglottic stenosis, after treatment (2 of 2)
Subglottic stenosis, after treatment (2 of 2)
Subglottic Stenosis, before and after Dilation
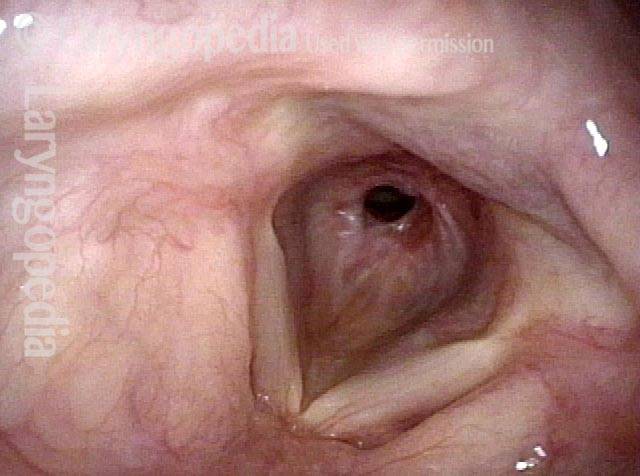
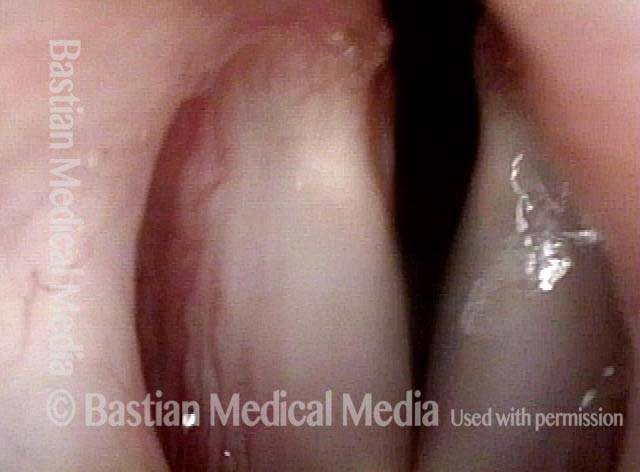
Subglottic stenosis, before dilation (1 of 2)
Subglottic stenosis, before dilation (1 of 2)
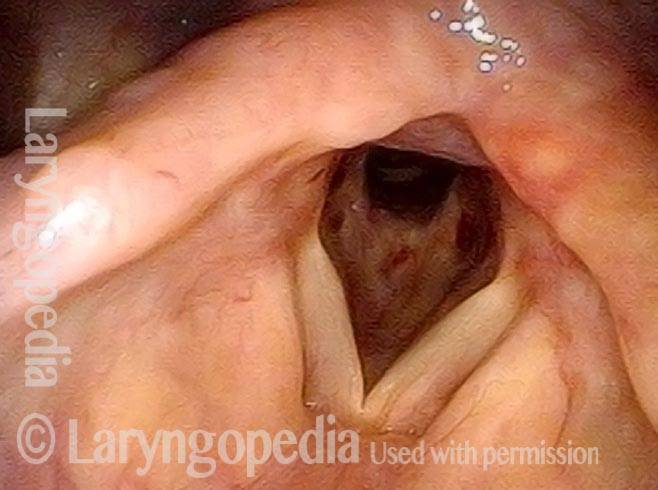
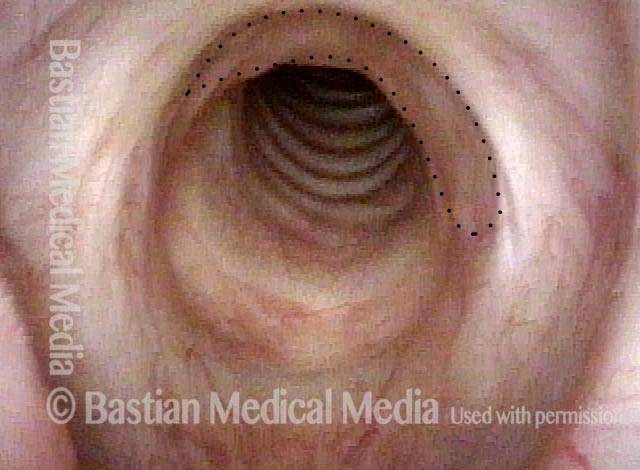
Subglottic stenosis, after dilation (2 of 2)
Subglottic stenosis, after dilation (2 of 2)
Example 2
Subglottic stenosis (1 of 5)
Subglottic stenosis (1 of 5)
Subglottic stenosis, worsened (2 of 5)
Subglottic stenosis, worsened (2 of 5)
Subglottic stenosis, worsened (3 of 5)
Subglottic stenosis, worsened (3 of 5)
Subglottic stenosis, after dilation (4 of 5)
