Early Vocal Cord Cancer: Remove with a Laser, or Radiate?
Robert W. Bastian, M.D. — Published July 31, 2014
Introduction
Patients who are diagnosed with early vocal cord cancer have two main treatment options to consider: laser surgery or radiation. There are quite a few factors to consider when weighing these two options, which can be confusing for the patient and challenging for the clinician to explain.
After 15 years of laryngology practice, I decided to create a single, codified overview on this subject, to help me teach more clearly and comprehensively when consulting with patients about this decision. Since creating that overview (which I also send home with patients as a handout), I’ve found it much easier to explain to patients the factors to consider when deciding between laser surgery and radiation to treat early vocal cord cancer. Below is that overview I created, in case it could help others who are consulting on or making this decision.
Background
Vocal cord cancer is classified according to size, location, and whether or not there is spread beyond the larynx. To simplify, the classification system for the primary tumor (site of origin) is:
- T1—very superficial, with normal mobility of the vocal cord
- T2—tumor has spread a little deeper and wider and this reduces movement of the vocal cord
- T3—the tumor replaces much of the vocal cord, and the vocal cord is fixed (immobile)
- T4—the vocal cord is not only fixed, but there is evidence of cartilage framework (voice box) invasion
This article focuses on the early vocal cord cancers, T1 and T2. The vocal cord is fairly “isolated” immunologically, so spread to lymph nodes, or to distant organs, is rare with early tumors, and the “N” (nodal) and “M” (distant metastasis) status will therefore not be included in this discussion.
The cell type of cancer in this location is virtually always squamous cell carcinoma. An alternate term, epidermoid carcinoma, is used interchangeably. These terms signify that the tumor originates from the mucosa, or surface layer of the vocal cord. The most common cause of this tumor is tobacco use. Another known cause is HPV (human papillomavirus) infection. Though controversial, some believe that chronic acid reflux from stomach up the esophagus and into the throat—outside of conscious awareness, during sleep—can be a cause as well.
Diagnosis and Workup
An extremely clear view of the tumor in a videoendoscopy room (after general head and neck examination) is usually sufficient to classify the primary tumor (see above). Given that spread outside the larynx is so rare, we in our laryngology practice do not routinely do CT or other scanning for a T1 and even T2 lesion (radiation doctors virtually always do). Biopsy to prove the diagnosis is accomplished either in the videoendoscopy procedure room using topical anesthesia, or in the operating room under general anesthesia.
Treating Cancer in General
The theoretical options for the treatment of cancer include chemotherapy, radiation therapy, and surgery. The obvious general principle when treating cancer of any organ is to match best treatment to each cancer, according to its type and whether it is early or advanced.
For example, leukemia is cancer of the blood cell-forming elements in bone marrow, but the cancerous cells circulate throughout the bloodstream as well. For this reason, neither surgery (a local and regional treatment) nor radiation (also a local and regional treatment) plays a significant role as compared with chemotherapy, which also circulates in the blood and therefore treats the entire body.
Note that some tumors are treated with a combination of surgery + radiation, or chemotherapy + radiation, etc.
Treatment of Early Vocal Cord Cancer
For early squamous cell carcinoma of the vocal cords, specifically T1 and T2 tumors, we use single modality treatment (i.e., only one mode of treatment is used rather than two or three in combination). There are two perfectly valid modes of treatment which are highly competitive options: endoscopic laser surgery, accomplished through the mouth during general anesthesia, or radiation therapy 1. A table highlighting each treatment mode’s “points of competition” for early vocal cord cancer—that is, the pros and cons of each—is presented below.
