The mucous membranes (or mucosa) are to our interior as skin is to our exterior. Mucosa covers or lines various body cavities and internal organs. In laryngology, the mucosa of the vocal cords is the point of main susceptibility to vibration-induced traumatic abnormalities such as nodules, polyps, capillary ectasia, and so forth. Mucosa also lines the nose, mouth, pharynx, esophagus, and tracheobronchial tree.
Healed Mucosa After Ulcerative Laryngitis
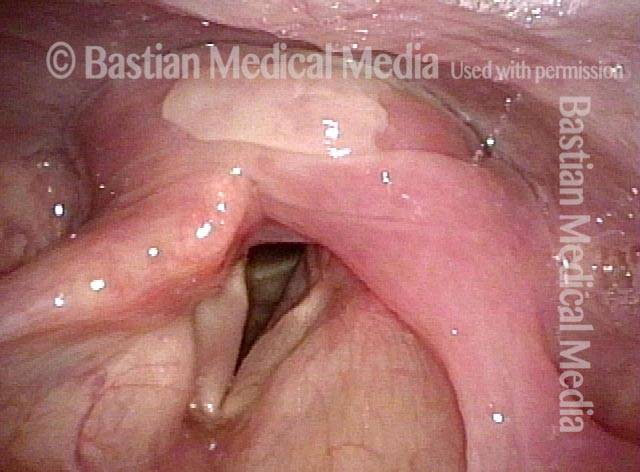
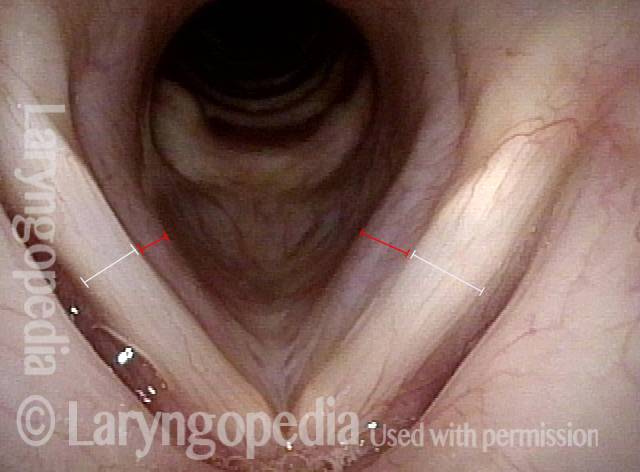
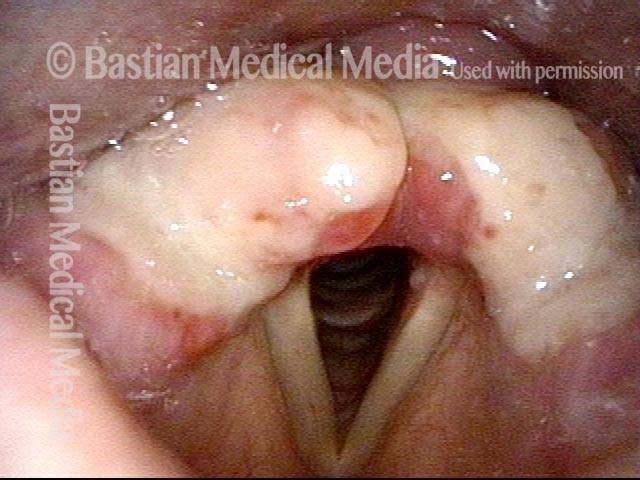
Ulcerative laryngitis (1 of 4)
Severe ulcerative laryngitis. Mucosa has sloughed away in the area of the white patches, not yet re-mucosalized.
Ulcerative laryngitis (1 of 4)
Severe ulcerative laryngitis. Mucosa has sloughed away in the area of the white patches, not yet re-mucosalized.
