Videos
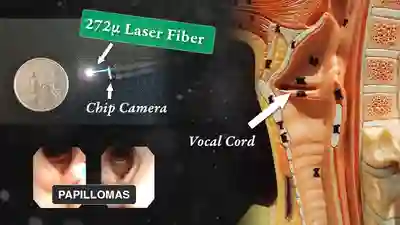
Laser Treatment of Laryngeal Papillomas (RRP)
This man has had RRP (laryngeal papillomas) for many years. He has had laser ablations both in the O.R. under general anesthesia, and in an “office” laser room.
RRP | What Is It? | a.k.a Human Papilloma Virus (HPV)
In this video, Dr. Robert Bastian discusses chronic human papilloma virus (HPV) infection of the larynx (especially vocal cords), causing hoarseness.
This video is designed particularly for those who have been recently diagnosed with a condition called recurrent respiratory papillomatosis (RRP). Those feeling overwhelmed or victimized by this condition are invited to understand the disorder in detail, and what to do about it.
May you feel encouraged by the points of optimism Dr. Bastian explains near the end of his discussion!
The Perfect Patient!!! | Topical Anesthesia for Laryngeal Surgery
This patient is sitting in a chair under topical anesthesia. He is able to minimize movement of his vocal cords, and is therefore a “perfect” candidate for office-based thulium laser ablation of residual laryngeal papilloma.
May you feel encouraged by the points of optimism Dr. Bastian explains near the end of his discussion!

Vocal Cord Injection of Cidofovir
This video portrays a vocal cord injection of Cidofovir following the removal of a papilloma.
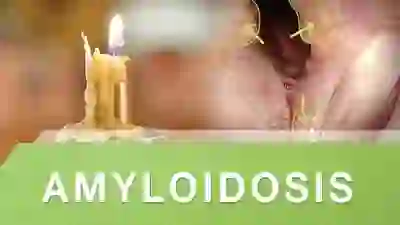
Amyloidosis
A condition in which abnormal proteins (called amyloids) become deposited in the spaces between cells.
In laryngeal amyloidosis, the deposits seem to be localized either just to the larynx, or to the larynx and pharynx. One sees what looks like yellowish candle wax within the tissues. The amyloid deposits are quite firm, and when biopsied, there is little bleeding.

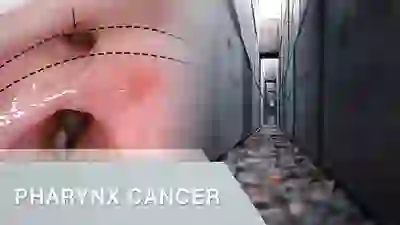
Early Vocal Cord Cancer | Introduction and Treatment Options
This video provides an introduction to early vocal cord cancer (stages 1 and 2) and compares the two main treatment options, laser surgery and radiation therapy.
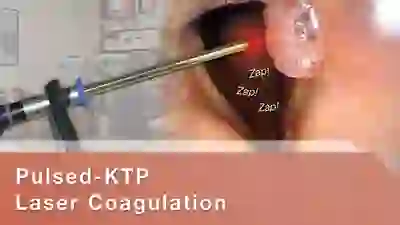
Pulsed-KTP Laser Coagulation of Vocal Cord Papillomas (RRP)
See a video demonstration of laser coagulation of vocal cord papillomas.

Papillomas of the Larynx and Trachea
This video shows wart-like growths in the voicebox and windpipe (larynx and trachea) caused by chronic infection with the human papillomavirus (HPV).
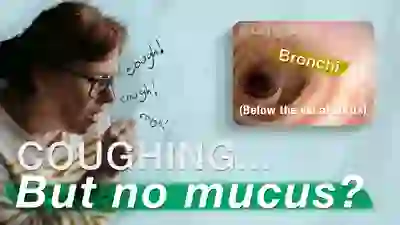
Feel Like Mucus Is Causing Your Cough? Maybe It Is Something Else…
“My cough / throat clearing is caused by mucus! But I’ve tried several “mucus” medicines and they don’t help!” This is a common scenario for persons with sensory neuropathic cough.
Listen to the surprising relationship between “mucus” and sensory neuropathic cough, including illustrations from the stories of actual patients.
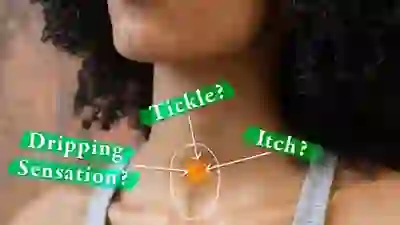
A Sudden Tickle, Itch or Drip in the Throat | Sensory Neuropathic Throat Clearing (SNTC)
Sometimes chronic throat clearing refuses to respond to treatments for allergy, acid reflux, and more. The answer for some persons is an elusive diagnosis called “sensory neuropathic throat clearing” (SNTC). SNTC is caused by sensory neuropathy that creates a very real sensation of tickling, dripping, dryness that in turn initiates repetitive throat clearing.
Persons with SNTC become exasperated with the constant need to throat-clear, and they may annoy family and co-workers. This neurogenic form of throat clearing is often seen together with the highly related sensory neuropathic cough (SNC). Dr. Bastian explains SNTC, which often responds to the same treatments used for SNC.
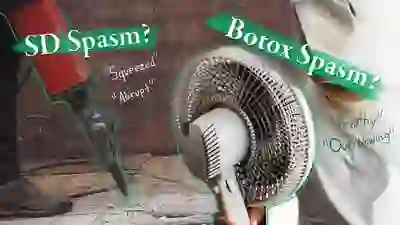
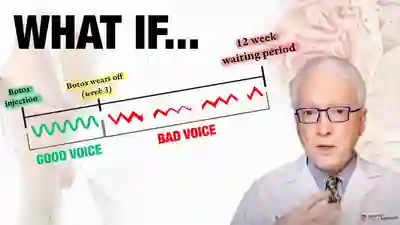
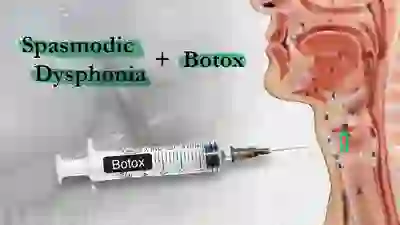
Is My Vocal Weakness from My Spasmodic Dysphonia (SD) Spasms, or Is It A Botox Side Effect?
Persons with Spasmodic Dysphonia (SD) may describe the one of the effects of that disorder as vocal “weakness.” After treatment with Botox, they may use the same word—“weakness”—to describe one of the early side effects of treatment with Botox. Especially after the initial several injections, before they have become treatment “veterans,” some patients struggle to distinguish between these two kinds of vocal “weakness.”
As a result they may have difficulty communicating whether the next Botox injection should be a higher or lower dose. In an attempt to address this problem, this video compares and contrasts the vocal weakness of SD with the (initial) post-injection Botox-related vocal weakness.
Still Coughing After COVID? – SNC
In this video, Dr. Robert W. Bastian explains three explanations for coughing in the context of Covid-19 infection, with emphasis on the potential for sensory neuropathic cough (Phase 3).
The possible phases are:
- During the “hurricaine” of the infection itself, when your lungs may be fighting active and as-yet undefeated virus.
- During the “cleanup phase,” when the virus has been vanquished, but the lung debris (think: “downed branches and detached roof shingles”) is being cleaned up, even though “the sun is shining.”
- For weeks to months after phases 1 and 2 are long past, coughing caused by damaged nerve endings that go “ZING!” with a tickling, burning, dry, or dripping sensation that initiates coughing, throat clearing, or laryngospasm.
This often-overlooked sensory neuropathic type of cough is explained in detail, including how to treat it.
Coughing that Won’t Go Away | SNC – Part I
Sensory neuropathic cough is a chronic cough condition that does not respond to the usual treatments. Many individuals who have been coughing for years find relief from treatment with “neuralgia” medications.

