 The trachea, or windpipe in layman’s terminology, begins on its upper end just below the larynx and extends inferiorly into the chest where it splits into the right and left mainstem bronchi; delivering inspired air to the right and left lungs, respectively.
The trachea, or windpipe in layman’s terminology, begins on its upper end just below the larynx and extends inferiorly into the chest where it splits into the right and left mainstem bronchi; delivering inspired air to the right and left lungs, respectively.
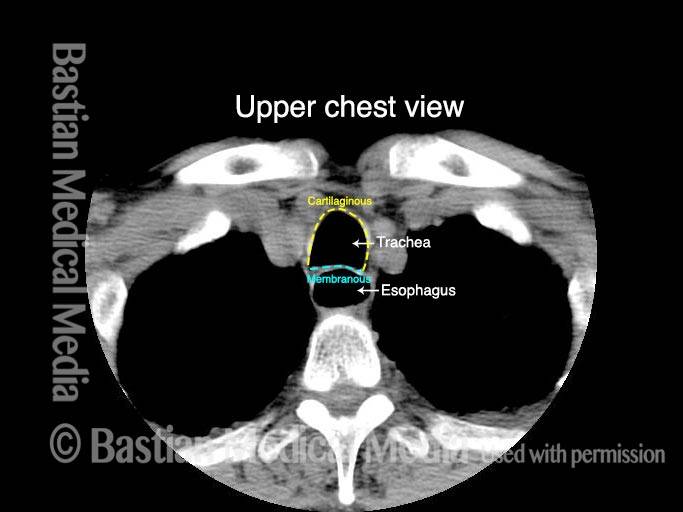
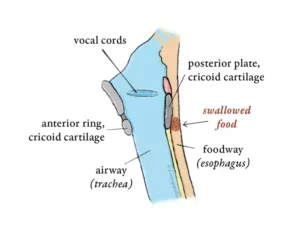