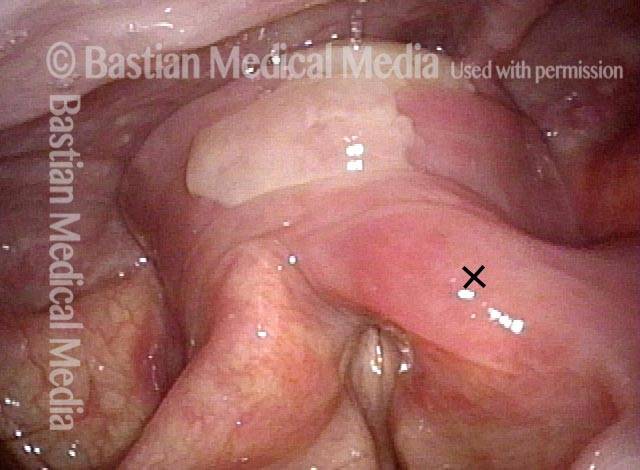
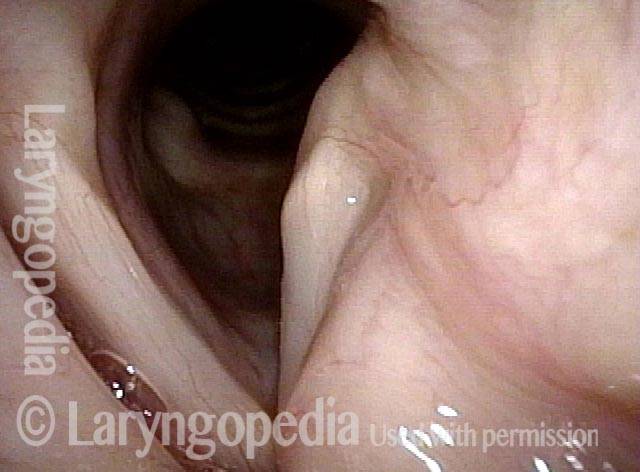
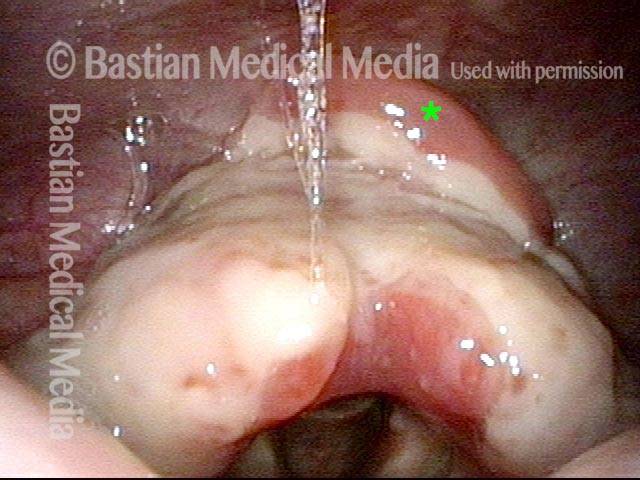
Six weeks later (2 of 4)
As is typical for ulcerative laryngitis, the mucosa takes 6 weeks or more to regenerate. This is six weeks after photo 1. Soon after this examination, voice returned to nearly-normal.
Six weeks later (2 of 4)
As is typical for ulcerative laryngitis, the mucosa takes 6 weeks or more to regenerate. This is six weeks after photo 1. Soon after this examination, voice returned to nearly-normal.
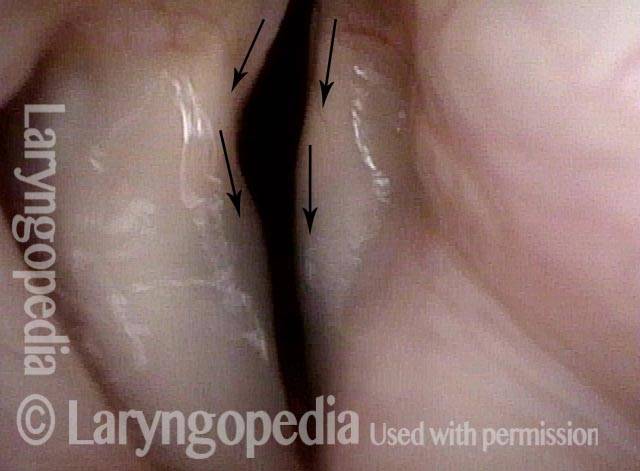
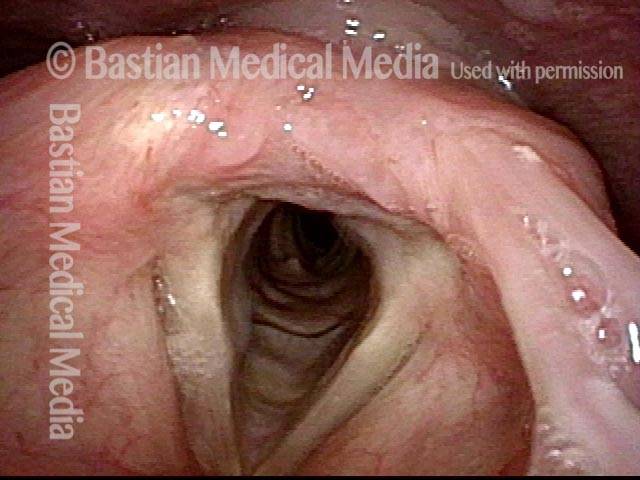
7 years later (3 of 4)
About 7 years later, the voice remains essentially normal. Still, in this standard light view, one can see a faint white area in the area of the original ulceration. This is better appreciated in the next photo.