Subglottic stenosis, after dilation (4 of 5)
Subglottic stenosis, after dilation (5 of 5)
Subglottic stenosis, after dilation (5 of 5)
Stenosis Before and After Dilation for Forme Fruste Wegener’s
Subglottic stenosis (1 of 5)
Subglottic stenosis (1 of 5)
Inflammation (2 of 5)
Inflammation (2 of 5)
Flexible scope (3 of 5)
Flexible scope (3 of 5)
Post-dilation (4 of 5)
Post-dilation (4 of 5)
Post-operative bruising (5 of 5)
Post-operative bruising (5 of 5)
Subglottic / Tracheal Stenosis
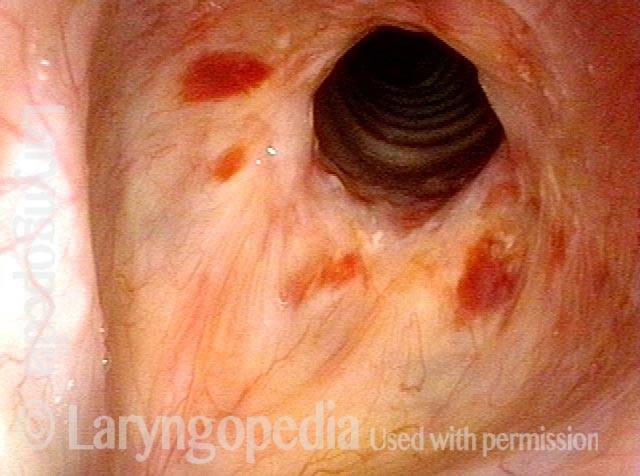
Wegener’s granulomatosis (1 of 4)
Wegener’s granulomatosis (1 of 4)
Subglottic / Tracheal stenosis (2 of 4)
Subglottic / Tracheal stenosis (2 of 4)
Subglottic / Tracheal stenosis (3 of 4)
Subglottic / Tracheal stenosis (3 of 4)
