Miotomia Cricofaringea
La miotomia cricofaringea (CPM) è una procedura in cui il muscolo cricofaringeo, che forma un “anello” attorno all’esofago superiore, viene diviso o tagliato per rilassarlo. Questo viene fatto nei casi in cui questo muscolo cricofaringeo (cioè lo sfintere esofageo superiore) non riesce a rilassarsi quando si deglutisce (disfunzione cricofaringea anterograda [A-CPD]), con conseguente ostruzione funzionale. Il CPM lascia il muscolo sempre aperto e consente alla persona di riprendere la deglutizione in modo relativamente normale.
In una percentuale di soggetti con mancato rilassamento del muscolo cricofaringeo, le continue alte pressioni della deglutizione possono eventualmente causare una “ernia” nel passaggio della deglutizione chiamata diverticolo di Zenker.
Procedura CPM
La miotomia cricofaringea viene eseguita in anestesia generale, in due modi: la metodologia preferita e più recente viene eseguita per via endoscopica. Utilizzando questo metodo, un “tubo” cavo e illuminato, chiamato esofagoscopio, viene inserito nella gola e nella parte superiore dell’esofago per esaminare l’area e pianificare il passaggio successivo. Quindi, uno speciale cannocchiale laser viene posizionato nell’esofago superiore. Un microscopio consente una visione ingrandita e ben illuminata dell’anello muscolare incriminato.
If a clear view cannot be achieved during esophagoscopy due to difficult patient anatomy (e.g., jaws won’t open well, small lower jaw, short neck, large upper teeth), then we return to a more traditional approach through an incision on the lower left neck. In this case, the muscle is divided from outside in. Depending on a number of issues, an associated Zenker’s diverticulum may or may not be removed at the same time.
Il laser viene utilizzato per dividere il muscolo e spezzarne la “presa”. Se la sacca di Zenker è evidente, è “marsupializzata”, il che significa che la sua apertura è allargata per essere sicuri che la sacca non trattenga il cibo, ma svuoti invece il suo contenuto direttamente nell’esofago.