7 years later (3 of 4)
About 7 years later, the voice remains essentially normal. Still, in this standard light view, one can see a faint white area in the area of the original ulceration. This is better appreciated in the next photo.
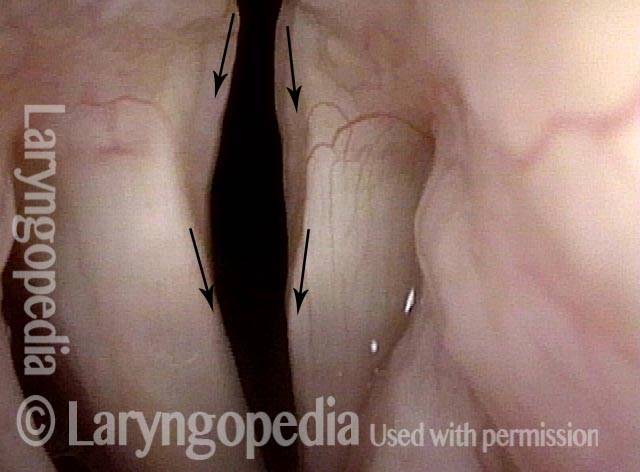
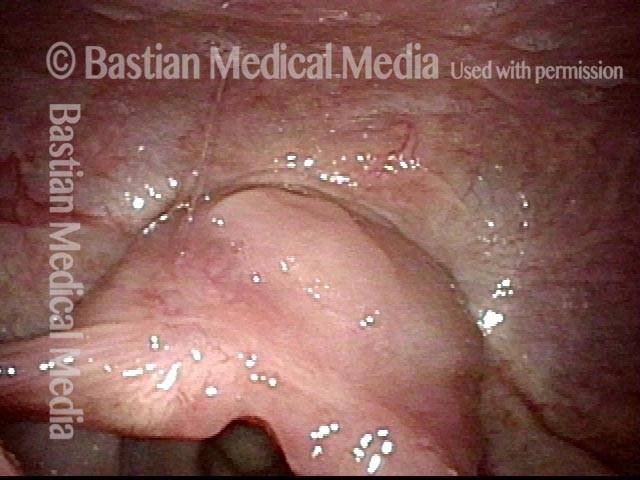
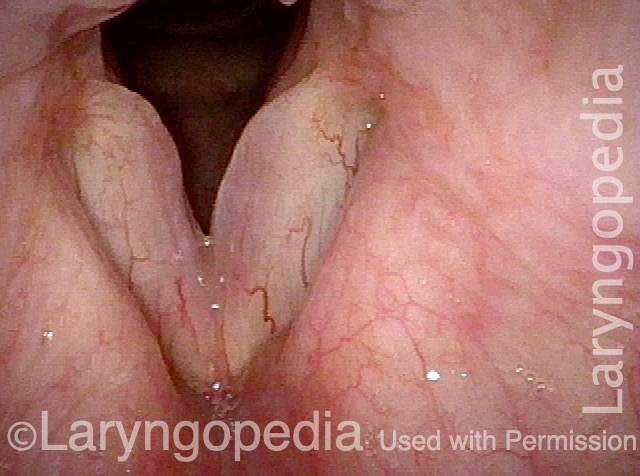
Narrow band lighting (4 of 4)
Under narrow band light, the (originally) more deeply ulcerated right vocal cord (left of photo) remains more avascular than the left (right of photo), where the capillary pattern has returned, but still with a demarcated area of reduced micro-capillaries causing a whiter appearance.