Coughing that Won’t Go Away | Medications – Part 2
Dr. Bastian continues from SNC, Part I and introduces potential medications to treat sensory neuropathic cough.

Coughing that Won’t Go Away | Medications – Part 2
Dr. Bastian continues from SNC, Part I and introduces potential medications to treat sensory neuropathic cough.
Phantom Phlegm!!!
Patients with Sensory Neuropathic Cough (SNC) comment on feeling mucus drip down their throats, but often…it isn’t there! Watch this video to find out about this Phantom Phlegm!
7 Communication Tips for Those with A Weak Voice Especially If the Listener Is Hearing Impaired
The combination of a weak voice in one person and weak “ears” in another can annoy, frustrate, and seriously hamper communication. Hearing aids and “voice building” can be a partial answer. And here are additional tips and pointers that may help two people struggling to communicate:
- Get listener’s attention
- Provide context—a “headline”
- Consider word choice with fewer fricatives/sibilants
- Use duplicate words
- Be aware of loudness setpoint
- O-Ver-ar-Ti-Cu-LaTe!
- Lip read

To Diminish your Voice Problem, Read to Children!
Something to try for your gravelly, tired, or under-energized voice: Reading to Children! As a technique for everyone you talk to!
Asymmetrical Vocal Cord Movement
This person manifests noticeably asymmetrical vocal cord movement. Her diagnosis happens to be sensory neuropathic cough (SNC).

Here Are 3 Simple Exercises to Strengthen A Weak Voice! You only need a few minutes per day…
A weak voice that can’t be heard in noisy places, or that “fades” in quality and strength across a day can be frustrating!
There is a long list of potential explanations. A common one is weak, atrophied, flaccid vocal cord—and other vocal tract—muscles. When this is the cause for a weak voice determined by medical evaluation, voice strengthening is the first place to start.
In this video, Dr. Bastian provides background information about muscle strengthening in general, and why vocal muscles can weaken in some people.
He then suggests a simple voice strengthening strategy consisting of three exercises, taking no more than 60 seconds to complete. For many people, this DIY regimen can be sufficient by itself. If not, it can prepare you for further work with a speech pathologist or laryngologist. For those who want to skip straight to the three voice strengthening tasks, begin viewing at 5:28

Here Are 3 Voice Building Strategies for Parkinson’s Disease
Persons with Parkinson’s Disease (PD) often develop weak, even whispery voices. The explanation is not only a weak mechanism (primarily muscles), but also PD’s reduction of the inner vitality that “energizes” voice and speech.
This video outlines a rationale and strategy for voice building designed specifically for PD. The two fundamental ideas are to challenge the muscles of voice and speech, and also to “rev the engine” of the voice. Simple at-home exercises are explained that the affected individual and family/friends can easily master.
Along with expert medical / pharmacological management, a trial of this sort is appropriate before considering anything else (like vocal cord implants)
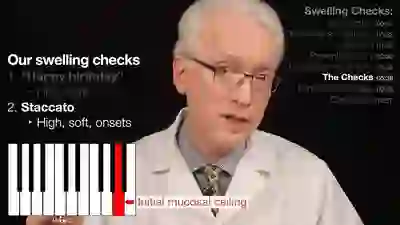
Vocal Cord Swelling Checks: A Simple Way to Detect the Early Signs of Vocal Injury
Vocal cord swelling checks can help prevent a chronic vocal injury. The swelling checks, which are a pair of short, simple vocal exercises, help you to monitor the health of your vocal cord mucosa and detect the presence of any possible swelling, which could be the beginning of a potentially more serious vocal cord injury. By performing these checks twice a day every day, you can hopefully respond quickly to any warning signs and avoid the need for treatment down the road.
In this video, Dr. Bastian explains more fully how vocal injury might occur, he introduces and demonstrates the two swelling checks he recommends, and he discusses the long-term strategy for incorporating these checks into your daily routine.

Functional Dysphonia (Nonorganic): A Cause for Unexplained Voice Loss
This video gives an example of a patient who had been having a voice problem for several months. The clinician discovered that her voice problem was a nonorganic voice disorder, also called functional dysphonia. This kind of disorder is caused not by any abnormality of the larynx’s physical structures, but instead by an abnormal use of those physical structures.
You will see what the larynx looks like when a person with this kind of disorder makes voice, you will hear the clinician beginning to coax out the patient’s normal voice, and you will hear the patient learning to control this re-discovered normal voice.

