Total Laryngectomy
Total laryngectomy is the ultimate surgical option for larynx cancer, in which the entire voice box is removed. Options used to avoid total laryngectomy are:
- endoscopic laser surgery
- partial laryngectomy
- radiation
- chemo/radiation
Today, total laryngectomy is most often a salvage procedure, performed after failure of the initial treatment. It is still, however, a good primary option for very advanced tumors not likely to respond to chemo/radiation.
Change in Anatomy: Breathing
You can no longer breathe through your nose and mouth, but instead only through an opening or stoma at the base of the neck. Technically speaking, this is a tracheostomy, not a tracheotomy. After total laryngectomy, many persons’ stomas are self-maintaining, and this explains why there is often no need for a tracheal tube—because the person is breathing through an -ostomy (or stoma) that holds itself open.
Change in Anatomy: Swallowing
Swallowing is just as other people do. The difference is that the foodway is completely separated from the airway. In other words, the mouth and throat lead only into the esophagus. This means that it is physically impossible to aspirate (put food or saliva into the airway) unless the trachea-esophageal voice prosthesis or TEP (see below) is leaking.
Change in Anatomy: Talking
Talking is achieved in one of the three ways indicated below:
- Surgeons created a tracheoesophageal fistula through the back wall of the trachea and into the esophagus. A plastic device (tracheoesophageal prosthesis or TEP) containing a one-way valve to prevent backflow of saliva or food, was then placed in the fistula to allow the patient to divert pulmonary air through the TEP and into the esophagus. When the patient does this by “capping” their stoma while breathing out, the esophageal tissues vibrate and produce their esophageal pulmonary air-powered esophageal voice.
- A mechanical vibrator is held against the side of the neck to transmit sound through the tissues of the neck and into the throat.
- A semi-swallowed air-powered esophageal voice: The patient slightly “swallows” or “charges” air into the upper esophagus, and then releases it to produce vocal sound.
Key Point Summary about Status after Total Laryngectomy:
- Breathing does not occur through the nose and mouth, but ONLY through the stoma at the base of the neck.
- The stoma is not “delicate” or “dangerous.”
- The TEP device fitted into the tracheo-esophageal fistula must remain in position at all times.
- If for whatever reason the TEP comes out, put a red rubber catheter through the “empty” fistula tract so that it cannot heal closed. This avoids needing another operation to re-create the fistula.
- If the TEP is noted to be missing, first check the pajamas, bedclothes, floor, etc. to try to find it.
- If not found, as long as the red rubber catheter is in place, there is no emergency, but you should contact the patient’s laryngologist for further instructions.
What if I need mechanical ventilation for anesthesia during surgery?
The anesthesiologist must understand some basic things:
- All breathing must be done through the stoma at the base of the neck. Oxygen supplied to the nose or via a mask on the patient’s face is of no benefit—because there is no connection from the mouth and nose to the airway!
- The TEP (small plastic “bobbin” seen on the back wall of the trachea just inside the stoma) must be left in place during the procedure. On the other hand, if the patient uses a soft silastic breathing tube in addition to the TEP (used by only a small percentage of laryngectomees), this can be removed for further airway management during administration of general anesthesia.
Step-by-step instructions for how to manage breathing under general anesthesia
- Determine if the breathing tube that may be in the stoma needs to be removed:
- DON’T REMOVE if the patient doesn’t use this sort of tube, and breathes directly into a “bare” stoma.
- REMOVE if the patient uses a soft silastic breathing tube, which you can remove.
- “Never” remove the TEP “bobbin!” (The patient will show it to you before you put them under anesthesia.)
- Drip a couple of milliliters of 4% xylocaine into the stoma. This will make the patient cough. Wait a minimum of 90 seconds for the “numbing action” to occur in the trachea before proceeding.
- Insert a 6.5 or 7.0 endotracheal tube gently past the TEP device. The TEP is fairly secure and would be difficult to dislodge unless the endotracheal tube tip were to ‘”catch” the edge of the flange directly. Note that the carina is only a short distance below the stoma; therefore, the endotracheal tube should only be advanced until its balloon just enters the stoma.
To say this another way, the endotracheal tube will not be inserted to the usual 22 cm mark, but instead an estimated 5 or 6 cm.
- Inflate the balloon, attach the anesthesia circuit, and begin ventilation.
- When the surgery is finished and the patient is breathing on their own again, remove the endotracheal tube. The patient should let you know prior to surgery if they happen to need the soft silastic tracheal tube (see #1 above), so that you can re-insert it now, gently, and with care again not to dislodge the TEP device.
- KEY POINT: Please carefully verify that the TEP device the patient showed you before the surgery is in the same position that it was at the beginning of the case.
