Clinical Diagnosis of R-CPD via Syndrome-Matching: A Case Against Unnecessary Testing
ABSTRACT
This article presents a strong case for clinical diagnosis of retrograde cricopharyngeus dysfunction (R-CPD) based on syndrome-matching. When symptoms align precisely with the well-established R-CPD profile, this approach allows clinicians to avoid unnecessary, uncomfortable, and costly diagnostic procedures—relying instead on high-confidence, pattern-based recognition to lead directly to treatment.
Introduction
In 2019, Bastian and Smithson first fully described the syndrome of retrograde cricopharyngeus dysfunction (R-CPD) [Bastian & Smithson, 2019 [1]: At that time, a literature search revealed only three prior single-case reports describing inability to burp, typically accompanied by one or two associated symptoms.[2,3,4] Prior to the 2019 publication, however, no comprehensive symptom constellation had been codified, and no patient had been successfully treated. The initial series of 51 patients established a definitive syndrome profile and treatment pathway.
Since then, the codified symptom complex of R-CPD has been documented not only in the original article but also in numerous subsequent publications, articles, and educational videos—many of which are accessible at the public service and teaching website, laryngopedia.com/rcpd
Cardinal Symptoms of R-CPD
Patients with R-CPD typically swallow normally, but exhibit a strikingly consistent set of symptoms. At least three of the following four primary features are present:
- Inability to burp, except for rare, spontaneous, non-relieving, and non-harnessable micro-burps.
- Gurgling noises, often postprandial, which can range from quiet and internal to audible across a room.
- Bloating, defined here as pressure sensations in the abdomen, chest, and lower neck, frequently accompanied by visible distention later in the day.
- Excessive flatulence, ranging from mildly increased to, much more often, “world-class.”
Common but Less Universal Symptoms
- Painful hiccups
- Nausea or early satiety after eating
- Acid reflux (heartburn)
- Hypersalivation when otherwise symptomatic
- Sensation of shortness of breath (i.e., inability to fully expand the lungs)
- Difficulty vomiting (requiring aggressive and prolonged retching)
- Constipation
- Autonomic symptoms such as flushing and tachycardia
Sufficiency of Clinical Diagnosis
Given this richly distinctive symptom constellation, Bastian has long argued—both in peer conversations and physician tutorials—that syndrome-matching is not only necessary but also sufficient for confident clinical diagnosis. When symptoms align with the R-CPD profile, no further testing is required before botulinum toxin injection, which both validates and treats the condition.
Note as well that initial office examination can easily include at no additional cost, brief esophagoscopy, revealing the “always open” appearance. Furthermore, during E.R. visits for intense abdominal discomfort, many patients have been told that a KUB, CXR, CT, etc. shows extraordinary abdominal air.
Lifelong Pattern as Diagnostic Anchor
Among the more telling features is that the inability to burp has been lifelong—from the patient’s own memory. While some mothers report burping in infancy, affected individuals typically cannot recall ever being able to burp adequately [Bastian & Smithson, 2019]. The full-blown syndrome may have initiated in adolescence or even early adulthood, but the lifelong pattern of inability to burp effectively rules out any ominous cause.
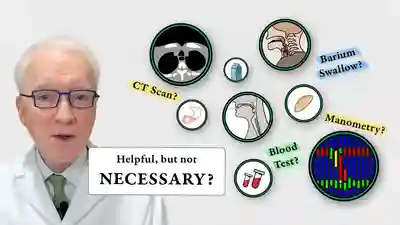
Evidence Against Testing-First Approach
Among more than 1,100 patients evaluated and treated to date, thousands of diagnostic tests were obtained prior to referral—yet yielded no primary diagnosis of R-CPD [Bastian, unpublished data; institutional records, 2015–2025]. Diagnoses rendered before self-referral included acid reflux, irritable bowel syndrome, gastroparesis, chronic constipation, and aerophagia. However, after identification and treatment of R-CPD, these GI symptoms were ultimately shown to be secondary consequences of R-CPD rather than primary disorders.
This massive experience has led to the formulation of “Bastian’s Dictum”:
“If the syndrome of R-CPD is matched, then all GI symptoms should be assumed to result from R-CPD—until proven otherwise after ability to burp is restored.”
Manometric proof of the entity can also be adduced as evidence against the testing-first approach. Two very strong studies have now validated the R-CPD not only observationally/syndromically but also manometrically. [5,6]. People with syndromic R-CPD (“I can’t burp and…”) have been shown to have R-CPD (“The UES won’t relax retrograde. This person can’t burp.”)
Why Is Testing Still Common in Other Clinics? Some Speculations:
- Medical Training Bias to Value Measurement Over Observation: Physicians are taught to prioritize data collection and objective proof. Observational diagnosis — even when robust — can feel insufficient without measurable parameters.
