Inability to Burp or Belch
Introduction
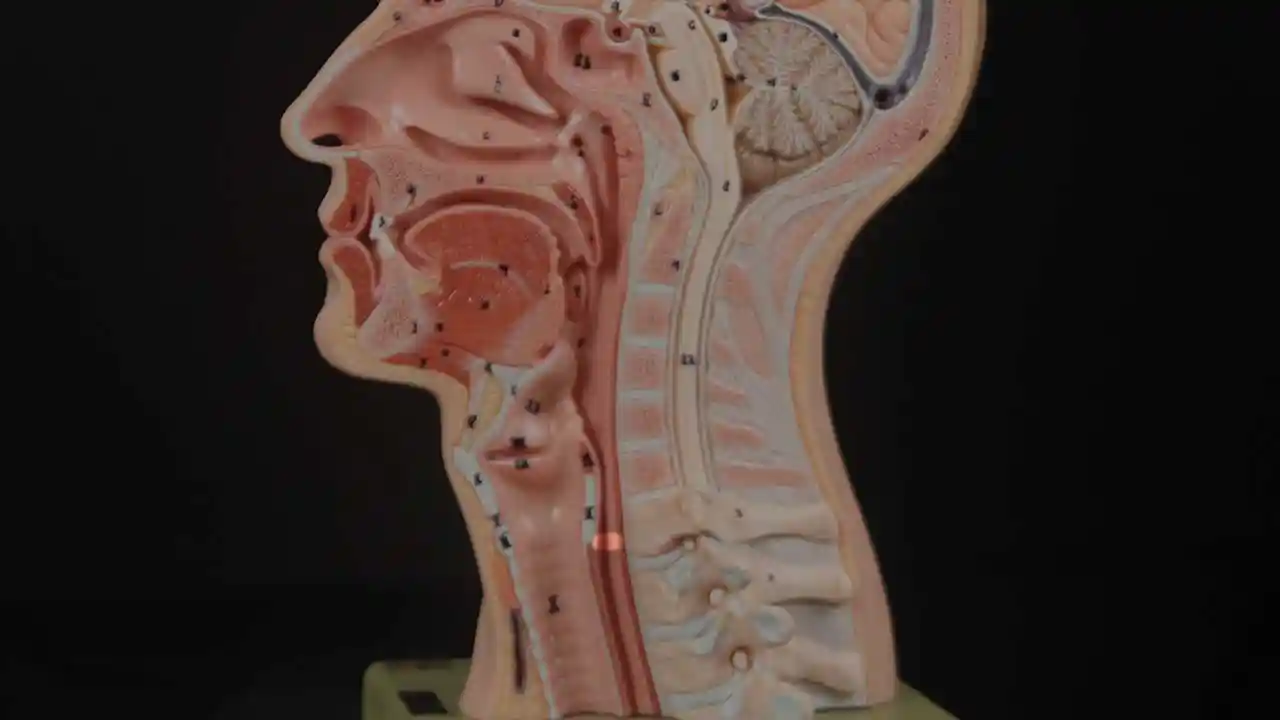
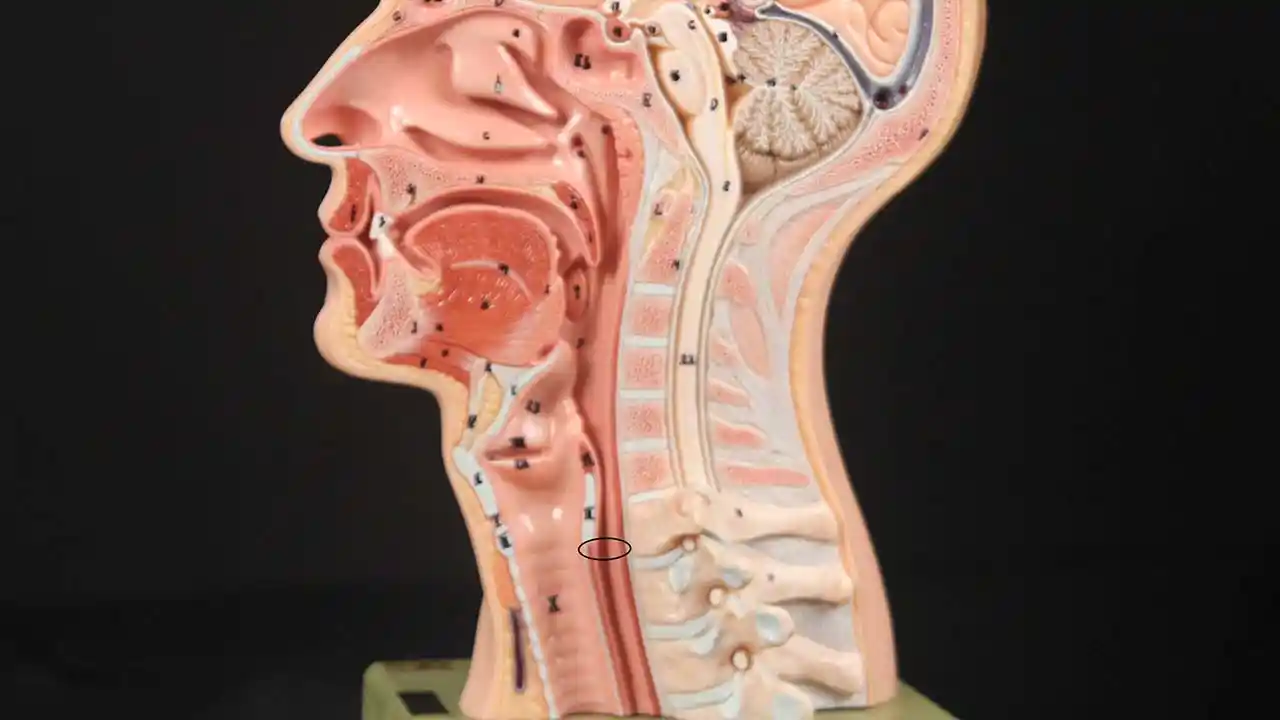
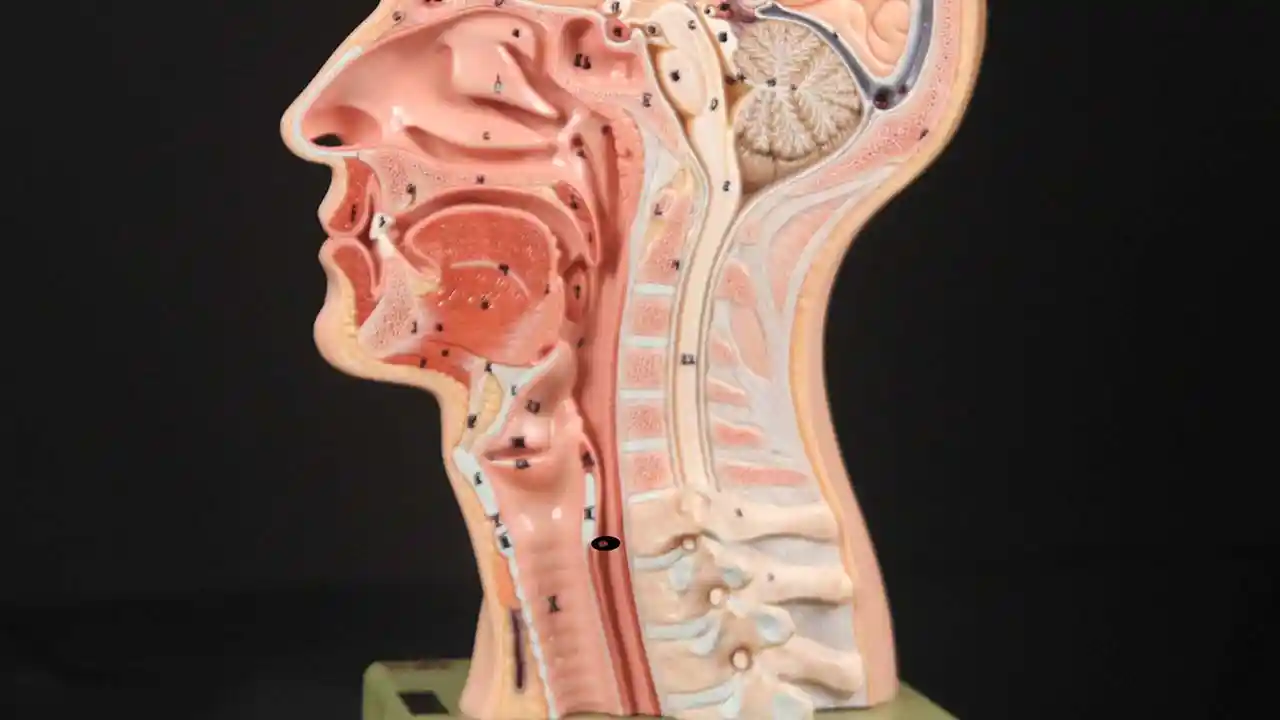
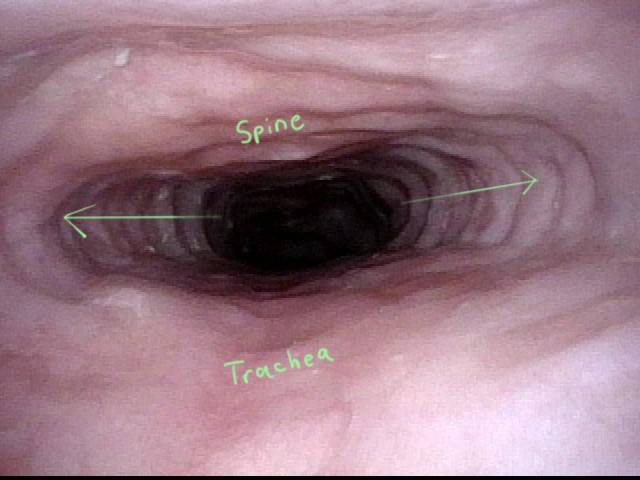
Inability to burp or belch occurs when the upper esophageal sphincter (cricopharyngeus muscle) cannot relax in order to release the “bubble” of air. The sphincter is a muscular valve that encircles the upper end of the esophagus just below the lower end of the throat passage. If looking from the front at a person’s neck, it is just below the “Adam’s / Eve’s apple,” directly behind the cricoid cartilage.