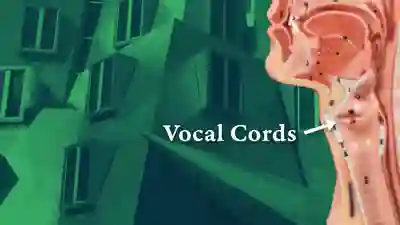
Introduction to Larynx, Pharynx, and Airway Anatomy
In this presentation Dr. Robert Bastian provides an introduction to larynx, pharynx, and airway anatomy. This information is meant to serve as an educational resource.
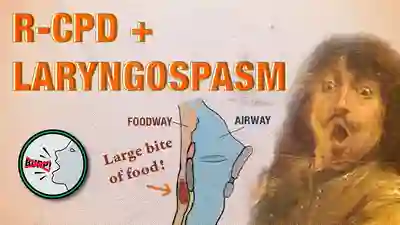
Laryngospasm after Botox Injection for R-CPD – How to Avoid It
Persons with no-burp, aka retrograde cricopharyngeus dysfunction (R-CPD) can usually learn to burp with the help of a single botulinum toxin (botox) injection (“once and done” in about 80%). The diagnosis and treatment are remarkably straightforward.
BUT…about one of 200 or so experience laryngospasms after the treatment and this is a source of anxiety for some considering the procedure. This video explains why laryngospasm occasionally occurs in this scenario and how to avoid it.
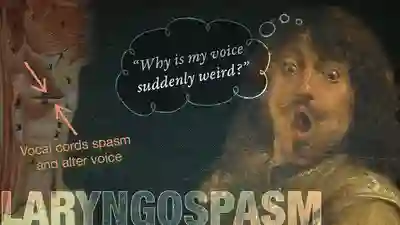
Laryngospasm of Voice | Sudden, Brief Change in Voice
From one second to the next, my voice changes suddenly…it almost goes away for a minute or so, and then is back to normal quickly.” That might be the comment of someone with “laryngospasm of voice.” This video explains this uncommon but frustrating disorder.
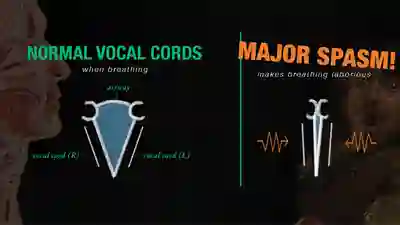
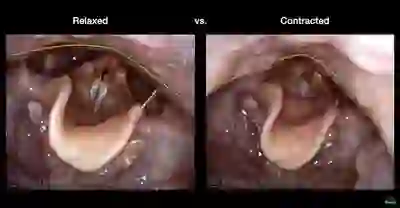
Laryngospasm: Sudden, Terrifying Difficulty Breathing
Dr. Robert Bastian of Bastian Voice Institute explains laryngospasm with video of the larynx and a simulated attack.
Laryngospasm is a sudden, often severe attack of difficulty breathing, typically lasting between 30 and 90 seconds. Usually the individual makes a frightening noise while trying to breathe in during the episode, which they often call a “choking attack. You will hear the types of noises often made by the person experiencing laryngospasm, and see what the vocal cords are doing at the same time.
Laryngospasm – Straw Breathing Part 2 | Sensory Neuropathic Cough
Laryngospasm is a sudden, often severe attack of difficulty breathing, typically lasting between 30 and 90 seconds. Usually the individual makes a frightening noise while trying to breathe in during the episode, which they often call a “choking attack.”
In this video, Dr. Bastian explains a simple procedure — straw breathing — that can be used by individuals suffering an attack.

Can’t Burp? This May Explain Why | R-CPD – Retrograde Cricopharyngeus Dysfunction, Inability to Burp
Can’t burp and feeling miserable? You may have R-CPD or retrograde cricopharyngeus dysfunction.
In this condition, the upper esophageal sphincter (cricopharyngeus muscle) works normally from above to permit swallowing, but it refuses to relax from below to let air be belched out.
This inability to belch causes severe daily misery due to socially-awkward gurgling noises, bloating (abdominal and/or chest and/or neck pressure), and excessive (often “ridiculous”) flatulence.
Dr. Robert Bastian of Laryngopedia (teaching website) and Bastian Voice Institute (clinical – patient care offices) explains this “noburp” condition in detail, based on experience with over 1,000 patients.
Fear of Vomiting and R-CPD | What Can You do About Emetaphobia?
Some people experience exaggerated and even debilitating fear of vomiting. They may panic at the very thought, and require psychotherapy. The term for this is emetophobia, and it occurs in perhaps one person per thousand of the general population.
But it may occur far more frequently—in as many as one of three persons—who have a condition called retrograde cricopharyngeus dysfunction (R-CPD, aka “no-burp”). Dr. Bastian explains why this might be, and what effect the successful treatment of R-CPD may have on emetophobia.
What is the Relationship between R-CPD (no-burp) and GERD? SIBO? IBS?
Often, and almost routinely, persons with easily-diagnosed R-CPD may initially be diagnosed instead as “gastroesophageal reflux disease” (GERD), or “irritable bowel syndrome,” (IBS) or “small intestine bacterial overgrowth” (SIBO).
Do GERD, IBS, and SIBO symptoms and findings point to coexisting and separate diagnoses, or are those symptoms part of the larger, umbrella diagnosis of R-CPD? Dr. Bastian discusses these questions in this video.

