Granulation tissue is tissue that develops as an exuberant “over-healing” response to irritation or injury. This irritation or injury could be due to an endotracheal tube, or a superficial cordectomy wound from surgery, or a number of other causes. Granulation tissue that forms on the posterior vocal cord is called a contact granuloma.
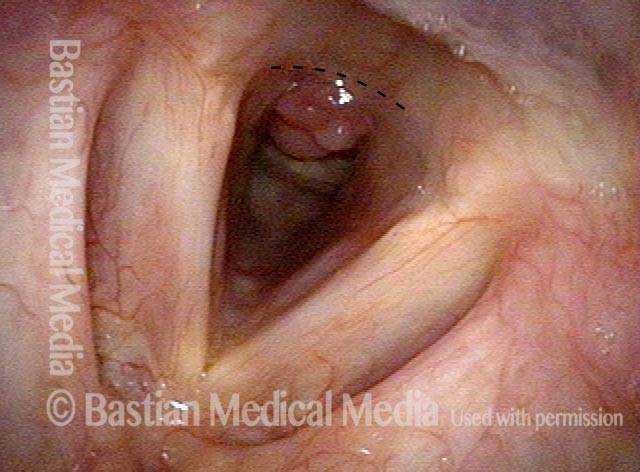
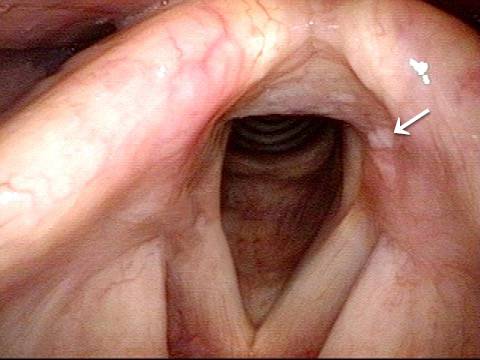
Subglottic granulation and curving airstream
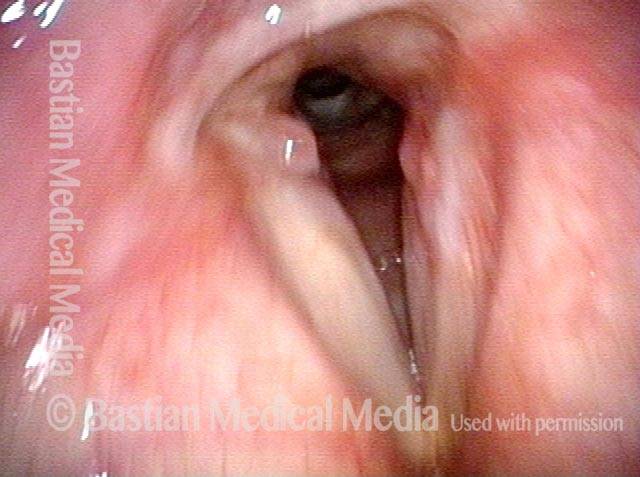
Intubation injury (1 of 4)
Intubation injury (1 of 4)
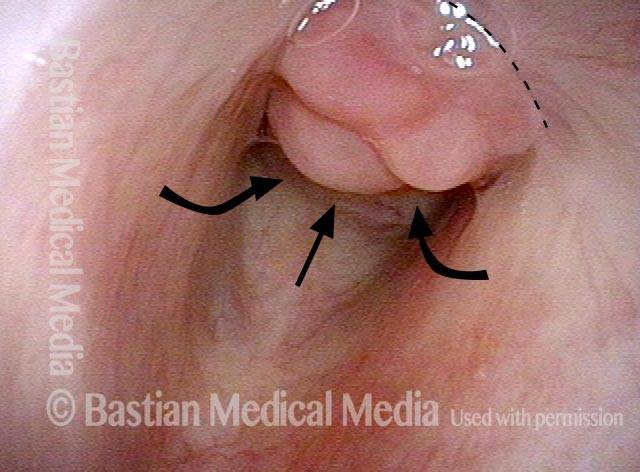
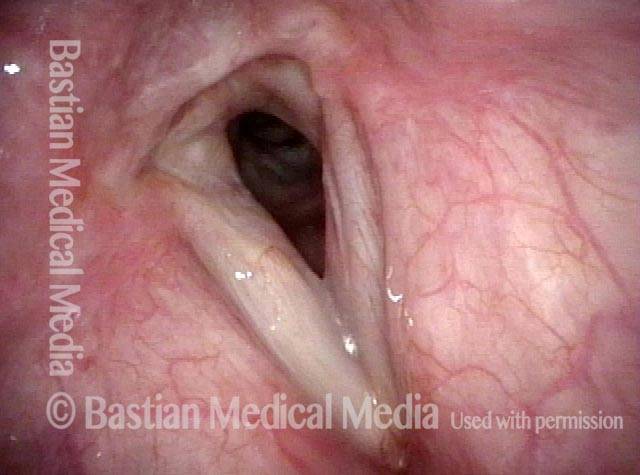
Lobules (2 of 4)
Lobules (2 of 4)
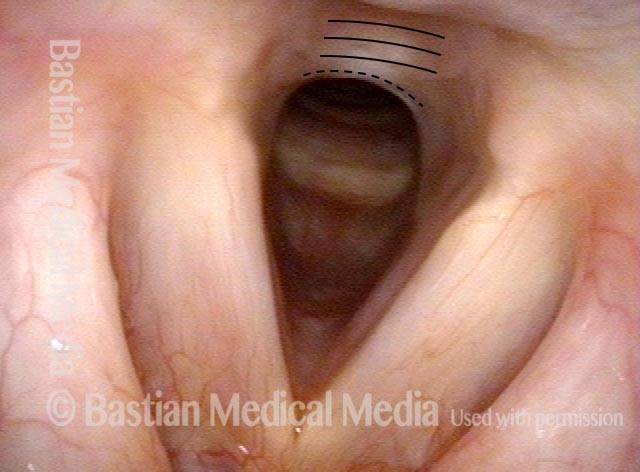
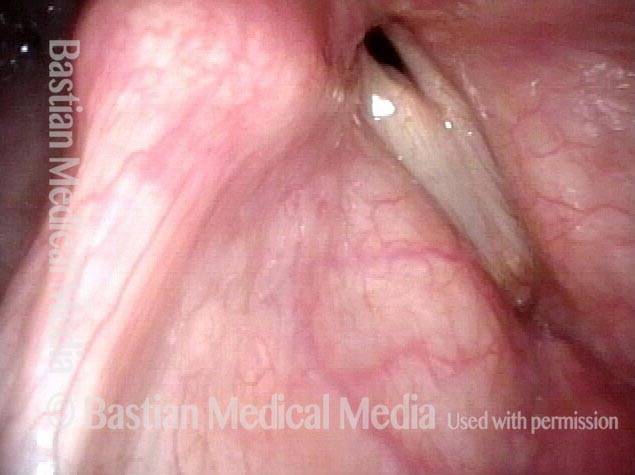
2 months later (3 of 4)
2 months later (3 of 4)
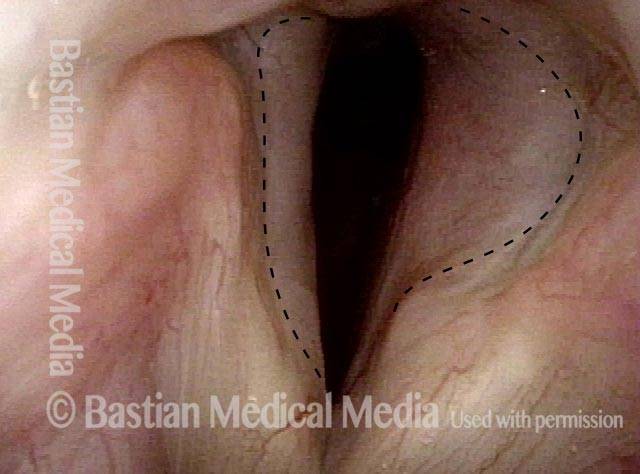
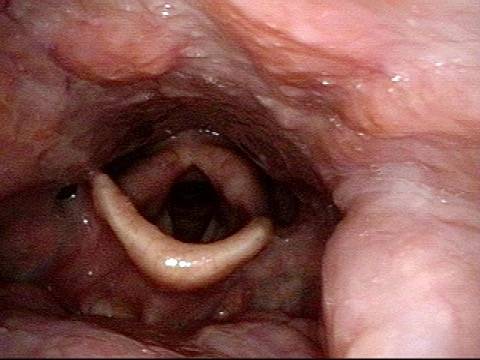
Scar band (4 of 4)
Scar band (4 of 4)
Sometimes you DO remove granulation to avoid tracheotomy
Granulation (1 of 8)
Granulation (1 of 8)
Closer view (2 of 8)
Closer view (2 of 8)
Post microlaryngoscopies (3 of 8)
Post microlaryngoscopies (3 of 8)
Scarring (4 of 8)
Scarring (4 of 8)
Post posterior commissuroplasty (5 of 8)