- IF the TEP device is not visible (and this is unlikely), do the following:
- First, try to locate it: Look on the sheets, into the upper part of the trachea by direct vision, etc. Use a fiberoptic bronchoscope to easily visualize the trachea and the mainstem bronchi.
- If not found “on the floor” or in my trachea, my surgeon may examine the upper esophagus or use x-ray as in iii below:
- If the TEP is still missing at this point, a chest x-ray can be done while the patient is still asleep to make sure the device was not dislodged into the trachea.
- Once the TEP is found, or definitively “lost” but verified not to be in the airway, do not try to reposition original or new TEP, unless you are a laryngologist or speech pathologist familiar with these devices. Instead, get a #16 or #18 red rubber catheter and slip it into the little opening on the back of the upper trachea, then downward into the esophagus. Tie a knot in the catheter just beyond the proximal (funnel shaped) end; that way, if the patient regurgitates or refluxes stomach contents into the esophagus, this material won’t be able to also travel through the catheter and drip down their chest!
- Tie a 20-inch piece of cotton “twill” tape (often used in other contexts to attach tracheotomy tubes around the neck) adjacent to the knot you tied in the red rubber catheter. Then tie the ends of the twill tape around the neck. This will hold the red rubber catheter in position.
- The patient will then see their speech pathologist within a few days. She or he will remove the red rubber catheter that has kept the fistula open, and re-fit them with a new TEP.
Suggested Discharge Instructions after Surgery
Bulb Suction
Empty bulb every twelve hours and record output. With stopper open, squeeze the bulb flat and replace stopper to keep it flattened and reactivate the suction. Call your physician if the drainage amount increases significantly over previous day, or if you see saliva or murky, infected-looking material in the drain tubing or bulb.
Tracheostomy Care: Stomavent Cleaning
This is done using clean, not necessarily sterile technique. Twice a day, remove stomavent tube. Place it in 1:1 water/ peroxide solution. Use fingers and/ or “pipe cleaner” to dislodge mucus. Clean around stoma with gauze moistened with solution; reinsert tube. Note that some crusts tend to adhere to the silk sutures around the stoma. Remove these as possible, but do not be concerned if you are unable to dislodge them all.
Nutrition
Until your swallowing passage heals (usually about 2 weeks), you will need to self-administer tube feedings at home. You will receive specific instructions about the amount and timing. Be sure to flush the tube with 50 ml of water before and after each feeding. If you feel full in the middle of a feeding, stop, flush with water, and wait an hour before you resume that feeding. If you are taking medications, you need to crush them to a fine powder, dissolve them in 50ml of water and administer it through feeding tube as you would the feedings. Flush after medications with 50ml of water also. If you feel thirsty between feedings, or if your urine looks concentrated, administer an amount equal to a glass of water through feeding tube.
Suctioning
If you have excessive secretions and are unable to cough them up, you will have a suction machine and catheter to use at home in the same manner as you were shown in the hospital. Alternatively, or in addition, instill saline into the stoma as directed. This will make you cough and at the same time moisten / loosen adherent crusts. If these measures fail to remove retained mucus, feel free to call your physician.
Supplies
You will need to procure the following items from your pharmacy:
- Pill crusher
- Enteral feeding solution recommended by dietician (unless provided by home healthcare agency)
- Gauze pads, and peroxide.
- Your physician usually gives you: extra stomavent ties, sterile water for cleaning tube, syringe set for giving feedings, measuring cup for feedings and for bulb drainage measurement, and reusable trach cleaning set for your stoma tube.
Go Straight to Total Laryngectomy, or Give Thulium Laser a Chance?