Narrow band lighting (4 of 4)
Under narrow band light, the (originally) more deeply ulcerated right vocal cord (left of photo) remains more avascular than the left (right of photo), where the capillary pattern has returned, but still with a demarcated area of reduced micro-capillaries causing a whiter appearance.
Pills can get Stuck and Burn
Superficial ulceration (1 of 4)
Superficial ulceration of post-arytenoid and -cricoid mucosa, where a pill was lodged in her throat. It took several hours to melt it with many sips of water; a sore throat ensued.
Superficial ulceration (1 of 4)
Superficial ulceration of post-arytenoid and -cricoid mucosa, where a pill was lodged in her throat. It took several hours to melt it with many sips of water; a sore throat ensued.
Inflamed pyriform (2 of 4)
Closer view. Note inflammatory reaction in left pyriform (right of photo) and left arytenoid (right of photo) apical mucosa (arrow and 'X', respectively).
Inflamed pyriform (2 of 4)
Closer view. Note inflammatory reaction in left pyriform (right of photo) and left arytenoid (right of photo) apical mucosa (arrow and 'X', respectively).
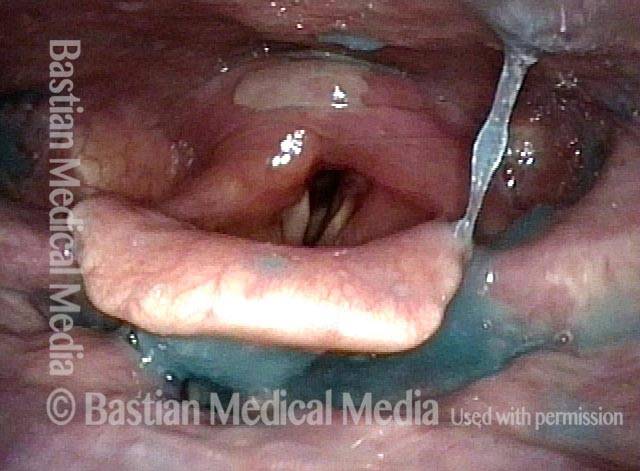
Oropharyngeal dysphagia (3 of 4)
After blue-stained applesauce, this residue confirms that the patient has mild oropharyngeal dysphagia.
Oropharyngeal dysphagia (3 of 4)
After blue-stained applesauce, this residue confirms that the patient has mild oropharyngeal dysphagia.
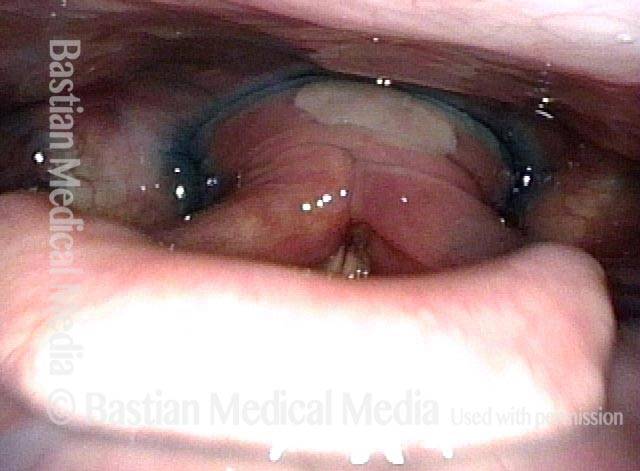
Hypopharyngeal crescent (4 of 4)
After blue-stained water pools in an organized way in the hypopharyngeal crescent, the question of cricopharyngeus muscle dysfunction (non-relaxation) is raised, but not yet confirmed.
Hypopharyngeal crescent (4 of 4)
After blue-stained water pools in an organized way in the hypopharyngeal crescent, the question of cricopharyngeus muscle dysfunction (non-relaxation) is raised, but not yet confirmed.
Classic TA + LCA-only Paresis, Right Vocal Cord
Atrophy of the conus (1 of 5)
This middle-aged woman awakened with a drastically altered, weakened voice. In this abducted position we can say both PCA muscles are normal. We can't assess LCA in this view. It appears that TA is weak on the right cord (left of photo). There is a faint "spaghetti - linguini" difference (white brackets) but the right ventricle does not seem particularly capacious, nor is there any significant margin bowing. The most convincing finding is atrophy of the "conus" part of the vocal cord covered by the darker "purplish" mucosa delineated by the red brackets.