Modes of Treatment for Early Vocal Cord Cancer
| Point of Competition | Radiation | Laser Surgery |
|---|---|---|
| 1. Cure Rate with Initial Single-Modality Treatment (Failure of first treatment does not imply that the tumor will win, but only that you will need a second treatment modality.) | Approximately 85% “cure.” The remaining 15% need more treatment. See also #7 below. | Approximately 85% “cure.” The remaining 15% need more treatment. See also #7 below. |
| 2. Convenience | Approximately 30 visits to the radiation therapy facility | One outpatient surgical procedure under general anesthesia, or, uncommonly, two |
| 3. Early Side Effects | Little to none for two weeks, then skin of neck goes from pink to red to somewhat tanned; the inside of the throat becomes sore. There may be a period of radiation laryngitis lasting a month or so, as well as a sore throat when swallowing. You may lose some weight due to swallowing discomfort. | Sore throat from the laser surgery, typically for a few days following the procedure. Voice may be quite weak for a few weeks until healing is established. Approximately one in ten patients develop exuberant “proud flesh” healing response, which delays voice recovery, but does not change final result. |
| 4. Later Untoward Consequences, Potentially Permanent | 1) Persistent throat dryness. 2) A rare progressive fibrosis—what we call a “leatherization” process that makes tissues stiff, and voice progressively harder to produce, usually starting several years after radiotherapy was completed. 3) A rare stenosis where raw surfaces—either vocal cords, or upper esophagus—stick together, causing poor voice or swallowing difficulty. May be treated successfully, however. 4) A radiation-induced malignancy called sarcoma. It occurs rarely, many years after treatment is complete. | None, other than (for some, not all) persistent huskiness that is usually less than that caused by the tumor itself. |
| 5. Cost | An estimated five times the cost of surgery | An estimated one-fifth the cost of radiation |
| 6. Voice Result | Usually quite good after recovery from radiotherapy. Most voices a little deeper in pitch, and “drier.” | After healing, the typical voice result rivals that achieved with radiotherapy, provided not more than one-third of the bulk of the cord is removed. In those with larger resections, an implant can be placed to improve voice. |
| 7. Implications of Treatment Failure | Since radiation therapy cannot be repeated, the second treatment is necessarily some form of surgery: endoscopic laser or partial laryngectomy, or, rarely, even total laryngectomy. | All surgery options, including a second laser excision, remain. So does radiation therapy. |
Before and After Images of Surgical Treatment
Before and After Images of Radiation Treatment
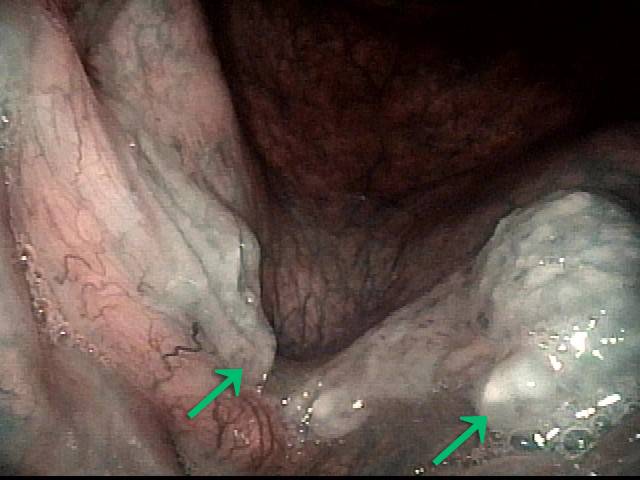
Laser Removal of Vocal Cord Cancer with Bilateral Disease
For treatment of early vocal cord cancer, both laser excision and radiotherapy are in competition as good treatment modalities. Often, radiation is used when disease is bilateral, in the interest of preserving voice. This is an example of the ability to do fairly extensive laser surgery bilaterally, yet preserving good voice. This man had a friend who had severe difficulty with radiation, and he was therefore opposed to that option.