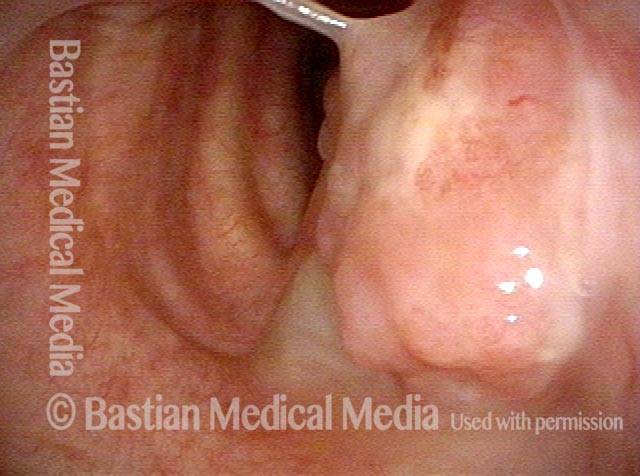
Lesion (1 of 5)
Lesion (1 of 5)
Decisions (2 of 5)
Decisions (2 of 5)
Removal (3 of 5)
Removal (3 of 5)
Bulk of tumor is gone (4 of 5)
Bulk of tumor is gone (4 of 5)
Complete healing? (5 of 5)
Complete healing? (5 of 5)
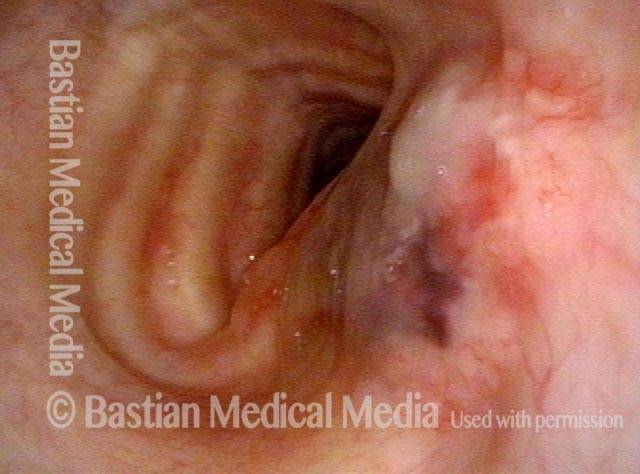
How a Sphincter Works
Open (1 of 2)
Open (1 of 2)
Contracted (2 of 2)
Contracted (2 of 2)
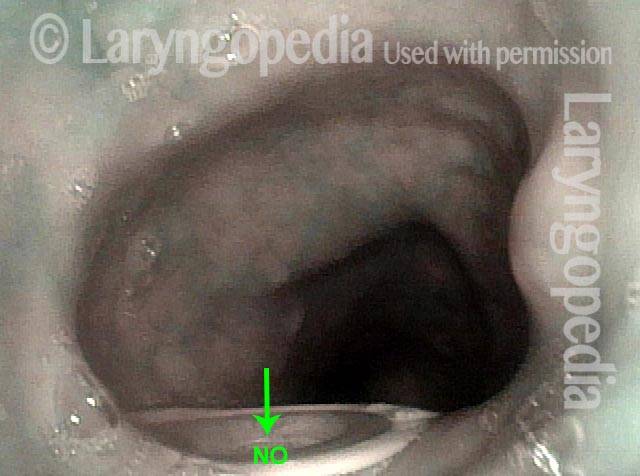
How the One-Way Flapper Valve Works in A Tracheo-Esophageal Voice Prosthesis
Food and liquid blocked from trachea (1 of 3)
Food and liquid blocked from trachea (1 of 3)
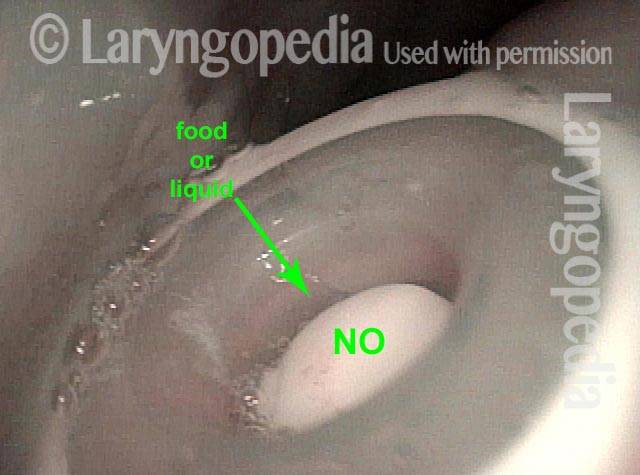
Closer look at closed valve (2 of 3)
Closer look at closed valve (2 of 3)
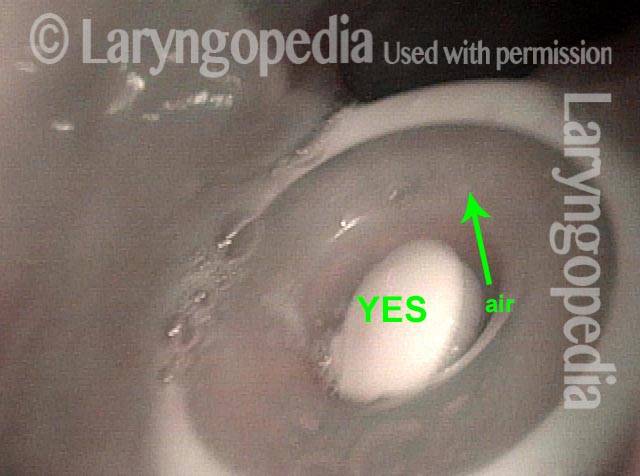
Opened valve (3 of 3)
Opened valve (3 of 3)
Share this article