Atrophy of the conus (1 of 5)
This middle-aged woman awakened with a drastically altered, weakened voice. In this abducted position we can say both PCA muscles are normal. We can't assess LCA in this view. It appears that TA is weak on the right cord (left of photo). There is a faint "spaghetti - linguini" difference (white brackets) but the right ventricle does not seem particularly capacious, nor is there any significant margin bowing. The most convincing finding is atrophy of the "conus" part of the vocal cord covered by the darker "purplish" mucosa delineated by the red brackets.
Inability to adduct (2 of 5)
Forced expiration should bring normal cords into slight "mirror image" adduction. In this view, the normal left cord (right of photo) adducts significantly, but the right does not. Now we know for sure that the right LCA muscle is not working. The phonation viewings that follow will allow us to further assess both LCA and TA function.
Inability to adduct (2 of 5)
Forced expiration should bring normal cords into slight "mirror image" adduction. In this view, the normal left cord (right of photo) adducts significantly, but the right does not. Now we know for sure that the right LCA muscle is not working. The phonation viewings that follow will allow us to further assess both LCA and TA function.
LCA weakness (3 of 5)
Low pitch phonation at F3 (175 Hz) with posterior commissure and vocal process mucosa in clear view, provides the "proof" of LCA weakness. Note that the right vocal process fails to turn medially. By contrast, the left vocal process is in line with the rest of the vocal cord and almost over-rotates medially to compensate.
LCA weakness (3 of 5)
Low pitch phonation at F3 (175 Hz) with posterior commissure and vocal process mucosa in clear view, provides the "proof" of LCA weakness. Note that the right vocal process fails to turn medially. By contrast, the left vocal process is in line with the rest of the vocal cord and almost over-rotates medially to compensate.
Further review (4 of 5)
Now more than an octave higher at A-flat 4 (415 Hz), the vocal process is pulled a little bit more in line by the anteroposterior stretch, but the failure to point straight anteriorly (as does the normal left side) again indicates LCA weakness.
Further review (4 of 5)
Now more than an octave higher at A-flat 4 (415 Hz), the vocal process is pulled a little bit more in line by the anteroposterior stretch, but the failure to point straight anteriorly (as does the normal left side) again indicates LCA weakness.
Luffing (5 of 5)
Under a strobe light, the patient is asked to produce voice at low pitch and as loudly as possible. This overwhelms the weak right cord. The audible luffing and the large amplitude and chaotic vibration of the right cord are virtually pathognomonic of vocal cord paralysis and every form of paresis other than PCA-only paresis.
Luffing (5 of 5)
Under a strobe light, the patient is asked to produce voice at low pitch and as loudly as possible. This overwhelms the weak right cord. The audible luffing and the large amplitude and chaotic vibration of the right cord are virtually pathognomonic of vocal cord paralysis and every form of paresis other than PCA-only paresis.
Redundant Supraglottic Mucosa, before and after Surgery
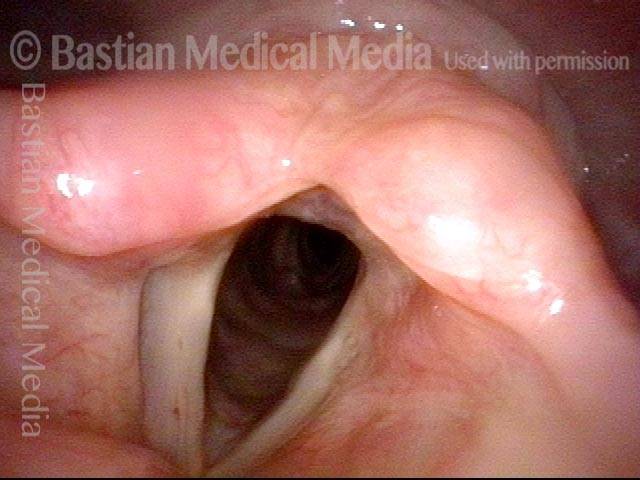
Redundant supraglottic mucosa (1 of 8)
This patient said that, when she breathes in (inspires), she hears noise and feels a sense of obstruction, especially if she inspires rapidly or with her chin down. She had found it necessary to use CPAP while reading with chin down, for example. Here, the patient is breathing quietly, with chin in neutral position, “looking at the horizon.” The vocal cords are abducted, the laryngeal vestibule is open, and there is no breathing noise.