How to Keep (if possible) the Ability to Burp After Botox Treatment for R-CPD
Inability to burp (aka R-CPD or no-burp) can thankfully be treated successfully with a simple outpatient injection of Botox into a muscle in the upper esophagus. Since the Botox effect on the muscle serves as “training wheels” for burping, about 4 out of 5 people are “cured” by a single treatment. That’s why we aim for “once and done” treatment.
In this video, Dr. Bastian describes here how to maximize the likelihood that the ability to burp will continue after Botox has worn off.
RCPD Workup – Do You Need Testing for a Diagnosis?
What is necessary to diagnose R-CPD? What is sufficient? Do we need to spend thousands of dollars for x-rays, manometry, upper GI scopes, gastric emptying studies?
Here’s Dr. Bastian’s opinion after successful diagnosis and treatment of his personal caseload of nearly 1000 persons with R-CPD.
What Surprises No-burpers (R-CPD, inability to burp) about People who Can Burp
Here are a few things that surprise people who can’t burp, about people who can! (This is especially for those with R-CPD).
What Surprises No-burpers (R-CPD, inability to burp) about People who Can Burp
Your questions answered! The subject: R-CPD. Dr. Bastian responds to a list of questions submitted through YouTube, Facebook, and Instagram.
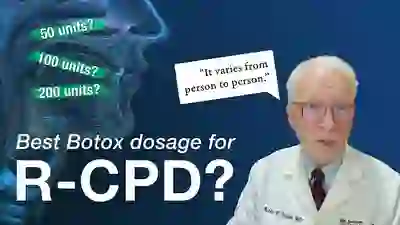
What is the Right Amount of Botox for R-CPD? 100 units? 50? 200?
The newer disorder called R-CPD (No burp) was originally described in 2019 by Bastian and Smithson. Both diagnostic criteria and details of successful treatment with botulinum toxin (‘botox’) were included in that report. Many doctors worldwide are now helping persons with this terrible affliction. But is dose the reason a small number don’t respond as well?
Newly diagnosed patients often ask: “What is the best dose for the initial injection of Botox?” Dr. Bastian provides an answer that includes context and nuance from his group’s experience with over 1400 patients injected to date.
Feeling Nauseated? Symptoms of R-CPD (the Inability to Burp)
Unexplained nausea is the subject of this video. R-CPD (retrograde cricopharyngeus dysfunction) is a disorder that causes inability to burp, gurgling, bloating, flatulence, hiccups, and in some people, NAUSEA.
Dr. Bastian explains that nausea can for some be the “doorway” to discover that they have R-CPD. This video summarizes the syndrome, and ends with an anecdote of a young woman who struggled with nausea for years, only to have it finally relieved via treatment of her R-CPD.
Do Shaker Exercises Work in Treating R-CPD? (inability to burp, no burp)
In this video, Dr. Bastian explains his thinking about “Shaker Exercises” as a means of learning to burp in persons with R-CPD (no-burp). A recent Reddit thread was created in response to his July 2022 Webinar comments on this subject, and it appeared to him that he had not conveyed his thinking clearly enough. Here is his more detailed and nuanced discussion…
Can’t Burp? Dr. Bastian answers your questions about R-CPD
Dr. Bastian answers a list of questions submitted by our R-CPD Webinar attendees.
Can’t Burp? Dr. Bastian Answers Common Questions About R-CPD | Part 2
In Part 2 of the R-CPD Q&A, Dr. Bastian answers a list of questions submitted by our R-CPD Webinar attendees.
Complications Compared to Expected Early Botox Effects in Treatment of R-CPD
People ask: “What could go wrong, if I receive a botox injection for my inability to burp and associated symptoms caused by retrograde cricopharyngeus dysfunction (R-CPD)?”
In this video, Dr. Bastian distinguishes the difference between early EFFECTS that are expected, and COMPLICATIONS patients have experienced in a caseload of approximately 870 people. This informal discussion will likely reassure persons considering this treatment for the severe daily misery caused by R-CPD.
R-CPD in X-ray Images | Misery vs. Crisis from Inability to Burp
Why do persons with R-CPD experience such daily misery? These X-ray images provide the explanation, as well as the rare “abdominal crisis” in this group is also explained.
In a new video format, Dr. Bastian will discuss various photo essays found across Laryngopedia, and provide in-depth descriptions on their origins and what is going on behind the scenes during the time of capture.
Can’t Vomit? Symptoms of R-CPD (the Inability to Burp)
Nobody likes to vomit. Yet, imagine being unable to vomit if food poisoned… Or having to retch and heave for a long time without success before it finally happens with a herculean effort. Understandably, persons in these groups may develop a phobia of vomiting (emetophobia).
Inability to vomit can be part of a treatable larger syndrome, called R-CPD (retrograde cricopharyngeus dysfunction). R-CPD is explained.
Excessive Flatulence | Symptoms of R-CPD
The purpose of this video is to introduce those with excessive flatulence (gassiness) to a potential explanation they may not have encountered before: retrograde cricopharyngeus dysfunction (R-CPD).
Persons with R-CPD typically say that in addition to flatulence, they can’t burp, experience socially-awkward gurgling noises, and experience abdominal bloating. Treatment of R-CPD can dramatically reduce flatulence in this group of persons.

My Baby Can’t Burp! This May Explain Why..
“My baby can’t burp!”
“He/she cries with colic, sometimes for a long time.”
“So much spitting up and even projectile vomiting!”
“I’ve never seen such a gassy baby!” Babies and older children with this condition are in misery, and so are their parents, with the stress of it all. The answer might be a dysfunction of the upper esophageal sphincter (Retrograde CricoPharyngeus Dysfunction, or R-CPD).
When such babies grow older, those with severe cases of R-CPD may refuse to eat, and may continue to complain of stomach distress.
In this video, Dr. Robert Bastian explains this “new” diagnosis that can cause all of these symptoms. Parents who are exhausted and depressed may find here a glimmer of hope.
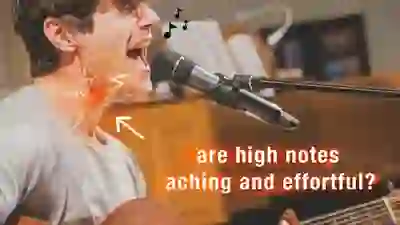
Loss of Upper Voice Caused by Lowered Muscular Ceiling (MTD)
Every voice has a natural range (from its “floor” to its “ceiling”), often 2 ½ octaves or more. Over time, some singers notice upper range loss or effortfulness (the ceiling descends). Yet there are no nodules or polyps.
When the “muscular ceiling” descends, it feels and sounds like the voice has to be pushed up to its upper range and the throat may almost ache with the effort. And pitch may sag.
A common association in women is menopause, but it can be seen in either sex at any age. Dr. Bastian is not a voice teacher but offers insights from his work as a laryngologist with hundreds of singers.
Why Botox Injections for Spasmodic Dysphonia (SD) Should Be Individualized
Should Botox injection dosage and interval for your Spasmodic Dysphonia be decided by you and your doctor? Or should a “checklist,” created by someone who doesn’t know you, determine what you and your doctor may and may not do?
Here’s a discussion, and patient examples, that explain the crucial importance of the former approach of freedom of choice and individualization!

