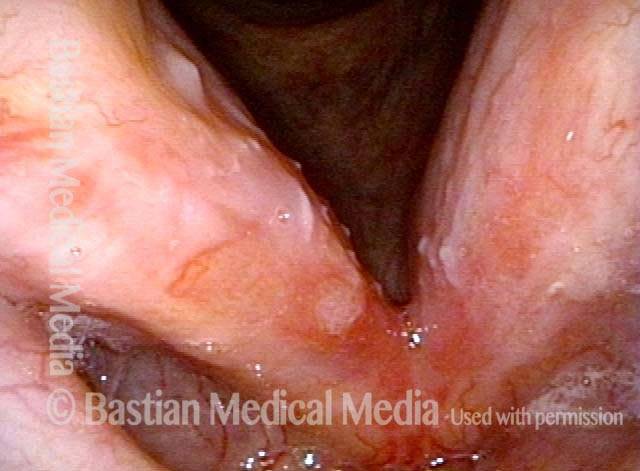
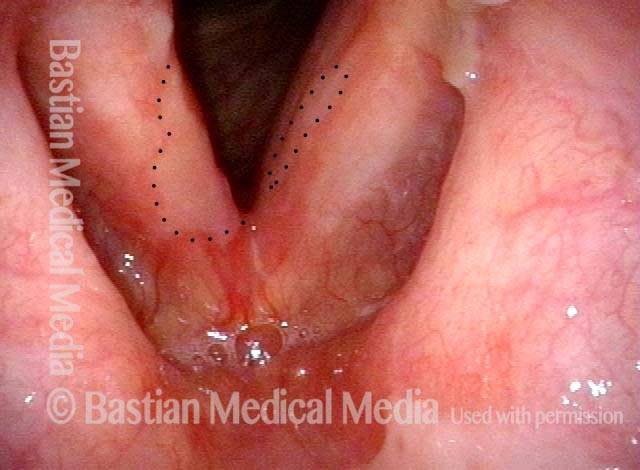
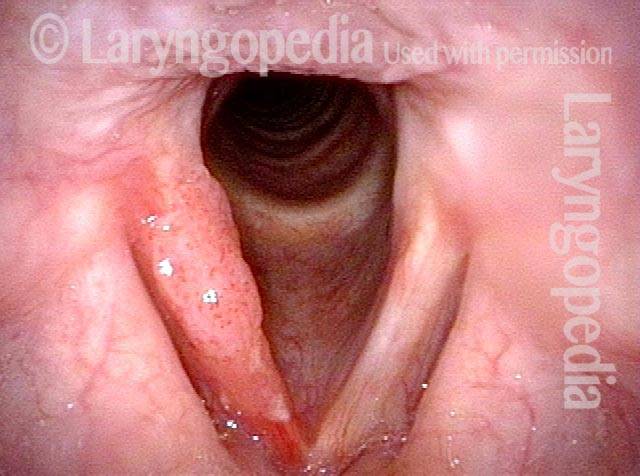
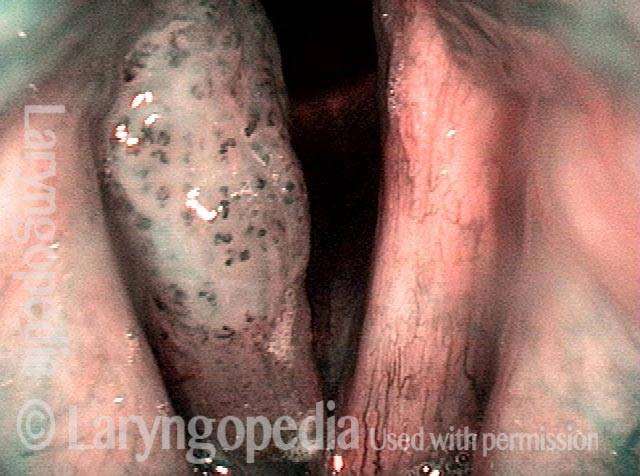
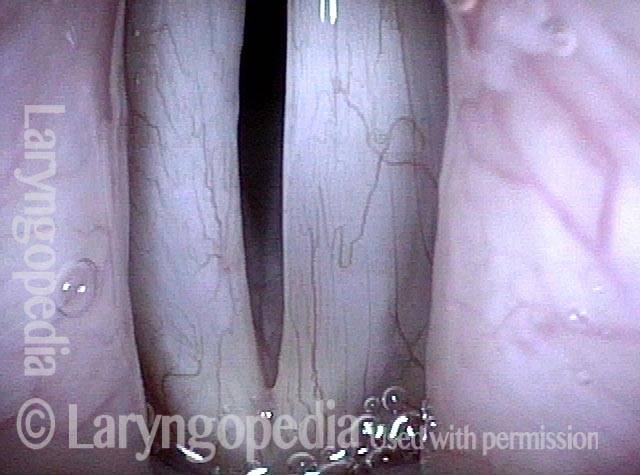
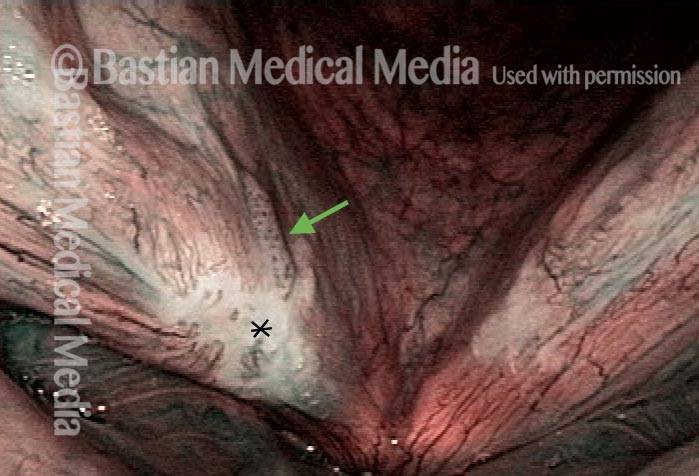
Carcinoma in situ (CIS) is a lesion comprised of “cancer cells,” but with those cells limited to the lining mucosa and without evidence of extension to adjacent structures. In other words, there is no sign of invasion beyond the mucosa. CIS is typically a localized and highly curable precursor to invasive cancer. It is sometimes called intraepithelial carcinoma.
In laryngology, CIS is found primarily on the vocal cords themselves, where a tiny, early lesion can change the quality of the voice. In other locations, CIS would ordinarily be “silent.”
Is CIS considered cancer or pre cancerous?
Since the definition of malignancy is cells growing outside of their normal location, or that have metastasized, then CIS is technically not malignant. The cells are cancerous but still within the mucosa (covering layer) of the vocal cords. However, CIS should be regarded and treated as early cancer since if it is left alone it will eventually penetrate beyond the mucosa. So it is terrific when it is taken care of extremely early and cure rate extraordinarily high, but of course careful follow up examinations are necessary.