Inflammed Stenosis (4 of 4)
Inflammed Stenosis (4 of 4)
Subglottic Stenosis, Due to Wegener’s Granulomatosis
Subglottic stenosis, due to Wegener’s (1 of 2)
Subglottic stenosis, due to Wegener’s (1 of 2)
Subglottic stenosis, due to Wegener’s (2 of 2)
Subglottic stenosis, due to Wegener’s (2 of 2)
Supraglottic, Glottic, and Subglottic Endotracheal Tube Injury
Breathing tube injury (1 of 4)
Breathing tube injury (1 of 4)
Aryepiglottic cord defect (2 of 4)
Aryepiglottic cord defect (2 of 4)
Phonation (3 of 4)
Phonation (3 of 4)
Posterior subglottic thickening (4 of 4)
Posterior subglottic thickening (4 of 4)
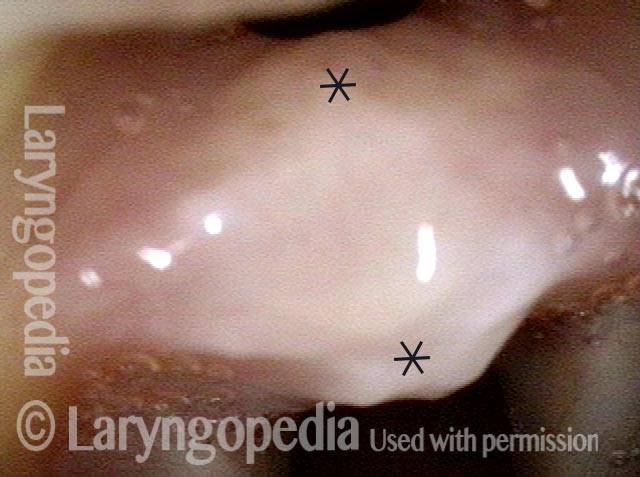
Pinhole Opening in Near-Complete Subglottic Stenosis
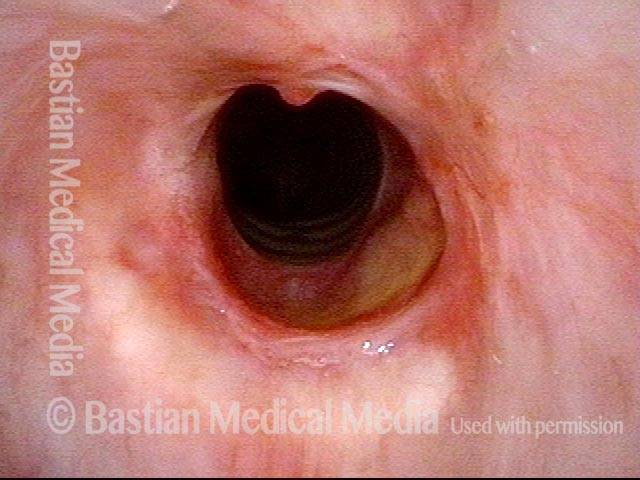