Redundant supraglottic mucosa (1 of 8)
This patient said that, when she breathes in (inspires), she hears noise and feels a sense of obstruction, especially if she inspires rapidly or with her chin down. She had found it necessary to use CPAP while reading with chin down, for example. Here, the patient is breathing quietly, with chin in neutral position, “looking at the horizon.” The vocal cords are abducted, the laryngeal vestibule is open, and there is no breathing noise.
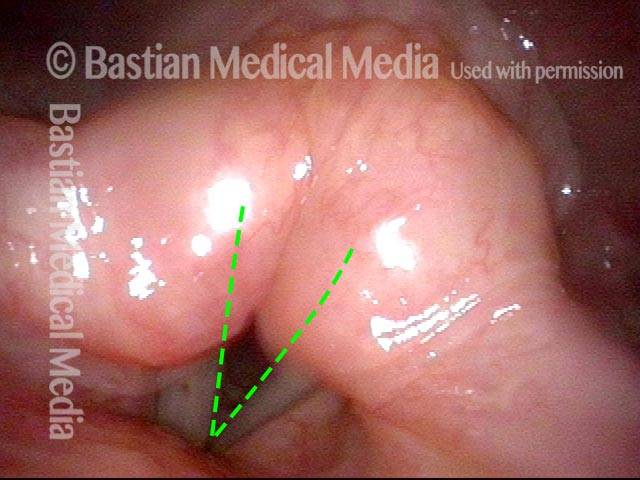
Supraglottic tissue (2 of 8)
Upon request, with her head position unchanged, the patient begins to inspire rapidly. As she inspires, supraglottic tissue (of the arytenoids and aryepiglottic cords) is drawn into the laryngeal vestibule, and harsh breathing noise is heard. This indrawn tissue, which is redundant mucosa, partially obscures the view of the still-abducted vocal cords (dotted lines).
Supraglottic tissue (2 of 8)
Upon request, with her head position unchanged, the patient begins to inspire rapidly. As she inspires, supraglottic tissue (of the arytenoids and aryepiglottic cords) is drawn into the laryngeal vestibule, and harsh breathing noise is heard. This indrawn tissue, which is redundant mucosa, partially obscures the view of the still-abducted vocal cords (dotted lines).
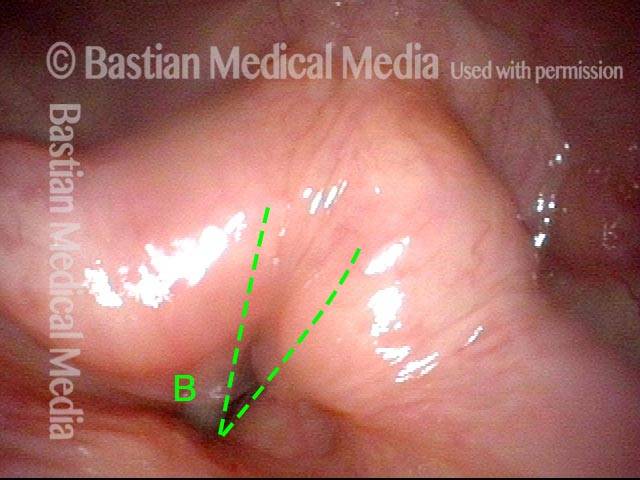
Vibrating mucosal margin (3 of 8)
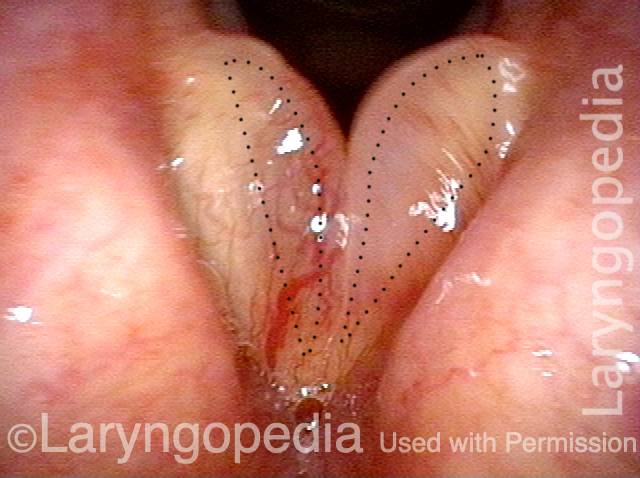
At the peak of rapid inspiration. The vocal cords are still fully abducted (dotted lines) but almost completely obscured by the indrawn mucosa. In addition to the rushing sound, there is also a low-pitched fluttering or rumbling sound, caused by vibration of the leading edge of the indrawn supraglottic mucosa. “B” marks this blurred, vibrating mucosal margin.