The tracheal rings comprise approximately two-thirds of the circumference of the trachea, anteriorly and laterally. The remaining posterior one-third “membranous” tracheal mucosa is the anterior surface of the “party wall” it shares with the esophagus.
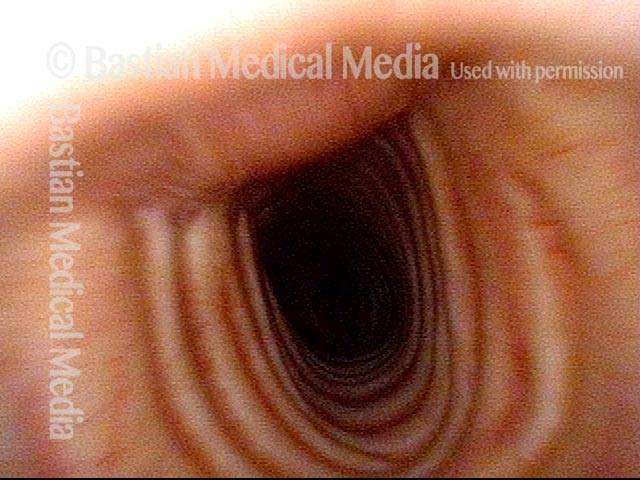
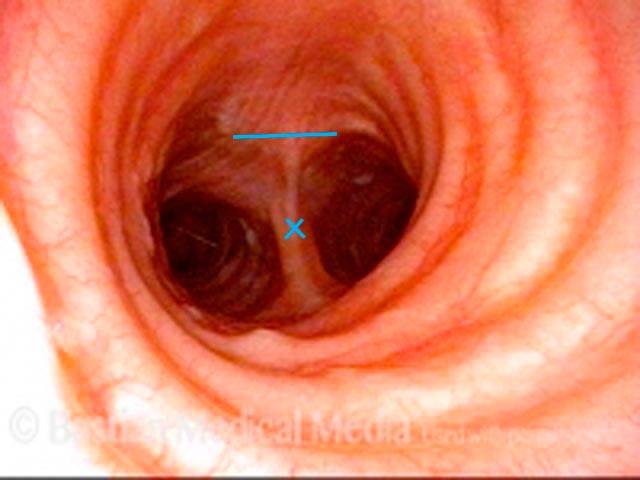
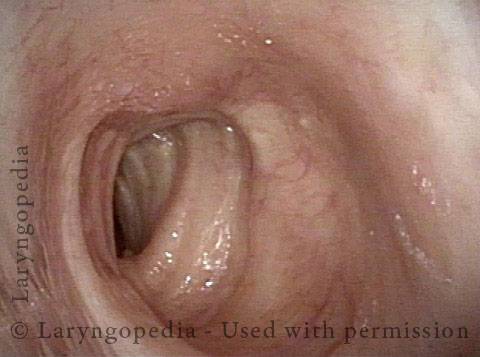
Trachea (1 of 2)
Trachea (1 of 2)
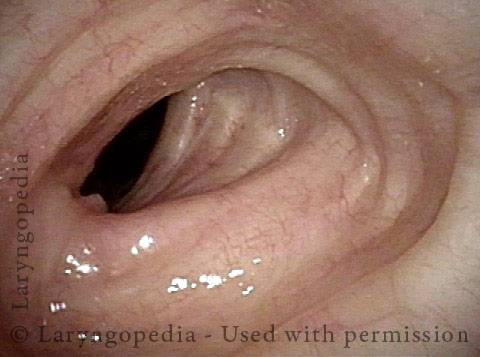
Tracheal rings (2 of 2)
Tracheal rings (2 of 2)
Example 2
Trachea X-Ray (1 of 1)
Trachea X-Ray (1 of 1)
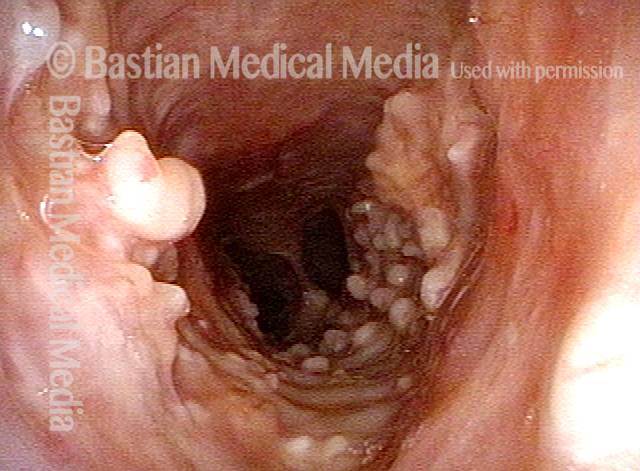
Benign Bony Growths in the Trachea Called Tracheobronchopathia Osteochochondroplastica!