If you care to see this on a model, look at the photos below. That sphincter muscle relaxes for about a second every time we swallow saliva, food, or drink. All of the rest of the time it is contracted. Whenever a person belches, the same sphincter needs to let go for a split second in order for the excess air to escape upwards.
In other words, just as it is necessary that the sphincter “let go” to admit food and drink downwards in the normal act swallowing, it is also necessary that the sphincter be able to “let go” to release air upwards for belching. The formal name for this disorder is retrograde cricopharyngeus dysfunction (R-CPD).
People who cannot release air upwards are miserable. They can feel the “bubble” sitting at the mid to low neck with nowhere to go. Or they experience gurgling when air comes up the esophagus only to find that the way of escape is blocked by a non-relaxing sphincter. It is as though the muscle of the esophagus continually churns and squeezes without success.
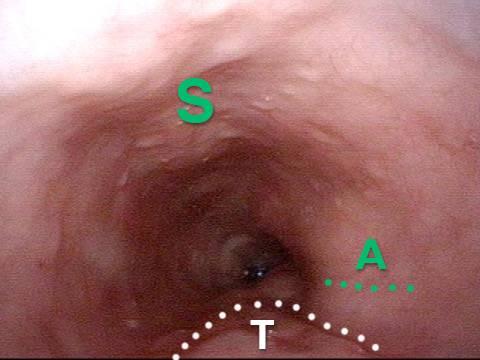
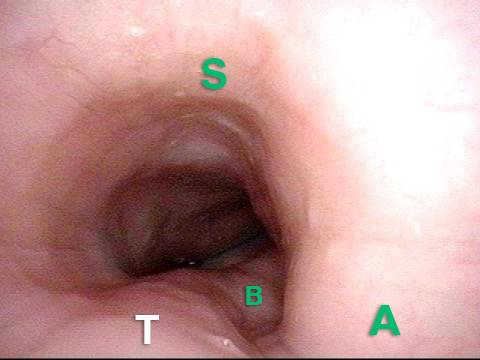
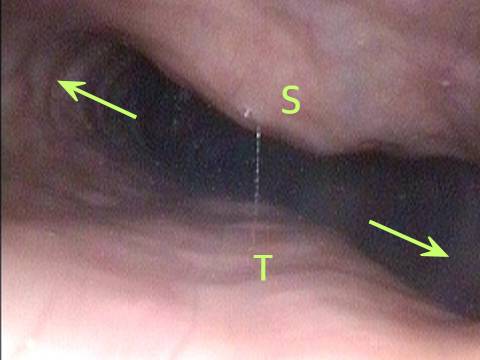
Cricopharyngeus Muscle (1 of 3)
Cricopharyngeus Muscle (1 of 3)
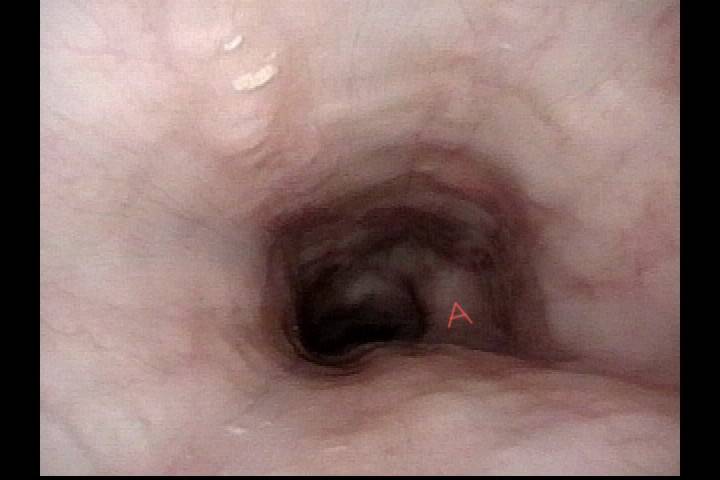
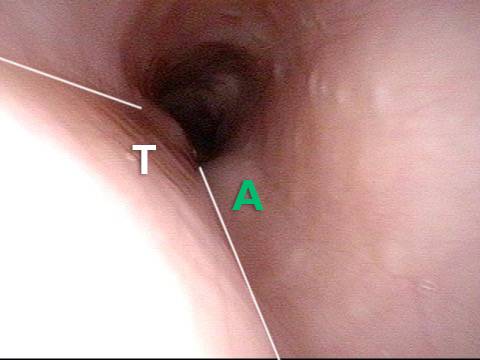
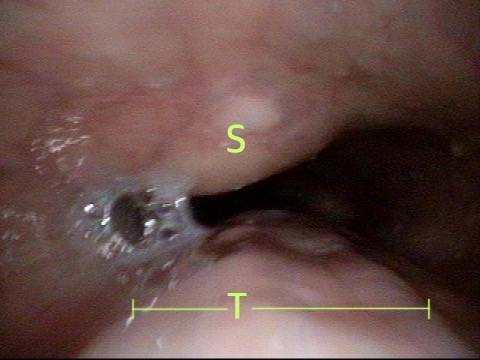
Open Cricopharyngeus Muscle (2 of 3)
Open Cricopharyngeus Muscle (2 of 3)
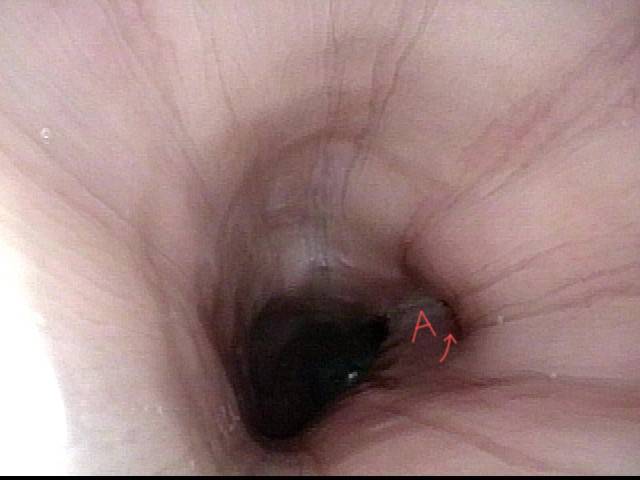
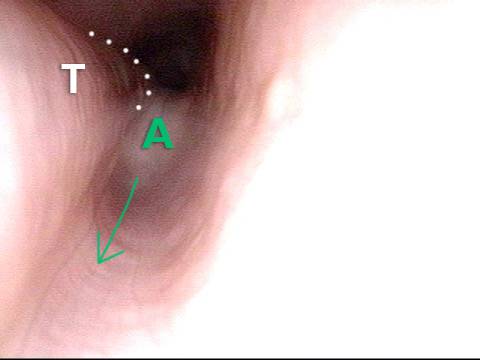
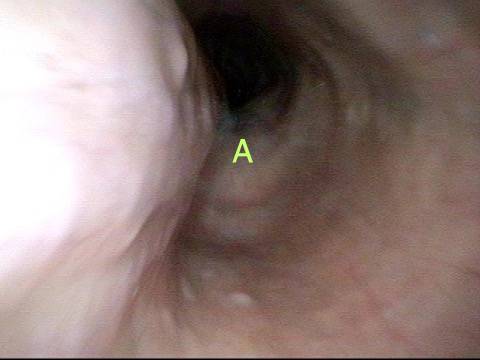
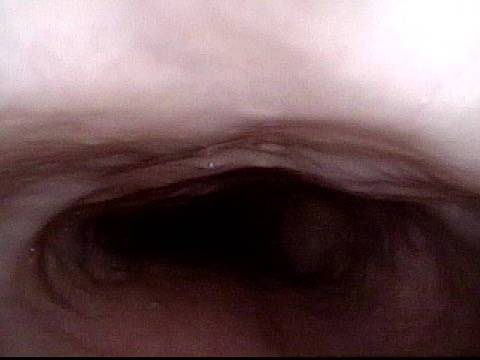
Closed (3 of 3)
Closed (3 of 3)
The person so wants and needs to burp, but continues to experience this inability to burp. Sometimes this can even be painful. Such people often experience chest pressure or abdominal bloating, and even abdominal distention. Flatulence is also severe in most persons with R-CPD. Other less universal symptoms are nausea after eating, painful hiccups, hypersalivation, or a feeling of difficulty breathing with exertion when “full of air.”