Vibrating mucosal margin (3 of 8)
At the peak of rapid inspiration. The vocal cords are still fully abducted (dotted lines) but almost completely obscured by the indrawn mucosa. In addition to the rushing sound, there is also a low-pitched fluttering or rumbling sound, caused by vibration of the leading edge of the indrawn supraglottic mucosa. “B” marks this blurred, vibrating mucosal margin.
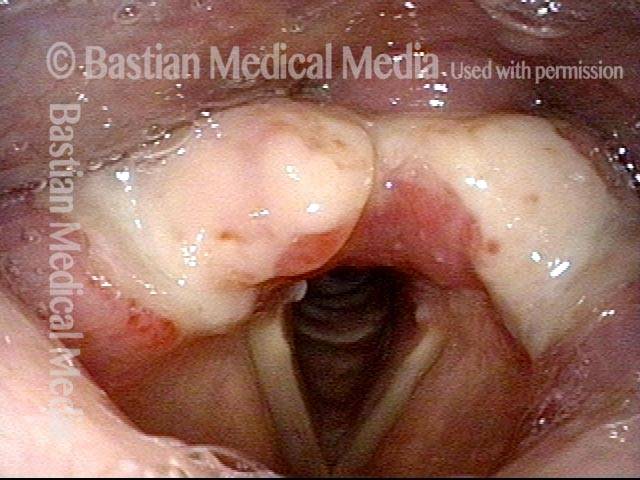
1 week after surgery (4 of 8)
Same patient, one week after laser peeling of the redundant mucosa. The areas which were addressed include: the upper face of the arytenoid, apical mucosa, aryepiglottic mucosa adjacent to the arytenoid, mucosa from the postarytenoid surface, and even some postcricoid mucosa.
1 week after surgery (4 of 8)
Same patient, one week after laser peeling of the redundant mucosa. The areas which were addressed include: the upper face of the arytenoid, apical mucosa, aryepiglottic mucosa adjacent to the arytenoid, mucosa from the postarytenoid surface, and even some postcricoid mucosa.
1 week after surgery (5 of 8)
At the peak of rapid inspiration. The aryepiglottic cords are drawn in slightly, but the laryngeal vestibule remains widely open. Compare with photo 3.
1 week after surgery (5 of 8)
At the peak of rapid inspiration. The aryepiglottic cords are drawn in slightly, but the laryngeal vestibule remains widely open. Compare with photo 3.
1 week after surgery (6 of 8)
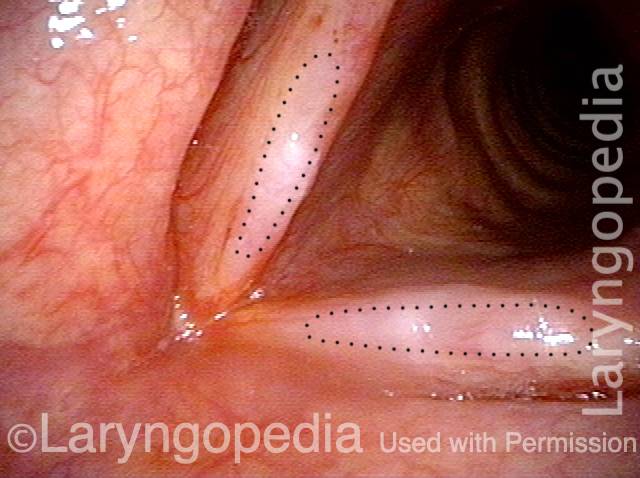
Closer view of surgical details, showing that the entire posterior surface of the arytenoids has been denuded. An asterisk marks the edema at the cut edge of the postcricoid mucosa.