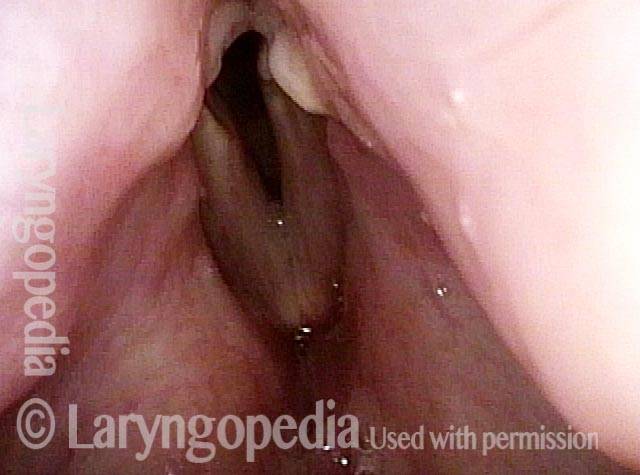
Narrowed space for breathing (1 of 4)
Narrowed space for breathing (1 of 4)
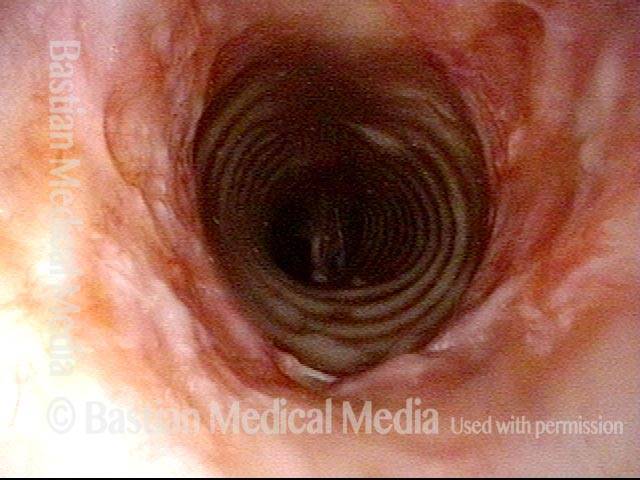
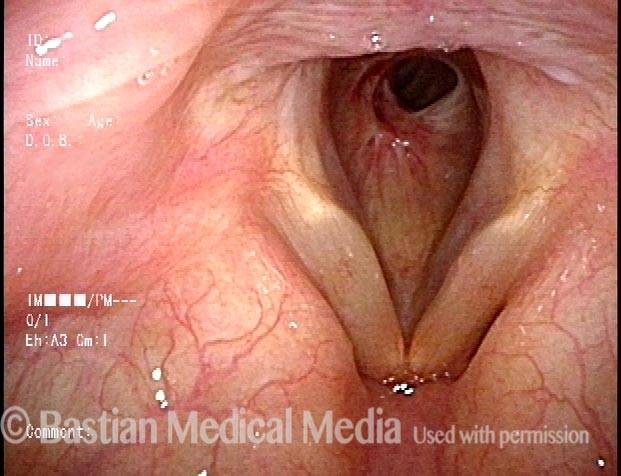
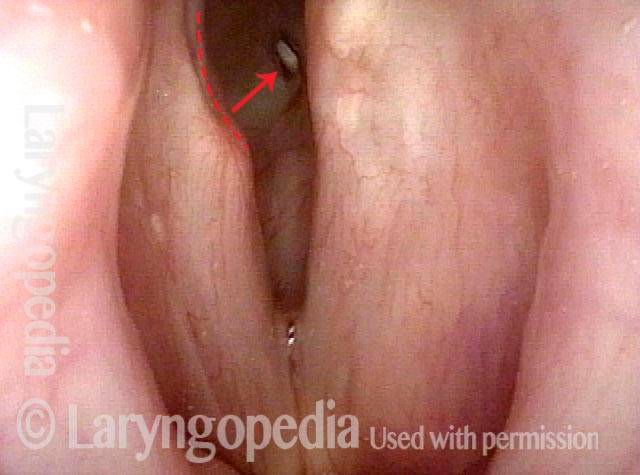
Looking between the vocal cords (2 of 4)
Looking between the vocal cords (2 of 4)
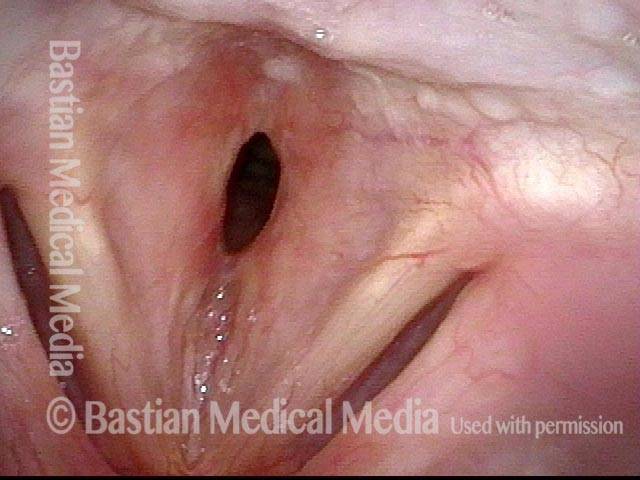
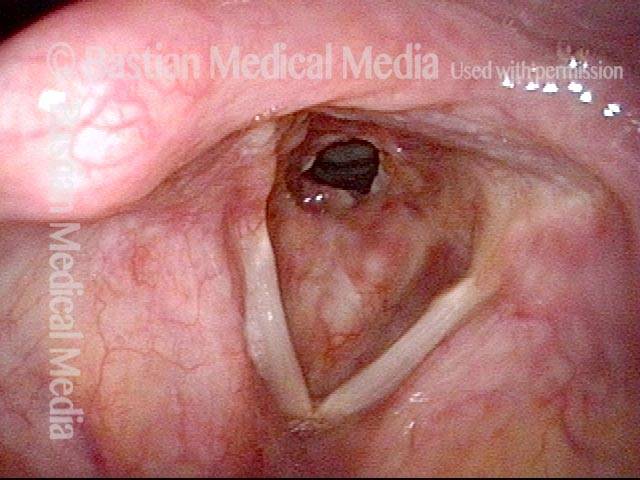
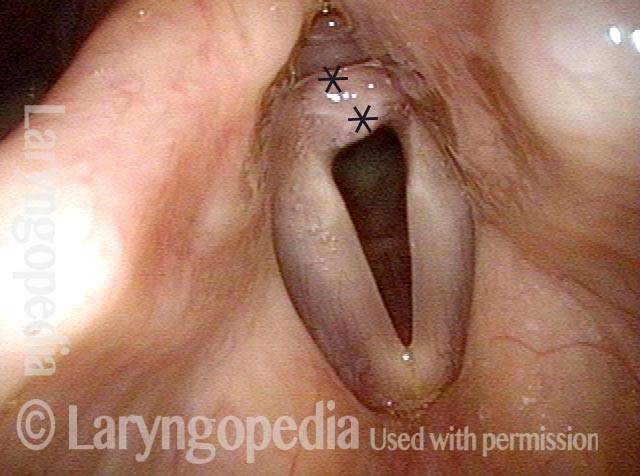
Closer view (3 of 4)
Closer view (3 of 4)
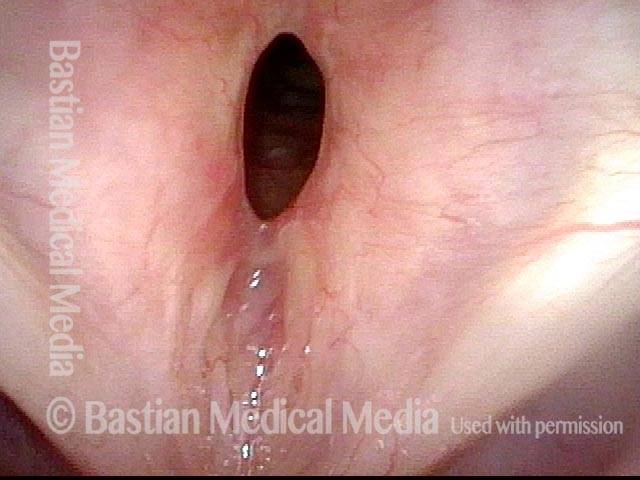
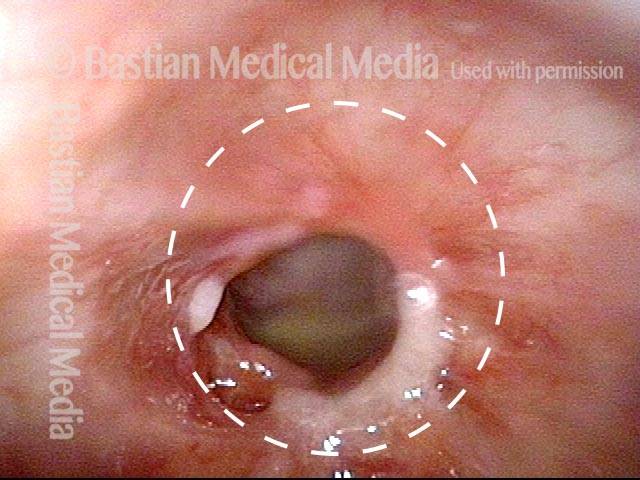
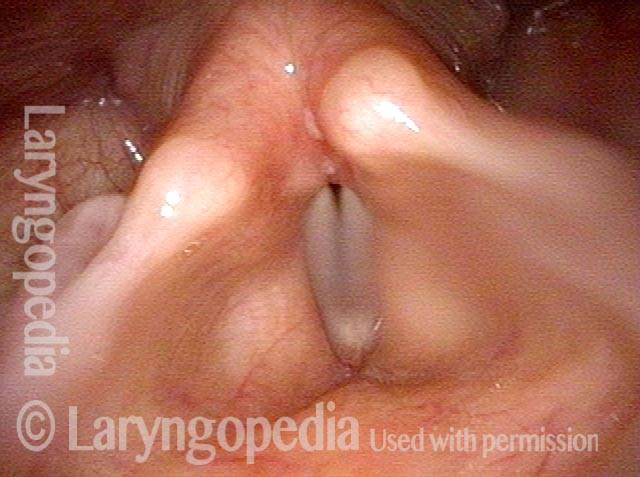
Space between subglottis and trachea (4 of 4)
Space between subglottis and trachea (4 of 4)
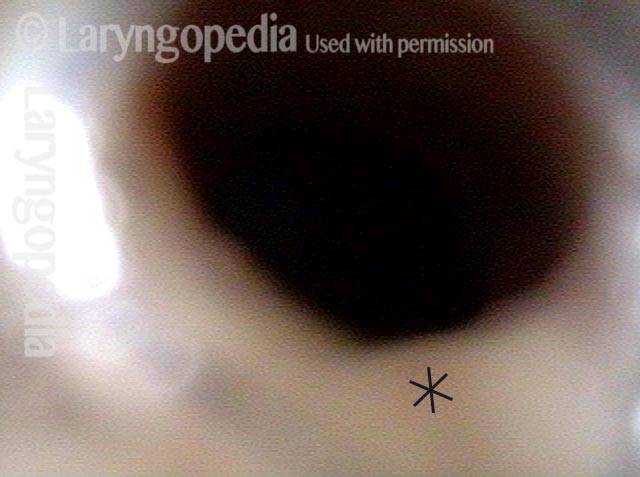
Difficulty Breathing after a 3-day Intubation