Many persons with R-CPD have undergone extensive testing and treatment trials without benefit. R-CPD reduces quality of life, and is often socially disruptive and anxiety-provoking. Common (incorrect) diagnoses are “acid reflux” and “irritable bowel syndrome,” and therefore treatments for these conditions do not relieve symptoms significantly.
Approaches for treating the inability to burp:
For people who match the syndrome of:
- Inability to belch
- Gurgling noises
- Chest/abdominal pressure and bloating
- Flatulence
Here is the most efficient way forward: First, a consultation to determine whether or not the criteria for diagnosing R-CPD are met. Next, a simple office-based videoendoscopic swallow study which incorporates a neurological examination of tongue, pharynx (throat) and larynx muscles and often includes a mini-esophagoscopy. This establishes that the sphincter works normally in a forward (antegrade) swallowing direction, but not in a reverse (retrograde) burping or regurgitating fashion.
Along with the symptoms described above, this straightforward office consultation and swallowing evaluation establishes the diagnosis of retrograde cricopharyngeus dysfunction (non-relaxation).
The second step is to place Botox into the malfunctioning sphincter muscle. The desired effect of Botox in muscle is to weaken it for at least several months. The person thus has many weeks to verify that the problem is solved or at least minimized.
Lifting the CPM for a R-CPD Injection
These are intra-operative photos of one of nearly 1500 persons treated for R-CPD as of September 2023. This sequence shows several things: The dilated, “always open” esophagus distal (below) the muscle; how to identify the cricopharyngeus muscle; and one way of injecting it.
Above the CPM (1 of 5)
Above the CPM (1 of 5)
Ridge of the CPM (2 of 5)
Ridge of the CPM (2 of 5)
Exposed CPM ( 3 of 5)
Exposed CPM ( 3 of 5)
CPM Palpated ( 4 of 5)
CPM Palpated ( 4 of 5)
Botox injection ( 5 of 5)
Botox injection ( 5 of 5)
The Botox injection could potentially be done in an office setting, but we recommend the first time (at least) placing it during a very brief general anesthetic in an outpatient operating room. That’s because the first time, it is important to answer the question definitively, that is, that the sphincter’s inability to relax when presented with a bubble of air from below, is the problem.
Furthermore, based upon an experience with more than 890 patients as of August 2019, a single injection appears to “train” the patient how to burp. Approximately 80% of patients have maintained the ability to burp long after the effect of the Botox has dissipated. That is, long past 6 months from the time of injection.
Patients treated for R-CPD as just described should experience dramatic relief of their symptoms. And to repeat, our experience in treating more than 890 patients (and counting) suggests that this single Botox injection allows the system to “reset” and the person may never lose his or her ability to burp.
Of course, if the problem returns, the individual could elect to pursue additional Botox treatments, or might even elect to undergo endoscopic laser cricopharyngeus myotomy. To learn more about this condition, see Dr. Bastian’s description of his experience with the first 51 of his much larger caseload.
R-CPD, Aerophagia and Burping
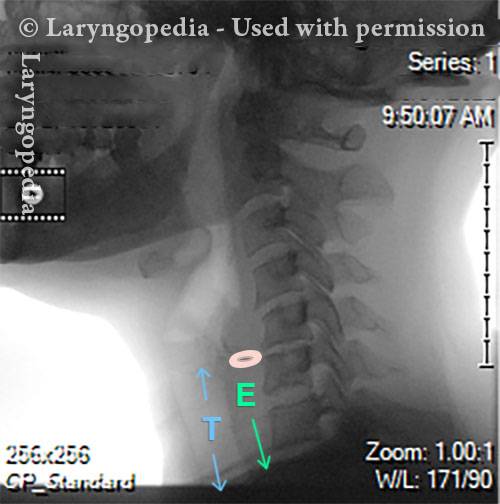
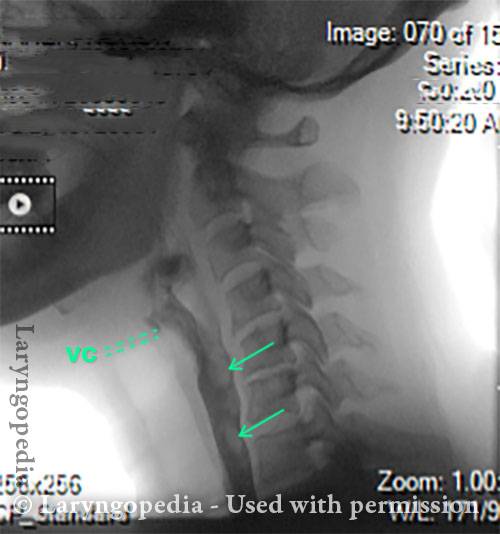
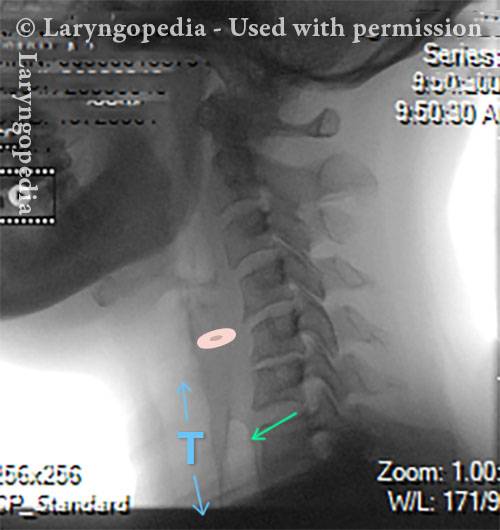
This lateral xray of the neck is part of a swallow studyand illustrates how air can accumulate and need to be burped up. The focus of this post is the esophagus, or “foodway,” that connects the lower part of the throat to the stomach. The esophagus is a muscular tube that remains mostly collapsed—closed—except when food, liquid, or saliva traverses it.