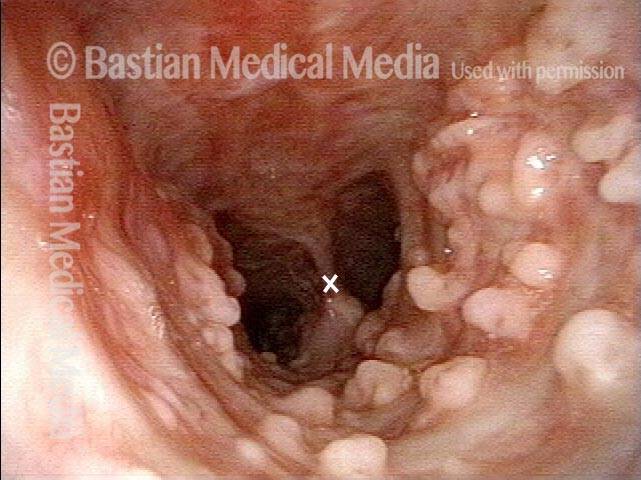
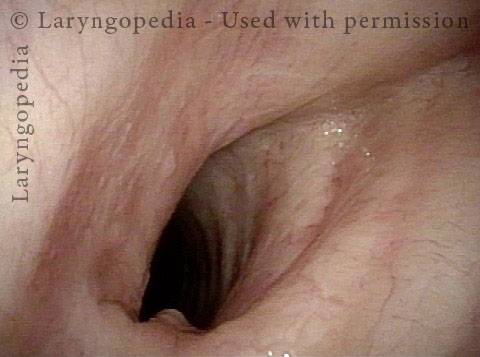
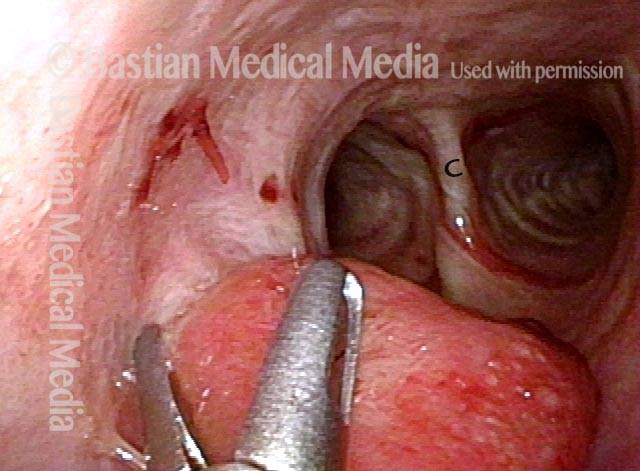
View into mid-trachea, diagnosis unknown (1 of 4)
View into mid-trachea, diagnosis unknown (1 of 4)
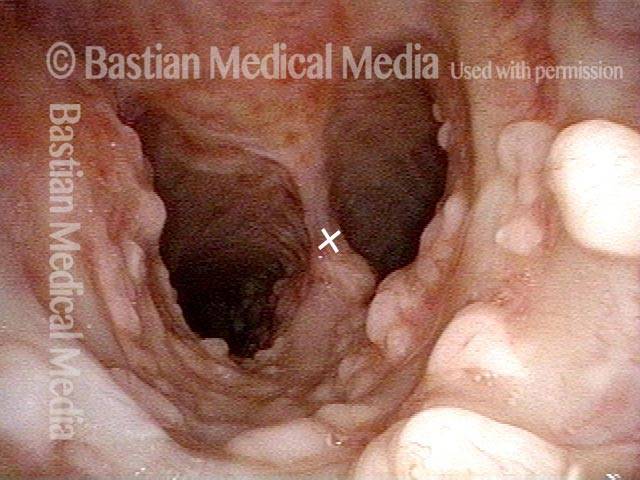
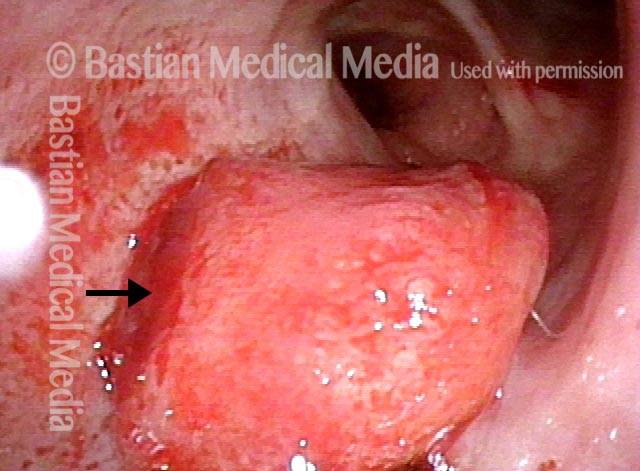
Spicules found in the tracheal wall (2 of 4)
Spicules found in the tracheal wall (2 of 4)
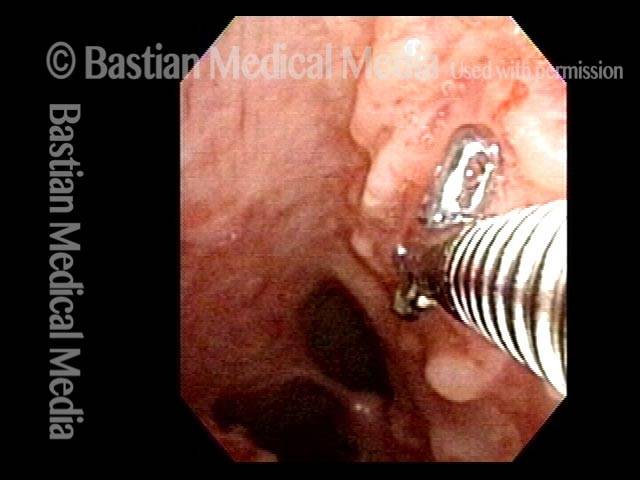
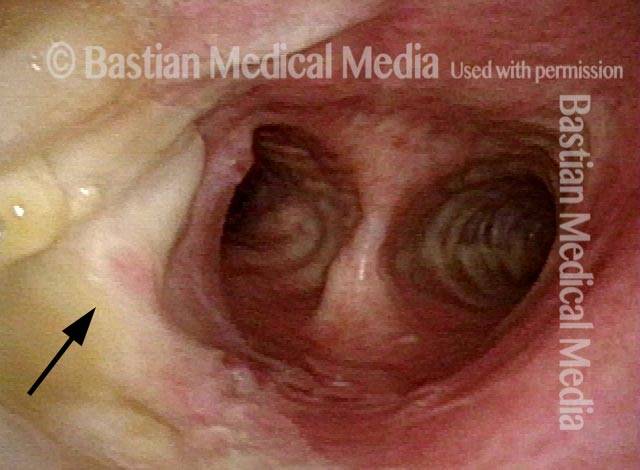
Diagnosis revealed (3 of 4)
Diagnosis revealed (3 of 4)
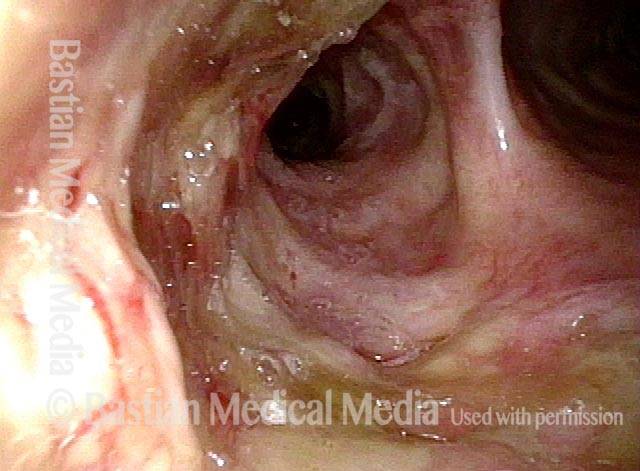
Biopsy reveals bone tissue (4 of 4)