Post posterior commissuroplasty (5 of 8)
Breathing improved (6 of 8)
Breathing improved (6 of 8)
Closer view (7 of 8)
Closer view (7 of 8)
Phonatory view (8 of 8)
Phonatory view (8 of 8)
Laser surgery for Bilateral Vocal Cord Cancer
Squamous cell carcinoma (1 of 6)
Squamous cell carcinoma (1 of 6)
Tumor on the vocal cords (2 of 6)
Tumor on the vocal cords (2 of 6)
Granuloma delays voice recovery (3 of 6)
Granuloma delays voice recovery (3 of 6)
Closer view of granuloma (4 of 6)
Closer view of granuloma (4 of 6)
Granuloma is smaller (5 of 6)
Granuloma is smaller (5 of 6)
Granuloma doesn't impede voice (6 of 6)
Granuloma doesn't impede voice (6 of 6)
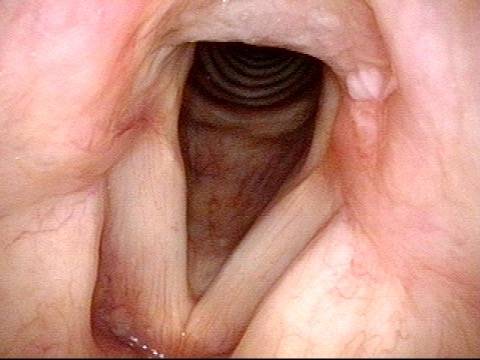
Arytenoid Perichondritis—an Issue of “Festering”
This middle-aged man has had a chronically sore throat on the left for at least 6 months. When asked to indicate where, he doesn’t gesture towards the throat as a whole, but points with one finger to the upper part of the thyroid cartilage fairly far laterally. He doesn’t remember being ill, or any other explanation. After seeing the lesion below, read the introductory article of this post for treatment of this condition.