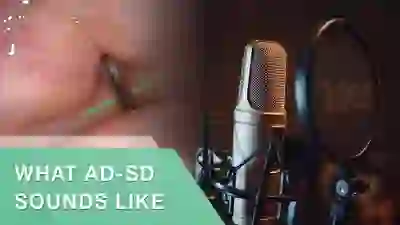
Dropped Syllables? Catches in Your Voice? | Adductory Spasmodic Dysphonia (AD-SD)
A strained voice, usually with “catches” or dropped syllables or words, may be the result of a rare neurological condition called adductory spasmodic dysphonia (AD-SD). Abnormal muscular tone in vocal cords (laryngeal dystonia) results in abnormal vocal sound (spasmodic dysphonia).
This video explains the disorder. Current standard of care is botox, which can dramatically diminish symptoms with 3 or 4 treatments per year.
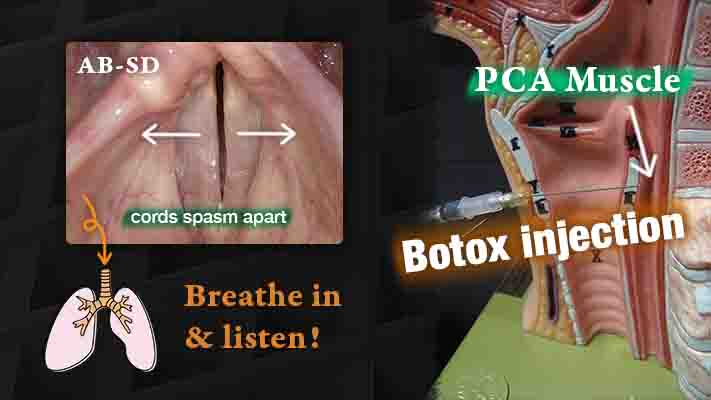
Vocal Cords Spasm Apart? | Abductory Spasmodic Dysphonia (AB-SD)
Syllables or words drop away to a whisper when a person is afflicted by the less common variant of a neurological disorder called AB-ductory spasmodic dysphonia (AB-SD) Due to its effect on speech, it is sometimes called “intermittent whisper dysphonia.”
In this video you will find a description of the disorder, its treatment with botox, and how to assess for proper dosage and placement of this medication.
Respiratory Dystonia | When Spasms Affect the Voice
In a peculiar disorder of breathing, “respiratory dystonia,” tiny spasms in the vocal cords prevent the smooth in- and out-flow of air to the lungs. It is as though the air comes in or goes out in little pieces rather than in a unified inspiration or expiration.
Quiet involuntary noises are heard from the throat, most often while trying to breathe in, and sometimes tiny “grunts” when breathing out.
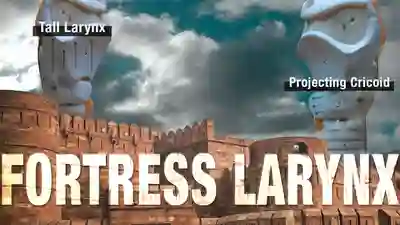
Botox Injection Into the “Fortress Larynx” for Spasmodic Dysphonia
High quality Botox shots for spasmodic dysphonia (SD) can be defined as:
- Available on demand.
- Accomplished efficiently and with minimal discomfort.
- Providing consistent results.
Numbers 2 & 3 can be difficult to impossible when the patient has a “fortress larynx.“ In this video, we define this problem and a possible solution…

Voice Drops or Sounds Breathless? AB-SD Phenomenology
Adductory Spasmodic Dysphonia – Tonic Variant
Adductory spasmodic dysphonia is a variant of spasmodic dysphonia in which the spasms push the vocal cords together, choking off or straining the voice. There are two variants of adductory spasmodic dysphonia: classic and tonic.
In the classic variant, the adductory spasms of adductor spasmodic dysphonia are intermittent, each time clamping the vocal cords together momentarily, so that words or syllables in a person’s speech are intermittently choked out.
In the tonic variant, the adductory spasms are more constant and sustained than intermittent, so that instead of interrupting the person’s speech, the spasms cause a constant strained or “tight” vocal quality.
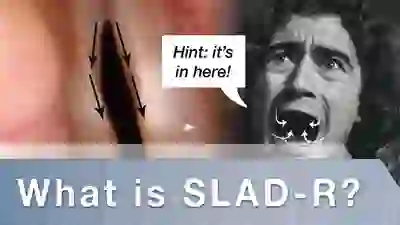
One Man’s Experience Over Time with SLAD-R (Selective Laryngeal Adductor Denervation-Reinnervation)
SLAD-R is a surgical alternative to ongoing “botox” injections for treatment of adductory spasmodic dysphonia. The surgery involves intentionally cutting the nerves that close the vocal cords for voice and reconnecting a different nearby nerve supply (reinnervating the nerves).
This surgery requires the patient’s willingness to endure an extremely breathy voice for many months after the procedure, while awaiting reinnervation.
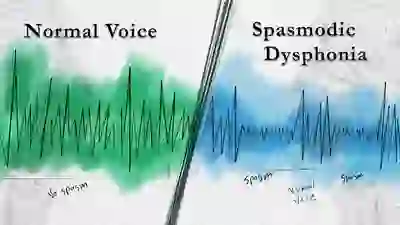
Spasmodic Dysphonia | A Peculiar Voice Disorder – Part 1
In this video, Dr. Robert Bastian reviews the various types and subtypes of a rare neurological voice disorder called spasmodic dysphonia (SD). Numerous voice examples are included, along with video of the vocal cords.
SD is a rare neurological disorder caused by laryngeal dystonia, and it interferes with the smooth functioning of the voice. Tiny spasms of the vocal cords may cause the voice to catch or cut out, strain or squeeze away, and sometimes to drop momentarily to a whisper. Those watching this tape will hear examples of the many types of SD.
Spasmodic Dysphonia | When Botox Disappoints – Part 2
In this video, Dr. Bastian discusses common problems with Botox treatment for spasmodic dysphonia (SD). He delivers clear, practical advice that can be used to increase the effectiveness of Botox treatments for SD.

Vocal Money – Recovering from Vocal Cord Injury
Individuals who develop chronic vibratory injuries of the vocal cords, such as nodules and polyps, can be thought of as having been vocal overspenders. And so, conceptualizing voice use as spending vocal money can provide a helpful analogy for those rehabilitating from their injuries.
The idea is to think of having vocal money to spend every day, and to manage the amount, manner, and spacing of expenditure, in order to get out of the vocal debt of vibratory injury.