X-Ray of Larynx (1 of 6)
X-Ray of Larynx (1 of 6)
Barium swallow (2 of 6)
Barium swallow (2 of 6)
Collapsed esophagus (3 of 6)
Collapsed esophagus (3 of 6)
Air is swallowed (4 of 6)
Air is swallowed (4 of 6)
UES refuses to open for a burp (5 of 6)
UES refuses to open for a burp (5 of 6)
Abdominal Distention from R-CPD (6 of 6)
Abdominal Distention from R-CPD (6 of 6)
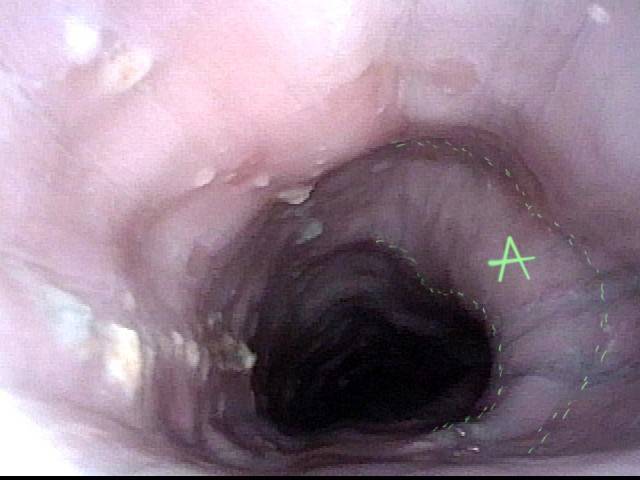
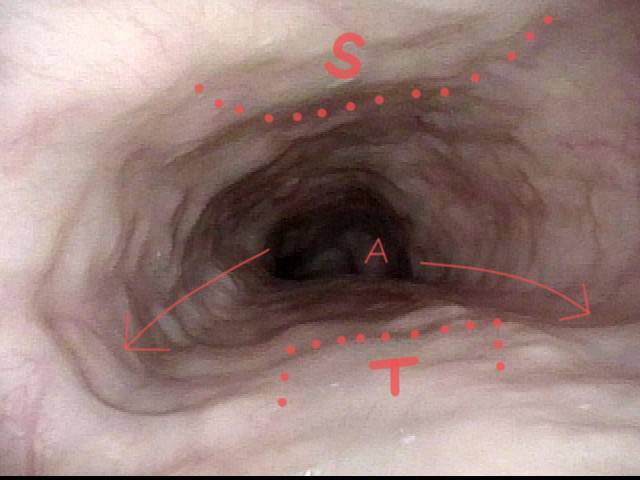
Esophageal Findings
Aortic shelf (1 of 3)
Aortic shelf (1 of 3)
Bony spur emerges due to stretched esophagus (2 of 3)
Bony spur emerges due to stretched esophagus (2 of 3)
Stretched esophagus due to unburpable air (3 of 3)
Stretched esophagus due to unburpable air (3 of 3)
Example 2
Saliva bubbles (1 of 5)
Saliva bubbles (1 of 5)
Symptoms point to GERD (2 of 5)
Symptoms point to GERD (2 of 5)
Pocket in the aorta (3 of 5)
Pocket in the aorta (3 of 5)
Trapped air expands the esophagus (4 of 5)
Trapped air expands the esophagus (4 of 5)
Exaggerated laterally-stretched esophagus (5 of 5)
Exaggerated laterally-stretched esophagus (5 of 5)
Example 3
Stretched Esophagus (1 of 4)
Stretched Esophagus (1 of 4)
Tracheal Wall (2 of 4)
Tracheal Wall (2 of 4)
Over-dilation (3 of 4)
Over-dilation (3 of 4)
Bronchus (4 of 4)
Bronchus (4 of 4)
Dramatic Lateral Dilation of the Upper Esophagus
Remarkable lateral dilation (1 of 3)
Remarkable lateral dilation (1 of 3)
Dilated upper esophagus (2 of 3)
Dilated upper esophagus (2 of 3)
Aortic shelf (3 of 3)
Aortic shelf (3 of 3)
What the Esophagus Can Look Like “Below A Burp”
Baseline (1 of 3)
Baseline (1 of 3)
Pre-burp (2 of 3)
Pre-burp (2 of 3)
Post-burp (3 of 3)
Post-burp (3 of 3)
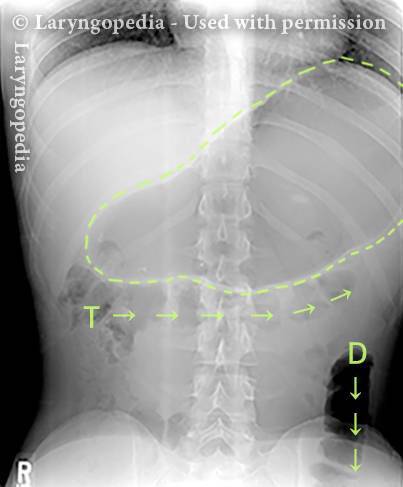
A Rare “abdominal crisis” Due to R-CPD (inability to burp)
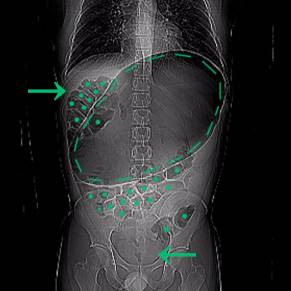
This young man had an abdominal crisis related to R-CPD. He has had lifelong symptoms of classic R-CPD: inability to burp, gurgling, bloating, and flatulence. During a time of particular discomfort, he unfortunately took a “remedy” that was carbonated.
