Tracheotomy Tube
A tracheotomy tube is a device that is surgically placed into the trachea low in the neck, with its tip well inside the trachea and its other end anchored to a faceplate that sits on the surface of the neck.
A tracheotomy tube allows an individual to breathe directly from the neck opening into the trachea as an alternative to normal breathing through the nose and/or mouth. “Trach” is the colloquial term used by clinicians to refer to a tracheotomy tube.
Tracheotomy tubes may be made of stainless steel or plastic.
Tracheotomy Home Care
Instructions for managing a tracheotomy tube outside of the hospital setting may vary between institutions. There is an input from “best medical practice,” but another input from common sense and “practicality.” We are summarizing below what the clinicians at Bastian Voice Institute teach their patients.
Keep in mind that the hospital management of tracheotomy tubes is much more intense than what follows below. This is because infection control practices must be much more meticulous in that environment to avoid a hospital-acquired infection, and because initial management of a newly established tracheotomy is different than the maintenance of an established tracheotomy.
Basic Information
- Every tracheotomy device has three parts: obturator; inner cannula; outer cannula.
- Only TWO of the three parts are ever in use at once, but you should keep all three parts at hand.
- The obturator and outer cannula are used at the time of complete tube change, just for the moment of insertion.
- The inner cannula and outer cannula are in use continuously while wearing the tracheotomy tube. (Exception: you will wear the outer cannula by itself for the few minutes needed to clean and change the inner cannula)
- Tracheotomy tubes tend to stimulate the production of mucus. Occasional tinges of blood are also normal.
- Mucus is cleared from the tracheotomy tube in one of four ways:
- By using suction. This is typically needed only during a hospital stay. That said, a suction machine is routinely part of the equipment you are sent home with, just in case of need. The machine can often be returned to the home health agency after you learn that you don’t need it.
- By removing the inner cannula narrowed or blocked by mucus, and then cleaning, and re-installing it within the outer cannula.
- By vigorous coughing into a tissue held over the opening of the tracheotomy tube.
- As an extension of c: By instilling saline into the trach tube, which will be followed “automatically” by vigorous coughing. This is particularly effective if the problem is dry crusts that are more common in the dry indoor air of Winter.
- The inner cannula should be routinely removed, cleaned, and replaced twice a day even if there seems to be no need. And if mucus accumulates frequently, it can be cleaned as often as necessary.
- The outer cannula (the part with attached faceplate) should be removed / replaced once a week. You clinician (doctor or nurse) will do this for you the first time or two while you are still learning, then watch you do it yourself a couple more times (possibly on the same day of your first change), and then you should be doing this on your own, with a family member nearby, at home. See also: Instructions for Tracheotomy Tube Change.