Noisy, restricted breathing following intubation (1 of 5)
Noisy, restricted breathing following intubation (1 of 5)
Normal voice (2 of 5)
Normal voice (2 of 5)
At close range (3 of 5)
At close range (3 of 5)
At even closer range (4 of 5)
At even closer range (4 of 5)
Mucosa-only scar (5 of 5)
Mucosa-only scar (5 of 5)
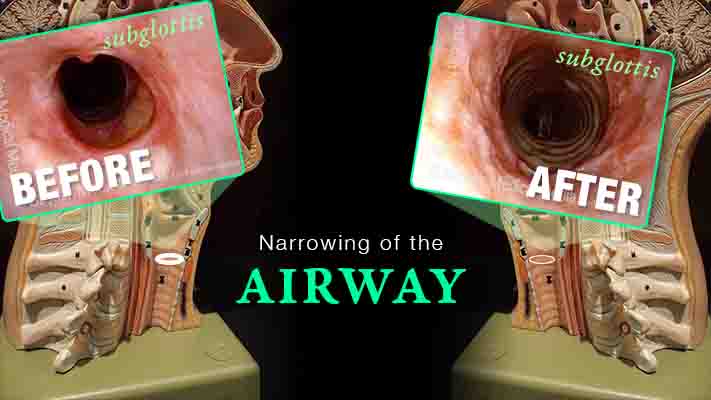
Inflammation Subglottic Stenosis – Definition, Symptoms, and Treatments
Are you experiencing gradual onset of noisy, even effortful breathing? One uncommon but important explanation is idiopathic, inflammatory subglottic stenosis. That just means “unknown cause, likely autoimmune narrowing just below the vocal cords and at the highest part of the windpipe.”
This video explains the disorder and its management, shows “before” and “after” photos, and reassures viewers that if yours is the usual case, there doesn’t seem to be any effect on general health or lifespan.
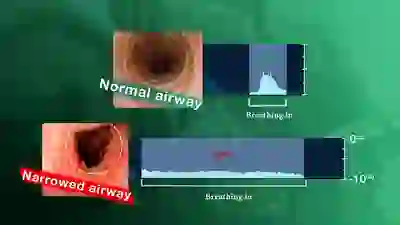
Using Your EARS to Understand Airway Narrowing
A narrowing anywhere in the breathing “pipe” that leads to the lungs causes shortness of breath, typically with harsh inspiratory noise on exertion. Such a narrowing can follow injury, intubation, cancer treatment, auto-immune disorders, etc.
It is possible to gain an immediate understanding of the magnitude of the airway narrowing within minutes by using a simple test “graded” with one’s ears. The severity of the problem can be understood before any examination or X-ray evaluation.