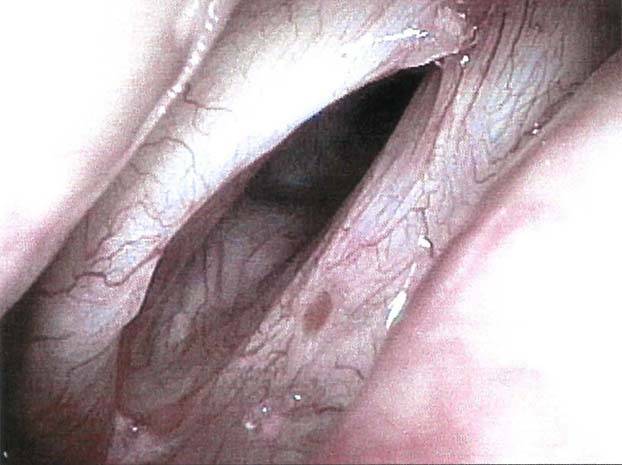
Vocal cord cancer (1 of 10)
Vocal cord cancer (1 of 10)
Stippling (2 of 10)
Stippling (2 of 10)
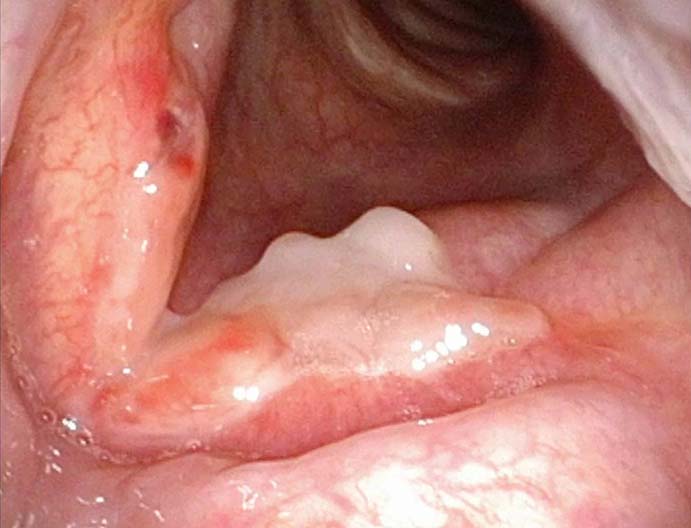
1 week after excision (3 of 10)
1 week after excision (3 of 10)
Reparative Granuloma emerges (4 of 10)
Reparative Granuloma emerges (4 of 10)
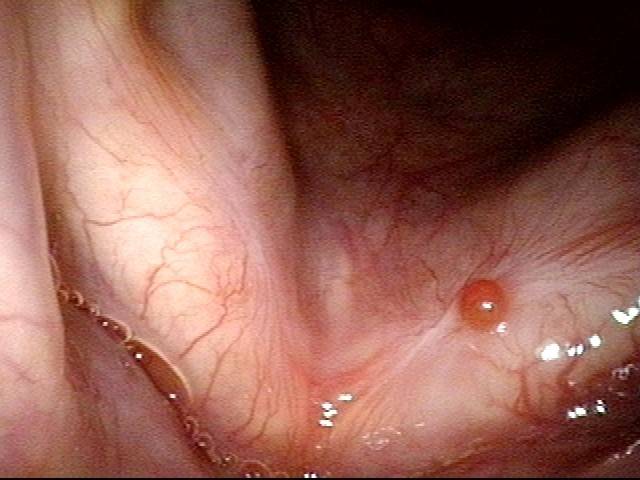
Granuloma interferes with voicing (5 of 10)
Granuloma interferes with voicing (5 of 10)
Granuloma fades away (6 of 10)
Granuloma fades away (6 of 10)
Closer view (7 of 10)
Closer view (7 of 10)
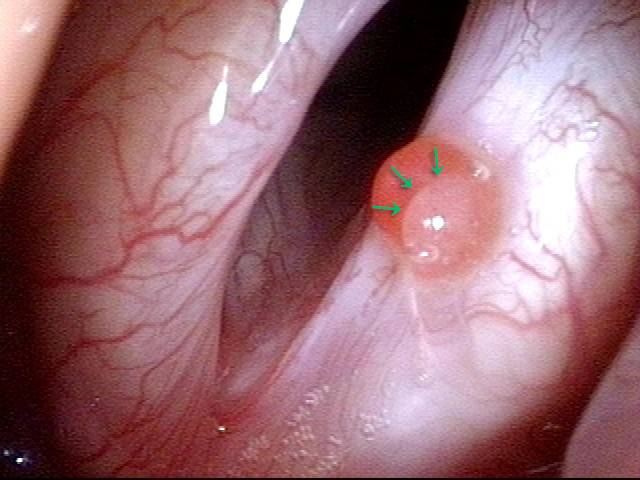
Granuloma cleft (8 of 10)
Granuloma cleft (8 of 10)
Blood tattoo (9 of 10)
Blood tattoo (9 of 10)
Voice is improved (10 of 10)
Voice is improved (10 of 10)
Share this article

Early Vocal Cord Cancer Introduction and Treatment Options
This video provides an introduction to early vocal cord cancer (stages 1 and 2) and compares the two main treatment options, laser surgery and radiation therapy.