Do I wear gloves when working with my trach tube, like they taught me in the hospital?
While this was important in the hospital, you only need to wash your hands well at home. No gloves are needed.
They sent me home with suction machine. Am I supposed to use it?
That depends. Most patients do not use the suction machine at home if their cough is strong and they use frequent saline “squirts.” The combination of a little squirt of saline down the tube and the coughing that follows is sufficient for most people.
The commonest exception would be for someone who is so weak from illness that they cannot cough up their own secretions.
They also sent me home with a humidification “machine” and tubing that leads to my tracheotomy tube. Is it important to use this?
Again, the answer is that only rarely do patients need this sort of device, whose sole purpose is to provide moistened air into the trachea. This is useful in hospital, in the first few days after the tracheotomy procedure was done, when secretions are more abundant and may crust. Thereafter, saline squirts are equally-if not more-effective.
How often can I use the saline squirts?
To make the point that they can be used as often as you like, we often say, only a little facetiously, “Not more than 50 times a day!”
A Fenestrated Tracheotomy Tube allows Voicing when there Is Stenosis
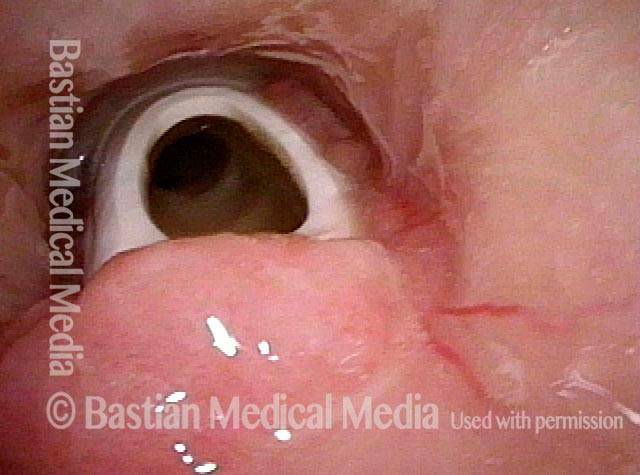
Tracheotomy (1 of 4)
Tracheotomy (1 of 4)
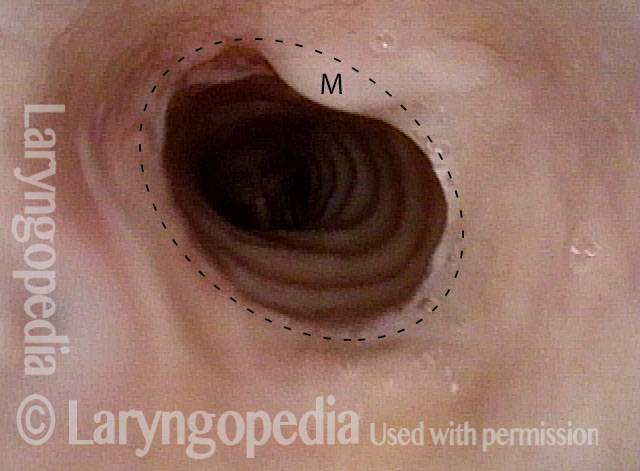
View below vocal cords (2 of 4)
View below vocal cords (2 of 4)
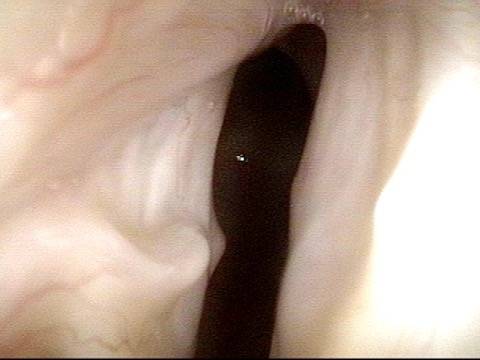
Fenestra (3 of 4)
Fenestra (3 of 4)
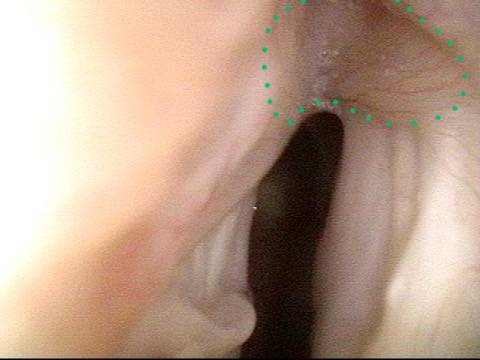
Patient post-trach (4 of 4)
Patient post-trach (4 of 4)
Nuances of Endotracheal Tube Injury
This woman with high-risk comorbidities of diabetes and obesity, was in ventilated in ICU more than a month for pulmonary complications of Covid-19 infection. She had an orotracheal tube in place for 3.5 weeks, and then a tracheotomy tube was placed. Now at her first visit a year later, she remains tracheotomy-dependent, and is told she has bilateral vocal cord paralysis (disproven in the following photo series).
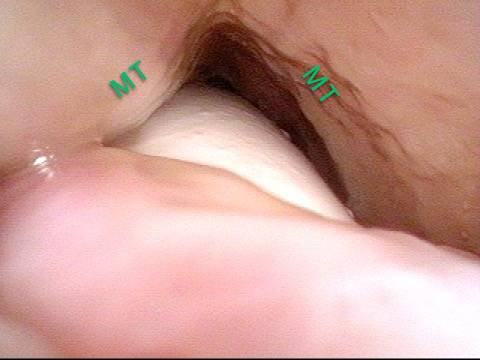
Maximum glottic opening (1 of 8)
Maximum glottic opening (1 of 8)
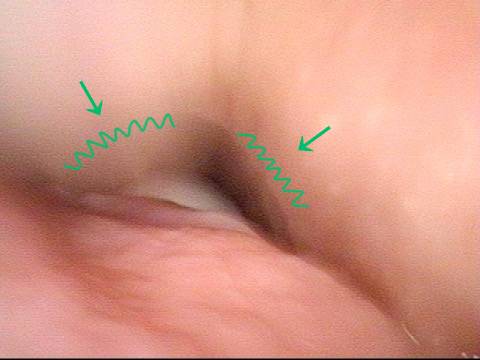
Undersurface mucosa indraws (2 of 8)
Undersurface mucosa indraws (2 of 8)
Phonation (3 of 8)
Phonation (3 of 8)
Posterior commissure divot (4 of 8)
Posterior commissure divot (4 of 8)
Further evidence of scarring (5 of 8)
Further evidence of scarring (5 of 8)
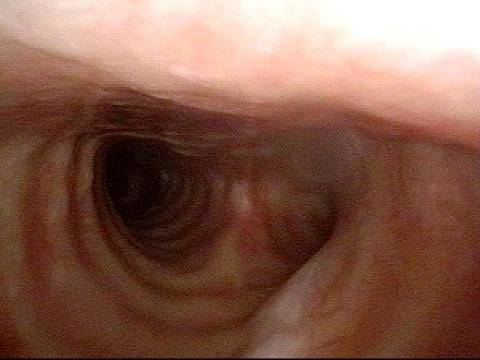
View into trachea (6 of 8)
View into trachea (6 of 8)
Vibration of trachea (7 of 8)
Vibration of trachea (7 of 8)
Open trachea beyond the tube (8 of 8)
Open trachea beyond the tube (8 of 8)
The plan here is posterior commissuroplasty, followed by placement of a smaller trach tube and a trial of plugging. If plugging is tolerated during the day, she will need a sleep study with it plugged at night, given the tracheomalacia and her obesity.
Trachea, with Tracheotomy Tube
Trachea, with tracheotomy tube (1 of 2)
Trachea, with tracheotomy tube (1 of 2)
Trachea, with tracheotomy tube (2 of 2)
Trachea, with tracheotomy tube (2 of 2)
Share this article