1 week after surgery (6 of 8)
Closer view of surgical details, showing that the entire posterior surface of the arytenoids has been denuded. An asterisk marks the edema at the cut edge of the postcricoid mucosa.
7 weeks after surgery (7 of 8)
Same patient, now seven weeks since laser peeling of the redundant mucosa. As the patient rapidly inspires here, the laryngeal vestibule remains widely open. The patient says that she no longer feels a sense of obstruction or hears noise when breathing, even with her chin down. Compare with photos 2 and 3.
7 weeks after surgery (7 of 8)
Same patient, now seven weeks since laser peeling of the redundant mucosa. As the patient rapidly inspires here, the laryngeal vestibule remains widely open. The patient says that she no longer feels a sense of obstruction or hears noise when breathing, even with her chin down. Compare with photos 2 and 3.
7 weeks after surgery (8 of 8)
The areas that were operated on have healed. Compare with photo 6.
7 weeks after surgery (8 of 8)
The areas that were operated on have healed. Compare with photo 6.
Smoker’s Polyp Reduction Improves Voice Even Though the Larynx Result May not be “Pretty”
Smokers Polyp (1 of 5)
Six years after vocal polyp removal elsewhere. As a result of continued smoking, the voice is deep and rough, and an obvious recurrent/residual "smoker's" polyp is seen on the right vocal cord(arrow, left of photo). The patient "hates" her rough and masculine voice quality.
Smokers Polyp (1 of 5)
Six years after vocal polyp removal elsewhere. As a result of continued smoking, the voice is deep and rough, and an obvious recurrent/residual "smoker's" polyp is seen on the right vocal cord(arrow, left of photo). The patient "hates" her rough and masculine voice quality.
Reine's edema (2 of 5)
Inspiratory phonation is elicited to "pull" the redundant tissue medially, revealing a lot of Reine's edema of the left vocal cord, too. The dotted lines show the ellipse of mucosa that will be removed during surgery. Mucose will be preserved at the margins and the gelatinous lateral within the polyps will be suctioned away if liquid, and dissected away if fibrotic.
Reine's edema (2 of 5)
Inspiratory phonation is elicited to "pull" the redundant tissue medially, revealing a lot of Reine's edema of the left vocal cord, too. The dotted lines show the ellipse of mucosa that will be removed during surgery. Mucose will be preserved at the margins and the gelatinous lateral within the polyps will be suctioned away if liquid, and dissected away if fibrotic.
A week after surgery (3 of 5)
The dotted lines show the extent of mucosal excision—an area that will take a few weeks to re-mucosalize. Since this was a polyp "reduction," though hoarse this early post, she has a " functional" voice. There should be no alarm if patients are aphonic for a week or even a few weeks while inflammation resolves.
A week after surgery (3 of 5)
The dotted lines show the extent of mucosal excision—an area that will take a few weeks to re-mucosalize. Since this was a polyp "reduction," though hoarse this early post, she has a " functional" voice. There should be no alarm if patients are aphonic for a week or even a few weeks while inflammation resolves.
Residual Reinke's edema (4 of 5)
At two months post, the patient is very pleased and says the improvement to voice is "large." Here, it appears there may be some residual Reinke's edema especially of the left vocal cord (right of photo) judging by the slightly convex margin.
Residual Reinke's edema (4 of 5)
At two months post, the patient is very pleased and says the improvement to voice is "large." Here, it appears there may be some residual Reinke's edema especially of the left vocal cord (right of photo) judging by the slightly convex margin.
Residual submucosal edema (5 of 5)
With inspiratory phonation, the residual submucosal edema is made obvious, especially on the left. This was (as intended) a polyp "reduction" approach, rather than polyp "removal" as the latter is too hard on voice, and it is not possible to "put back" if too much tissue is taken. Here, there is no stiffness, and if desired, more can be removed. Of course, since the patient is so pleased with her voice, no further treatment is needed.
Residual submucosal edema (5 of 5)
With inspiratory phonation, the residual submucosal edema is made obvious, especially on the left. This was (as intended) a polyp "reduction" approach, rather than polyp "removal" as the latter is too hard on voice, and it is not possible to "put back" if too much tissue is taken. Here, there is no stiffness, and if desired, more can be removed. Of course, since the patient is so pleased with her voice, no further treatment is needed.
Tagged Anatomy & Physiology, Education