Here you see a massive stomach air bubble. A lot of his intestines are air-filled and pressed up and to his right (left of photo, at arrow). The internal pressure within his abdomen also shut off his ability to pass gas. Watch a video commentary by Dr. Bastian.
X-Ray of Abdominal Bloating (1 of 2)
X-Ray of Abdominal Bloating (1 of 2)
Abdominal Distention of R-CPD
Gastric Air Bubble (1 of 3)
Gastric Air Bubble (1 of 3)
Bloated Abdomen (2 of 3)
Bloated Abdomen (2 of 3)
Non-bloated Abdomen (3 of 3)
Non-bloated Abdomen (3 of 3)
Example 2
This sixty-something man has endured the misery of R-CPD all of his life. His symptoms of inability to burp, gurgling, bloating, flatulence (and more) are dramatically relieved after botulinum toxin into his cricopharyngeus muscle (upper esophageal sphincter). Here, we see the before and after difference in his abdominal distension as well.
Bloating and abdominal distention before botox injection for inability to burp (1 of 2)
Bloating and abdominal distention before botox injection for inability to burp (1 of 2)
Resolved, one month after botox, with burping restored (2 of 2)
Resolved, one month after botox, with burping restored (2 of 2)
Can’t Burp: Progression of Bloating and Abdominal Distention— A Daily Cycle for Many with R-CPD
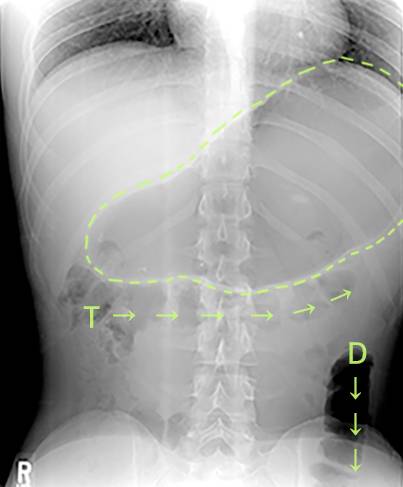
This young woman has classic R-CPD symptoms—the can’t burp syndrome. Early in the day, her symptoms are least, and abdomen at “baseline” because she has “deflated” via flatulence through the night. In this series you see the difference in her abdominal distention between early and late in the day.
The xray images show the remarkable amount of air retained that explains her bloating and distention. Her progression is quite typical; some with R-CPD distend even more than shown here especially after eating a large meal or consuming anything carbonated.