- Systemic and Financial Pressures: Some healthcare systems require confirmatory testing (e.g., manometry) before authorizing treatment. There may also be financial incentives tied to diagnostics.
- Conative Style of Physicians (“High Fact Finders” as described by Kolbe): Beyond their training (#1 above), doctors may be innately inclined toward data-heavy decision-making and resist relying on pattern recognition alone. High fact finders instinctively ask, “tell me more.” Low fact finders can also deal with a lot of detail, but they instinctively shed what they see as irrelevant, looking for the kernel or bottom line.
- Patient Psychology and Deference: Even well-informed patients may defer to their doctor’s preferences or feel more secure pursuing all options “just in case.”
Proposed Best Practice: Direct-to-Treatment
When patients match the R-CPD profile, proceeding directly to botulinum toxin injection—whether via EMG-guided office procedure or under general anesthesia—is an appropriate, patient-centric, ethical, and cost-effective first step. This serves both to validate the diagnosis and to initiate treatment.
For More Hesitant Physicians or Systems: Practical and Ethical Considerations
When diagnostic testing is pursued, contrary to the above thought process—whether for institutional authorization, provider reassurance, or patient preference—clinicians must consider whether to disclose that many experts view such testing as unnecessary in the presence of a classic R-CPD symptom profile. In an age of increasingly informed patients, it is common for individuals to ask, “May I skip the tests and proceed directly to botulinum toxin injection?” On what grounds would such a request be declined, particularly when the patient clearly matches the established syndrome?
The only test that can confirm R-CPD through objective measurement is specially tailored high-resolution manometry with ingested carbonation. But if such a test fails to detect the dysfunction in a patient whose symptoms are a textbook match, is it ethical to withhold treatment? In such cases, what should carry more diagnostic weight—the test result or the clinical pattern?
Cost also raises important ethical considerations. In the author’s setting, the all-inclusive cost of proceeding directly to treatment for international or self-pay patients is approximately $4,000. This figure is often much higher at other institutions. High-resolution manometry—if paid out of pocket—can add as much as $1,500, though Medicare reimbursement is considerably lower. Should more extensive diagnostic workups be pursued (“shotgun testing”), the total added cost may exceed $7,000 to $10,000 when including anesthesia, facility fees, endoscopy, and other procedural overhead [Based on Medicare fee schedules and typical facility billing data, 2024–2025].
This raises a final ethical question:
When the diagnosis is evident on syndromic grounds, is it justifiable to impose additional financial burden on the patient or the healthcare system?
Final Thoughts
This analysis encourages physicians to consider using syndrome recognition of R-CPD in clinical decision-making. When a symptom constellation is well-characterized, consistently present, and reliably responsive to a known treatment, the case for avoiding unnecessary testing becomes compelling. In R-CPD, pattern-based diagnosis not only shortens the path to relief but also models a more patient-centered, arguably ethical, and efficient standard of care.
References
- Bastian, RW and Smithson, ML: Inability to belch and associated symptoms due to retrograde cricopharyngeus dysfunction: Diagnosis and treatment. Oto Open 2018 https://doi.org/10.1177/2473974X19834553
- Kahrilas PJ, Dodds WJ, Hogan WJ. Dysfunction of the belch reflex: a cause of incapacitating chest pain. Gastroenterology. 1987; 93: 818–822. https://doi.org/10.1016/0016-5085(87)90445-8
- Waterman DC, Castell DO. Chest pain and inability to belch. Gastroenterology. 1989; 96: 274–275. https://doi.org/10.1016/0016-5085(89)90822-6
- Tomizawa M, Motoyasu K, Takashi A, et al. A case of inability to belch. J Gastroenterol Hepatol. 2001; 16: 349–351. https://doi.org/10.1046/j.1440-1746.2001.02333.x
- Renske A.B. Oude Nijhuis, Jurjaan A. Snelleman, Jac M. Oors, Boudewijn F. Kessing, Derrek A. Heuveling, Jeroen M. Schuitenmaker, Liesbeth ten Cate, Andreas J.P.M. Smout, Albert J. Bredenoord, The inability to belch syndrome: A study using concurrent high‐resolution manometry and impedance monitoring, Neurogastroenterology & Motility, 10.1111/nmo.14250, 34, 5, (2021). https://doi.org/10.1111/nmo.14250
- Raymenants, Karlien et al. Diagnosis of Retrograde Cricopharyngeus Dysfunction Using High Resolution Impedance Manometry and Comparison With Control Subjects. Clinical Gastroenterology and Hepatology, 2025. https://doi.org/10.1016/j.cgh.2024.12.014
Share this article
RCPD Workup – Do You Need Testing for a Diagnosis?
What is necessary to diagnose R-CPD? What is sufficient? Do we need to spend thousands of dollars for x-rays, manometry, upper GI scopes, gastric emptying studies?