Voice Use after Vocal Cord Microsurgery
Vocal cord microsurgery is reserved for “otherwise irreversible” injury. The risk is low if done well, and the benefit to voice can be major.
But what is the blueprint for resumption of voice use (speaking and, if one is a singer, singing) after vocal cord microsurgery? Listen for a recommended plan.
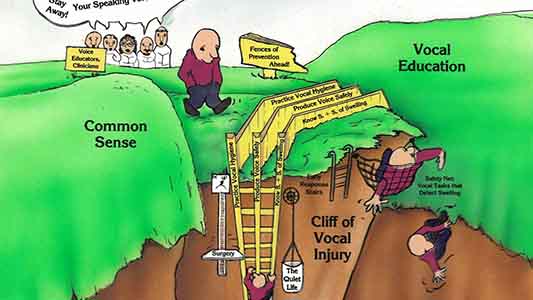
An Illustration of Vocal Cord Injury Prevention by Dr. Robert Bastian
When it comes to vocal cord injury, “It is better to build a fence at the top of a cliff than to park an ambulance at the bottom.” Prevention of injury is the point of Dr. Bastian’s tour of a cartoon he had drawn years ago.
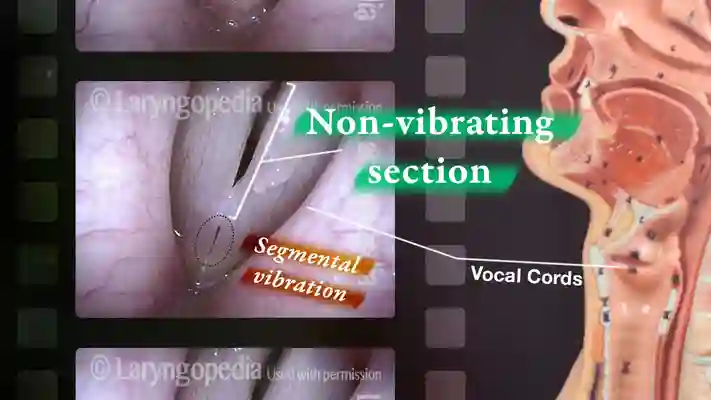
Tin Whistle Segmental Vibration of the Vocal Cords
A squeaking or “tin whistle” voice can be evidence of nodules or other vocal cord injury of overuse.
Background: normal vocal cords vibrate along their entire length even at very high pitch. When nodules or polyps stop vibration in the mid-cord, a tiny (usually anterior) segment may continue to vibrate, creating and equally tiny “tin whistle” quality.
This video explains the difference between full-length and segmental vibration of the vocal cords, with excellent audio and video (vocal cord) strobe light illustrations of both kinds of vibration.
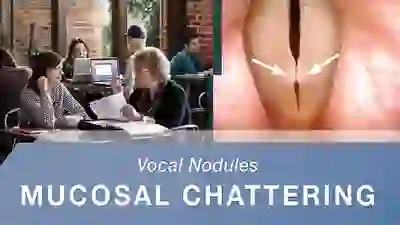
Vocal Cord Nodules – What Do They Sound Like? | Mucosal Chattering
In this video, Dr. Bastian makes extensive use of elicitation with his own voice in order to hear the “vocal phenomenology” of a voice under evaluation. He has named one phenomenon he has not heard described elsewhere as mucosal chatter.

A Halloween Shriek!!!
Segmental vibration refers to the creation of a very tiny, clear sound that cannot be swelled or crescendoed without some kind of a “squawking” adjustment of the vocal folds. When the sound occurs, only a short segment of the vocal folds is vibrating rather than their full length. Segmental vibration is most often heard in people who have nodules or polyps.

Capillary ectasia (including KTP laser treatment)
Capillary ectasia is the enlargement or dilation of capillaries on the surface of the vocal cords. At our practice we believe capillary ectasia is a manifestation of vocal overuse, and a response to ongoing injury of the vocal cords. Once established, capillary ectasia may cause symptoms of reduced vocal endurance and exaggerated premenstrual huskiness.
Capillary ectasia may also increase the risk of vocal cord bruising (hemorrhage) and hemorrhagic polyp formation. Capillary ectasia is easily corrected via vocal cord microsurgery.

Smoker’s Polyps (aka Polypoid Degeneration or Reinke’s Edema)
Smoker’s polyps, also known as polypoid degeneration or Reinke’s edema, refers to diffuse swelling of the vocal cords, due to build-up of edema fluid within the vocal cord mucosa. This condition is most often seen in long-term smokers who are also somewhat talkative.
This video illustrates how smoker’s polyps can be seen more easily when the patient makes voice while breathing in (called inspiratory phonation). During inspiratory phonation, the polyps are drawn inward and become easier to identify.
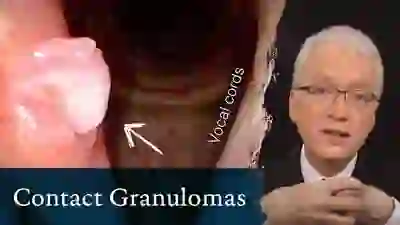
Contact Granulomas (or Contact Ulcers)
In this video, Dr. Bastian provides an introduction to contact granulomas. A contact granuloma (or contact ulcer) is a mass or lump of chronically irritated tissue that is best thought of as “exuberant healing response that didn’t know when to quit.”
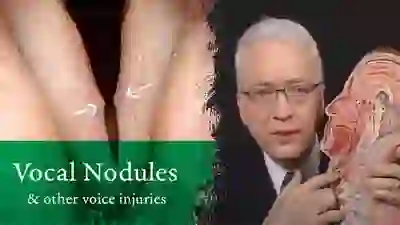
Nodules and Other Vocal Cord Injuries | How Do They Occur and Can They Be Treated?
This video explains how nodules and other vocal fold injuries occur: by excessive vibration of the vocal cords, which happens with vocal overuse. Having laid that foundational understanding, the video goes on to explore the roles of treatment options like voice therapy and vocal cord microsurgery.
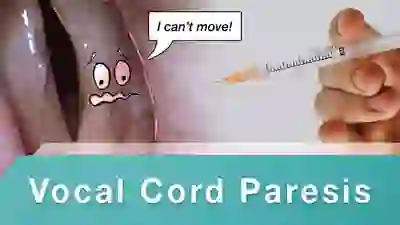
Injection Medialization for Vocal Cord Paresis
In this video, see an example of vocal cord paresis (a kind of “partial paralysis”) and how it limits the voice. Then watch an injection medialization procedure in which voice gel is injected into the vocal cord affected by paresis, and hear how the voice thereafter improves.
Mucus Retention Cyst | Before and After – Part 1
A mucus retention cyst is a type of cyst that forms on the vocal cord when one of the mucus glands just below the free margin of the vocal cords becomes plugged, trapping the mucus secreted by that gland.
A common symptom is hoarseness. Whereas many other vocal cord lesions arise from vocal overuse, mucus retention cysts seem to arise spontaneously, without any necessary correlation to how the voice is used.