What if I have not had a biopsy but you are suspecting tumor?
Most often, we do the biopsy in the videoendoscopy procedure room, using topical anesthesia. You can drive yourself to the appointment and home unless, by your request, you were supplied with an oral sedative to take before the biopsy procedure. In that case, you would need a driver. The biopsy can also be done under general anesthesia in the operating room.
What is involved, if I decide to opt for laser treatment?
This procedure is called microlaryngoscopy, and is most often accomplished in a day surgery center. While you are completely asleep, a hollow, lighted tube is placed on the back of the tongue to see your vocal cords directly. Bright light, magnification, and special instruments along with a laser allow removal of the disease with a narrow margin of normal tissue.
What are the risks or pitfalls of surgery?
- General anesthesia. Depending on your medical issues, general anesthesia is extraordinarily safe. It is probably statistically more dangerous to drive home from a visit to the doctor. If you have significant medical conditions, the risk may be increased.
- Dental injury. In order to visualize the vocal cords, we rest the laryngoscope on a tooth guard that covers your upper teeth. Even so, there is a small chance of a chipped, scratched, or even dislodged tooth. Weak or missing teeth and other anatomical characteristics may increase one person’s risk over another’s, but again, overall, the risk is very low.
- Abnormal voice. Initial post-surgical voice is expected to be weak, but gains strength steadily with healing. The final voice achieved is usually better than before the tumor was removed. About 10% of persons develop a temporary granuloma, or “proud flesh” healing response. Such individuals may say the voice was improving steadily for the first couple of weeks, and then began to get worse again. On examination, we may see a pink sphere of granulation tissue. This does not require biopsy. We occasionally treat the granuloma with steroids or office laser, but more typically just wait 1-4 months, by which time it usually falls off. Until it falls off, the voice may remain hoarse.
- Need for radiotherapy, in spite of surgical attempt at removal. This happens if the surgeon is unable to see or remove all of the tumor, usually due to difficult anatomy or occasionally because the tumor was larger than expected.
What does radiation therapy involve?
A consultation with a radiation oncologist is the best source of this information, but to summarize, during the typical treatment course, radiation is delivered in approximately 30 fractions, one per day from Monday through Friday, with Saturday and Sunday off. The entire course of radiation therapy usually spans six weeks.
If you suspect strongly that I have an early vocal cord cancer, do I have to undergo initial biopsy? Why not just remove the lesion?
We like that question. In fact, particularly when the lesion is small, and when the person is certain he or she would choose laser surgery over radiation therapy, we may go to the operating room in order to accomplish BOTH diagnostic biopsy AND definitive treatment in one step.
This requires that we educate the person extensively as we have in this article about the entire subject of early vocal cord carcinoma even before we have proof of the diagnosis. If it is larger, we might do an initial biopsy in our videoendoscopy room. We can also take a biopsy in the operating room with frozen section, and then proceed to remove the lesion.
Do vocal cord tumors always result in total laryngectomy?
Far from it; it depends on the stage… Here’s a very simplified “sense” of the various options.
- Early stage cancer often requires only laser or radiotherapy;
- middle stages often laser or partial laryngectomy;
- advanced stages may start with chemo and radiation or sometimes laryngectomy.
Laryngectomy happens most often these days for when recurrence after other treatments have failed and tumor has persisted or come back.
To refuse treatment would mean throwing one’s life away, but people definitely have the right to do this. The result is—over time—slow suffocation if it blocks the airway; difficulty swallowing, pain, bleeding, etc. Make sure you understand what is involved. If rehabilitated well, there is VERY GOOD life after laryngectomy…
- Agrawal N, Ha P H. Management of early-stage laryngeal cancer. Otolaryngol Clin North Am. 2008; 41(4): 757-69. [↩]