Biopsy reveals bone tissue (4 of 4)
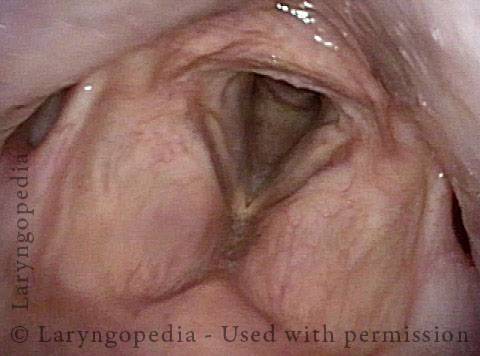
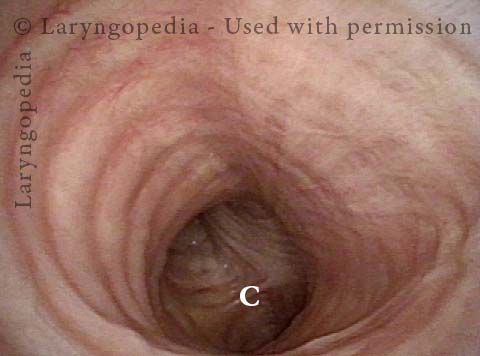
Tracheal Deformity After Tracheotomy
This man had a grave and life-threatening illness that required mechanical ventilation in an ICU for about 3 months. The initial weeks were through an oro-tracheal tube (a tube placed through the mouth, between the vocal cords, and into the trachea); the remaining 2 ½ months were via a tracheotomy (breathing tube inserted through the base of the neck directly into the trachea). Now out of hospital for many months, he has a barking cough, and occasionally mild harsh inspiratory noise.