Mucus Retention Cyst | Before and After – Part 2
This is our second video that features a mucus retention cyst, before and after surgical removal.
A mucus retention cyst is a type of cyst that forms on the vocal cord when one of the mucus glands just below the free margin of the vocal cords becomes plugged, trapping the mucus secreted by that gland. A common symptom is hoarseness. Whereas many other vocal cord lesions arise from vocal overuse, mucus retention cysts seem to arise spontaneously, without any necessary correlation to how the voice is used.
Hemorrhagic Vocal Cord Polyp: Before and After
Watch the story of a young man with a hemorrhagic vocal cord polyp. Listen to his voice and see his larynx both before and after surgical removal.

Glottic Sulcus: Laryngeal Video Stroboscopy
Glottic sulcus refers to a degenerative lesion consisting of the empty “pocket” of what was formerly a cyst under the mucosa of the vocal cord. The lips of the sulcus may be seen faintly during laryngeal stroboscopy. Or, vibratory characteristics may suggest this lesion.
The lesion may be overlooked unless one is familiar with this entity. To paraphrase eminent French laryngeal microsurgeon Dr. Marc Bouchayer, these lesions are diagnosed much more frequently once you know about them than before. At present, aside from having the patient coexist peacefully with this problem via voice therapy and other measures, surgery is the primary treatment modality.
What Happens When You Burp? A Look Inside the Throat
VESS (Videoendoscopic Swallowing Study)
A method of evaluating a person’s swallowing ability by means of a video-documented physical examination, looking from inside the throat. Also called the fiberoptic endoscopic evaluation of swallowing (FEES).
What Happens When You Laugh? A Look Inside the Throat
Have you ever wondered what your body actually does to laugh? This video shows the internal view of the vocal cords on a patient who is laughing and was placed online at his request.
100-year-old Swallow! (Videoendoscopic Swallowing Study)
The videoendoscopic swallowing study (VESS) is a method of evaluating a person’s swallowing ability by means of a video-documented physical examination, looking from inside the throat. Also called the fiberoptic endoscopic evaluation of swallowing (FEES).
This video features an example of a 100-year-old patient undergoing a VESS.
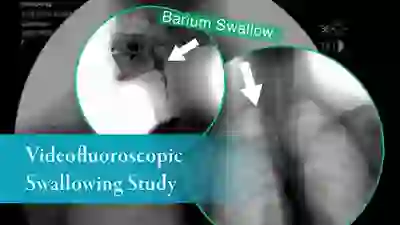
Barium Swallow (Barium Esophagram: Anterior-Posterior View)
This video presents a clear visual example of a barium swallow, a test that involves having the patient swallow a barium solution while using x-rays to observe the flow of the barium, which can reveal swallowing deficiencies.
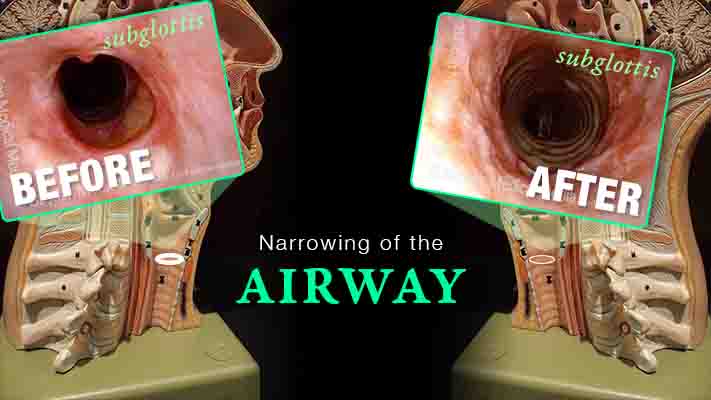
Inflammatory Subglottic Stenosis | Definition, Symptoms, and Treatments
Are you experiencing gradual onset of noisy, even effortful breathing? One uncommon but important explanation is idiopathic, inflammatory subglottic stenosis. That just means “unknown cause, likely autoimmune narrowing just below the vocal cords and at the highest part of the windpipe.”
This video explains the disorder and its management, shows “before” and “after” photos, and reassures viewers that if yours is the usual case, there doesn’t seem to be any effect on general health or lifespan.
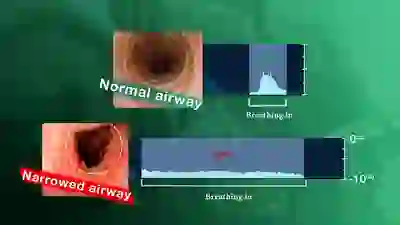
Trouble Breathing? How to Hear a Narrow Airway due to Tracheal Stenosis
A narrowing anywhere in the breathing “pipe” that leads to the lungs causes shortness of breath, typically with harsh inspiratory noise on exertion. Such a narrowing can follow injury, intubation, cancer treatment, auto-immune disorders, etc.
It is possible to gain an immediate understanding of the magnitude of the airway narrowing within minutes by using a simple test “graded” with one’s ears.
The severity of the problem can be understood before any examination or X-ray evaluation. Dr. Bastian explains…
Inspiratory Phonation – How marginal is this airway?
This video demonstrates involuntary inspiratory phonation; a vocal phenomenon in which an involuntary vocal sound is made when one breathes in.
In the video, the physician “shares” the patient’s airway with a flexible scope in order to determine the degree to which the airway is marginal. By “sharing” the airway, the patient concludes the following:
- That inspiratory noise is louder while sharing the airway.
- More importantly, that inspiration takes longer.
- That the patient’s airway is marginal but not dramatically so; emergency intervention is not needed.
- That what we have just seen/ heard correlates exactly with the patient’s description of degree of exercise intolerance.
Abrupt Feeling of Air Hunger? GASPING SYNDROME
This video is for those who fulfill four criteria:
- They experience abrupt feelings of air hunger, with or without exertion.
- Deep breaths in response to the feeling of “needing air” are not noisy and it doesn’t take longer to fill your lungs than for the other people in your life.
- Your doctors cannot find an explanation despite running a considerable number of “heart and lung” tests.
- All treatments tried are ineffective in abolishing the problem.
See if this video describes you!
Suction Drain as A Treatment Tool in Head and Neck Surgery | Part 2
Suction Drain As a Treatment Tool in Head & Neck Surgery – INTRODUCTION
This is an introduction to use of suction drains as a primary treatment for salivary fistulas, various air leaks after head and neck surgery, and infection. Suction drains may arguably reduce the need for free and pedicle flaps.
Length of hospital stay and the intensity of postoperative care can be dramatically reduced. Dr. Bastian includes the story of the “aha” moment that triggered this innovation.
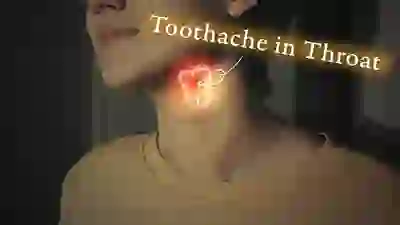
Hyoidynia | A Toothache in the Neck
A specific source of pain in the neck can worry and bother and elude diagnosis: *hyoidynia*. Dr. Bastian explains this little-known “toothache in the neck” disorder, and options for its treatment.