Side view of a bloated abdomen (1 of 6)
Side view of a bloated abdomen (1 of 6)
Front view (2 of 6)
Front view (2 of 6)
Greater Distention (3 of 6)
Greater Distention (3 of 6)
Front view of bloating stomach (4 of 6)
Front view of bloating stomach (4 of 6)
X-ray of trapped air (5 of 6)
X-ray of trapped air (5 of 6)
Side view (6 of 6)
Side view (6 of 6)
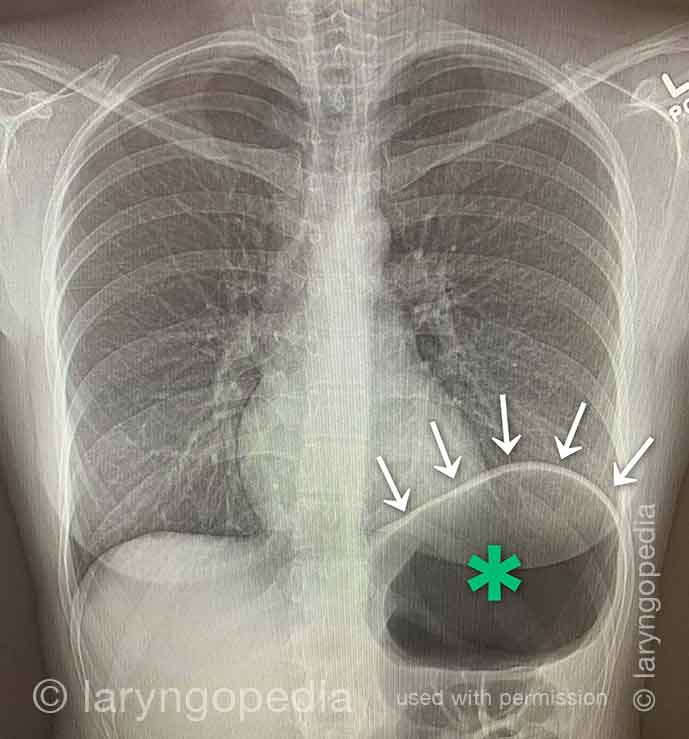
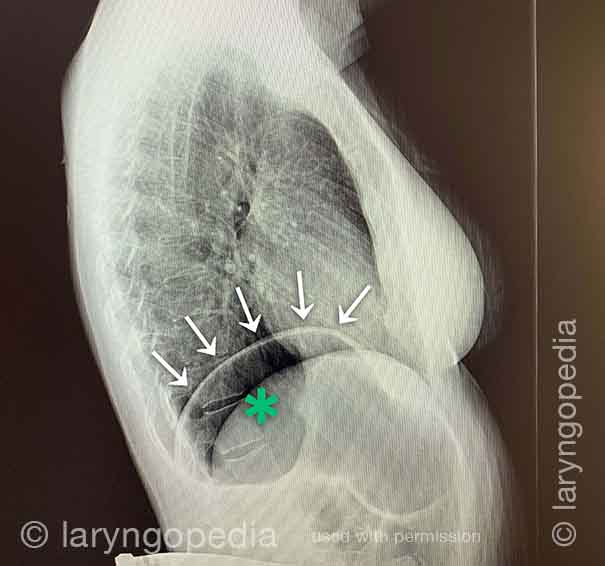
Shortness of Breath Caused by No-Burp (R-CPD)
Persons who can’t burp and have the full-blown R-CPD syndrome often say that when the bloating and distention are particularly bad—and especially when they have a sense of chest pressure, they also have a feeling of shortness of breath.
They’ll say, for example, “I’m a [singer, or runner, or cyclist or _____], but my ability is so diminished by R-CPD. If I’m competing or performing I can’t eat or drink for 6 hours beforehand.” S
ome even say that they can’t complete a yawn when symptoms are particularly bad. The X-rays below explain how inability to burp can cause shortness of breath.
X-ray of trapped air (1 of 2)
X-ray of trapped air (1 of 2)
Side view (2 of 2)
Side view (2 of 2)
What Surprises No-burpers about People who Can Burp
Here are a few things that surprise people who can’t burp, about people who can! (This is especially for those with R-CPD aka no-burp).

R-CPD Panel
A panel of expert discussion on Retrograde Cricopharyngeal Dysfunction (RCPD AKA “No Burp Syndrome”) featuring questions and answers from leaders in the field.
R-CPD (no-burp) Webinar
Live R-CPD (no-burp) Webinar hosted by Dr. Bastian on July 26, 2022 at 6 p.m. CST
R-CPD Q&A—Part I
Dr. Bastian answers a list of questions submitted by our R-CPD Webinar attendees.
R-CPD Q&A—Part II
In Part 2 of the R-CPD Q&A, Dr. Bastian answers a list of questions submitted by our R-CPD Webinar attendees.
Complications Compared to Expected Early Botox Effects in Treatment of R-CPD
Dr. Bastian distinguishes the difference between early EFFECTS that are expected, and COMPLICATIONS patients have experienced in a caseload of approximately 870 people. This informal discussion will likely reassure persons considering this treatment for the severe daily misery caused by R-CPD.