Nonorganic Breathing Noises
A nonorganic disorder in which a person’s vocal cords partially or fully close during breathing, which causes noisy breathing. Also called vocal fold dysfunction (VFD) or vocal cord dysfunction (VCD). The fundamental disorder is not in the mechanism itself, but rather in the patient’s “use” of the mechanism.

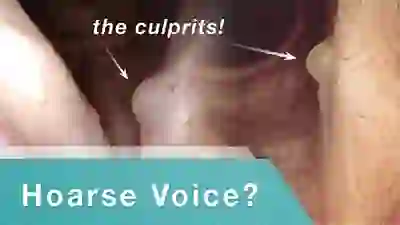
Laryngocele: A Cause of Hoarseness
A laryngocele is a disorder of the saccule, or laryngeal appendix, in which air abnormally expands it. Watch this video to see how a laryngocele behaves in real-time, and why that can affect the voice.
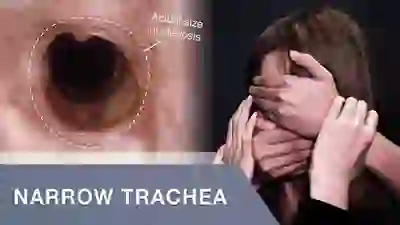
Tracheal Stenosis: Before and After Repair
In this video, trachea (windpipe) blockage causes shortness of breath until the narrowed segment is removed. You will see views of the trachea before and after surgical repair.

Wegener’s Granulomatosis – Forme Fruste (incomplete expression)
Wegener’s granulomatosis is a rare autoimmune disorder in which blood vessels become inflamed. The inflammation causes swelling and scarring. Three typical organs attacked are sinus/nasal cavities, lungs, and kidneys.
In the forme fruste variant, it is mostly an inflammatory stenosis (narrowing) of the area below the vocal cords, and also the trachea. A person becomes short of breath and begins to make harsh breathing sounds due to the narrowed passageway.
This is an example of one means of management: dilation of the narrowed area during a very brief general anesthetic in an outpatient operating room.
Post-Radiation Hypopharyngeal Stenosis
Individuals with larynx or pharynx (voice box or throat) cancer often undergo radiation therapy as part of their treatment regimen. An uncommon complication is stenosis (narrowing, scarring) of the entrance to the upper esophagus at the junction of the throat and esophagus. This video provides at example of this disorder.
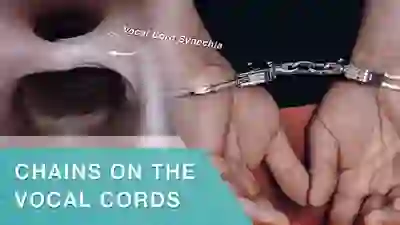
Vocal Cord Synechia
Vocal cord synechia is a condition wherein a scar band tethers the vocal cords to each other. Therefore, the vocal cords cannot fully open for breathing.

Having Trouble Swallowing Foods and Pills? A-CPD Can Be Treated with Cricopharyngeal Myotomy
A small percentage of (mostly) older people develop a progressive but treatable swallowing disorder called antegrade cricopharyngeal dysfunction (A-CPD).They have difficulty initially with solid foods and pills.
As the months and years pass, the tendency for food to lodge in the throat gradually increases. Eventually, they must limit their diets to softer and “easier” things more and more like “baby food.”
Special focus is placed on an effective endoscopic (through the mouth) laser procedure: cricopharyngeal myotomy.
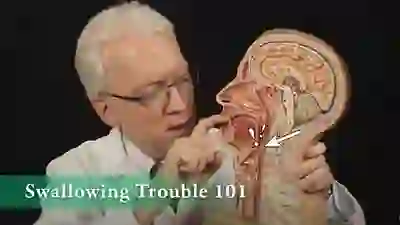
Swallowing Trouble 101
This video gives an overview of how swallowing works, how it can sometimes go wrong, and possible ways to treat those problems.
Cricopharyngeal Dysfunction: Before and After Cricopharyngeal Myotomy
This video shows x-rays of barium passing through the throat, first with a narrowed area caused by a non-relaxing upper esophageal sphincter (cricopharyngeus muscle), and then after laser division (myotomy) of this muscle.
Preoperatively, food and pills were getting stuck at the level of the mid-neck, and the person was eating mostly soft foods. After the myotomy, the patient could again swallow meat, pizza, pills, etc. without difficulty.
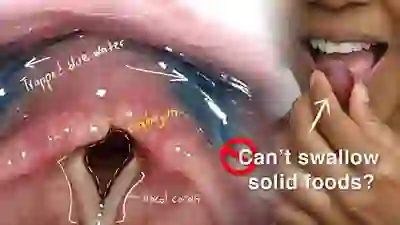
Cricopharyngeal Dysfunction: Difficulty Swallowing, Especially Solid Foods
In this video, Dr. Robert Bastian of Bastian Voice Institute explains this progressive swallowing problem, and presents options for treatment.
Cricopharyngeal dysfunction is caused by failure of relaxation of the upper esophageal sphincter—cricopharyngeus muscle—during eating. Typically it is solid foods that tend to lodge in the mid-neck area where this muscle is located. The disorder is described in detail within this short instructional videotape.
Cricopharyngeal Spasm: A Troubling Feeling of a Lump in the Throat
In this video, Dr. Robert Bastian of Bastian Voice Institute explains cricopharyngeal spasm, a problem that causes a troubling sensation of throat constriction or of a foreign body in the throat.
Cricopharyngeal spasm is caused by over-contraction of the upper esophageal sphincter, or cricopharyngeus muscle, and causes an annoying, preoccupying, even anxiety-provoking sensation of something stuck in the throat, like a “wad of phlegm.” A common description is “There is something in my throat that I can’t swallow or spit out.”
Individuals with this problem often have difficulty getting a clear diagnosis, and may see several physicians and undergo unnecessary and unhelpful tests in their quest for an answer. Sometimes also called “globus sensation,” this disorder is described and explained in detail.