A seconda del paziente e dei problemi chirurgici, un drenaggio di aspirazione può essere posizionato all’interno dell’esofago superiore e fatto uscire attraverso il naso. Un secondo tubicino per l’alimentazione può essere inserito attraverso il naso e giù nello stomaco. Una volta posizionate, entrambe le tube vengono rimosse la mattina successiva all’intervento.
Se durante l’esofagoscopia non è possibile ottenere una visione chiara a causa delle difficoltà anatomiche del paziente (ad esempio, le mascelle non si aprono bene, la mascella inferiore è piccola, il collo corto, i denti superiori grandi), si ritorna a un approccio più tradizionale attraverso un’incisione sulla parte inferiore collo sinistro. In questo caso, il muscolo viene diviso dall’esterno verso l’interno. A seconda di una serie di problemi, un diverticolo di Zenker associato può o meno essere rimosso contemporaneamente.
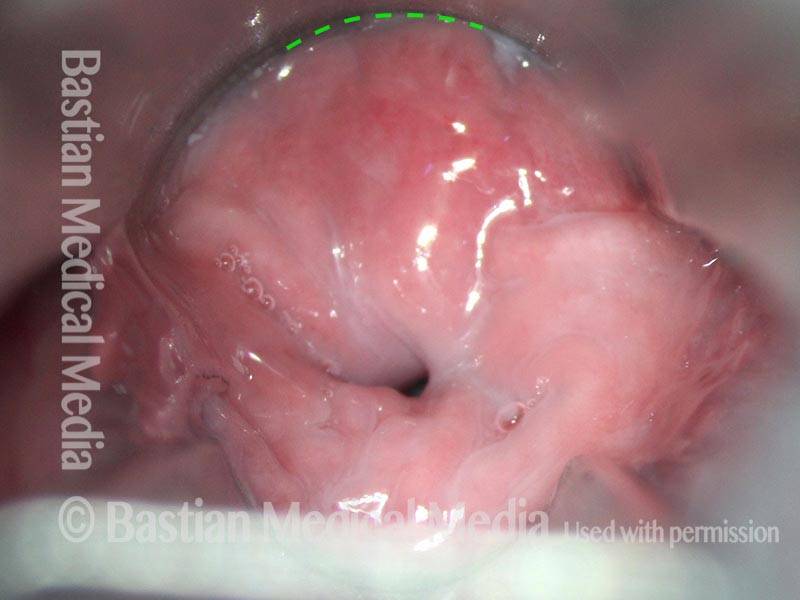
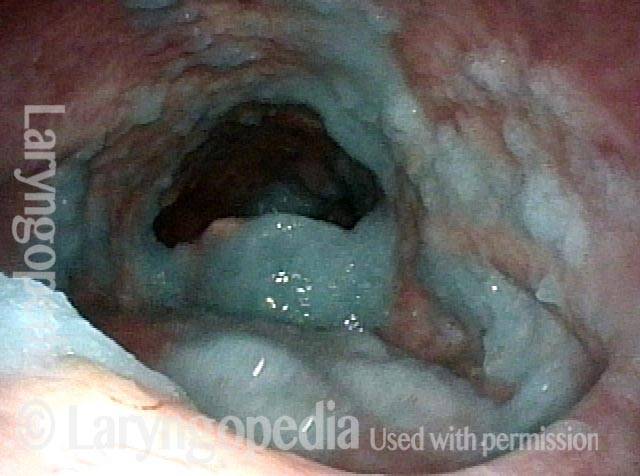
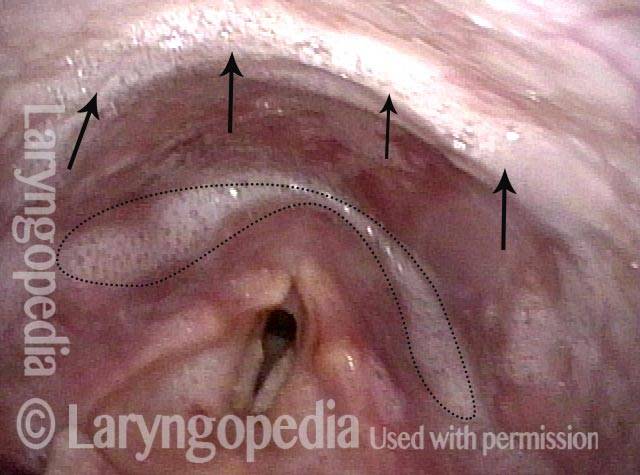
Cricopharyngeal myotomy (1 of 7)
Cricopharyngeal myotomy (1 of 7)
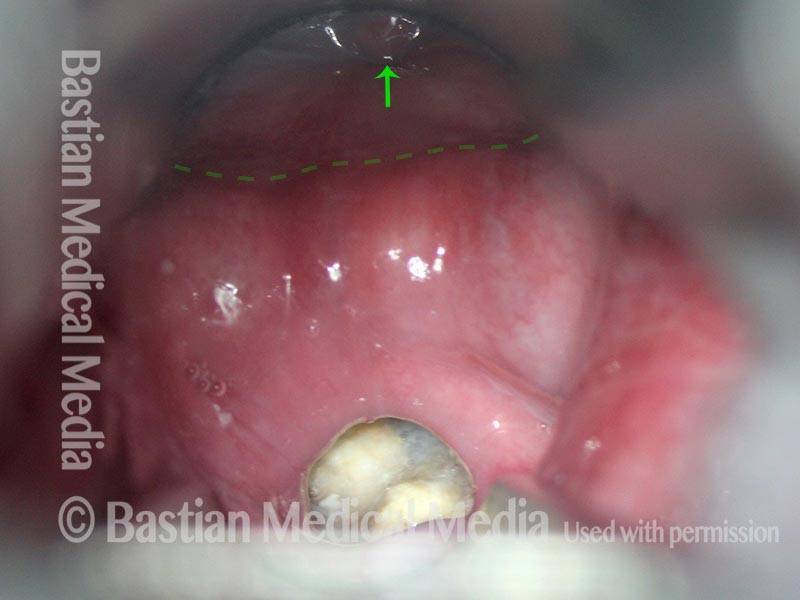
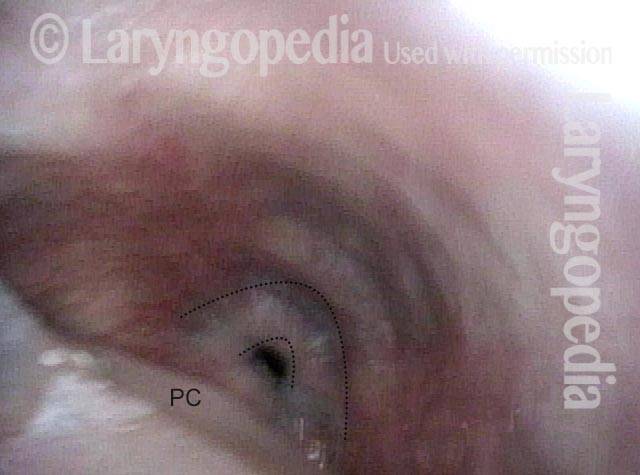
Cricopharyngeal myotomy (2 of 7)
Cricopharyngeal myotomy (2 of 7)
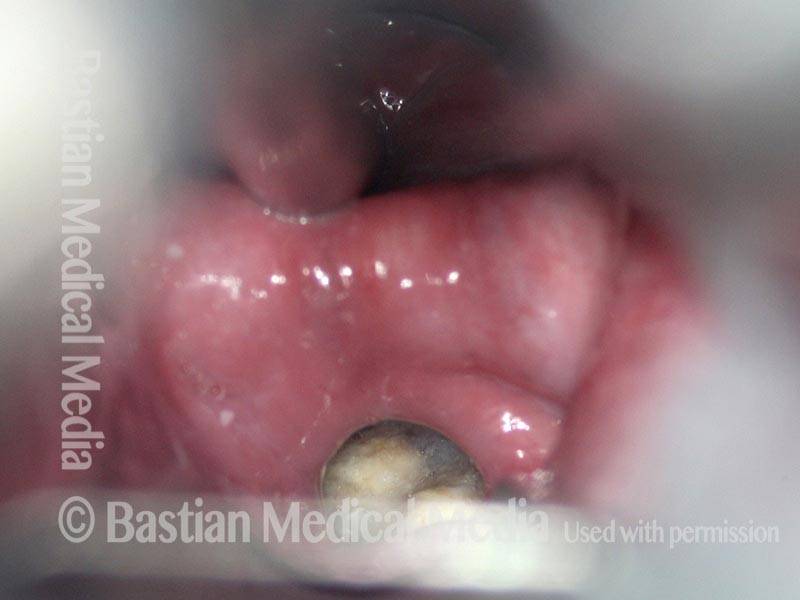
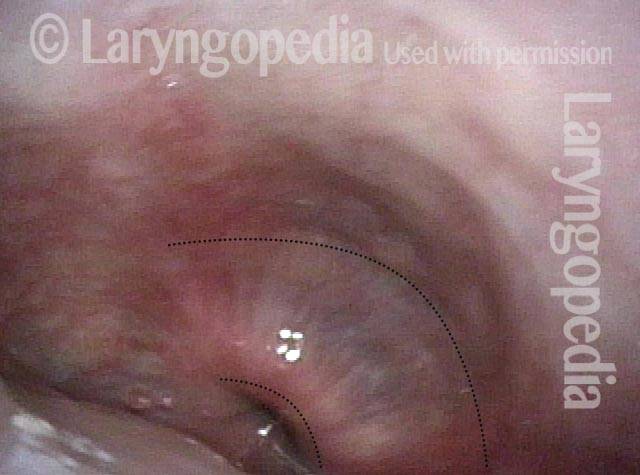
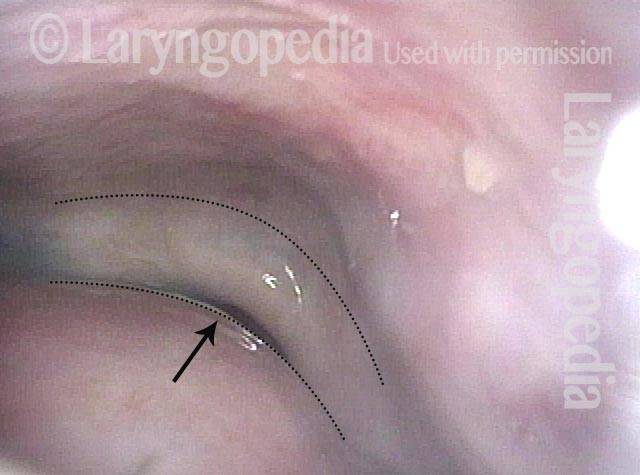
Cricopharyngeal myotomy (3 of 7)
Cricopharyngeal myotomy (3 of 7)
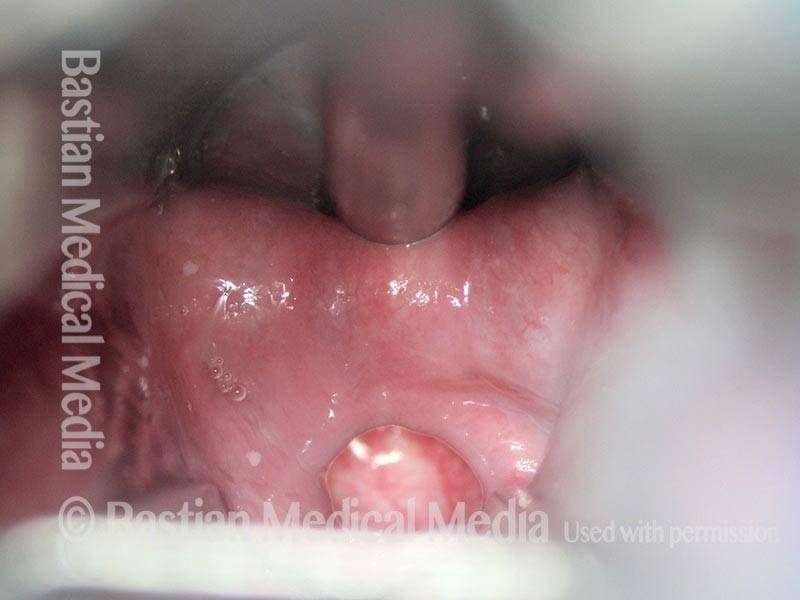
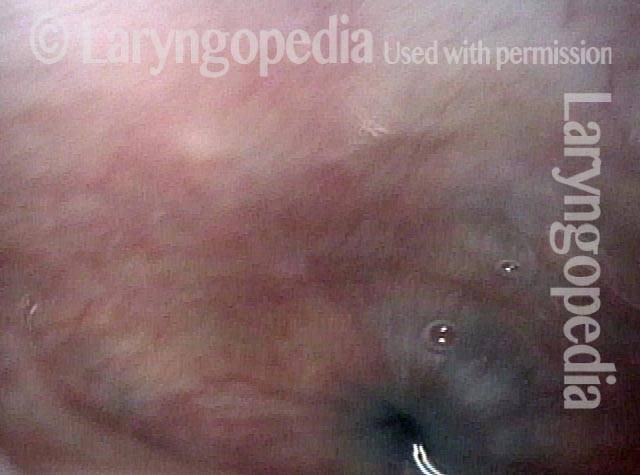
Cricopharyngeal myotomy (4 of 7)
Cricopharyngeal myotomy (4 of 7)
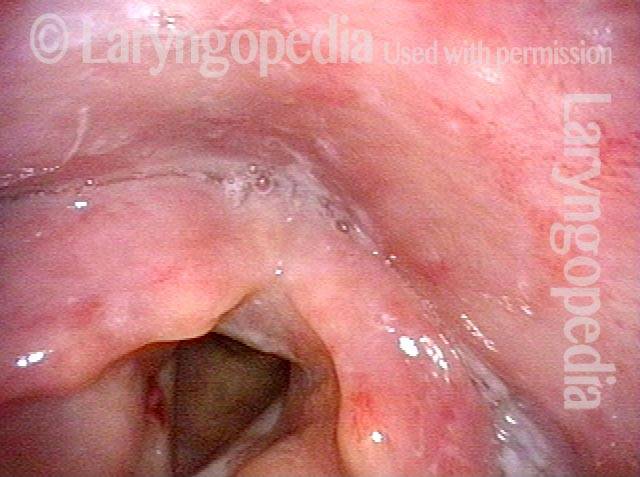
Cricopharyngeal myotomy (5 of 7)
Cricopharyngeal myotomy (5 of 7)
Cricopharyngeal myotomy (6 of 7)
Cricopharyngeal myotomy (6 of 7)
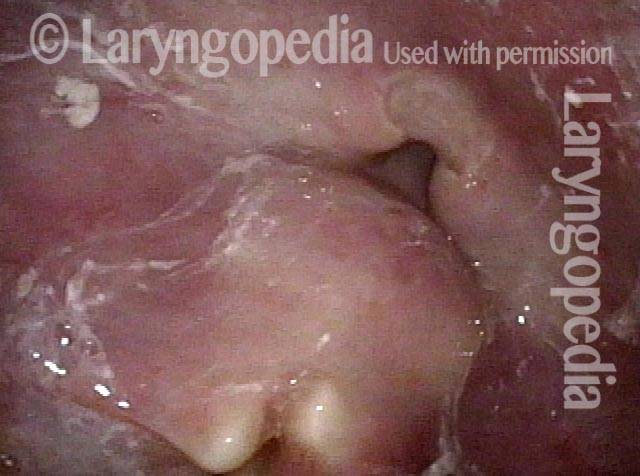
Cricopharyngeal myotomy (7 of 7)
Cricopharyngeal myotomy (7 of 7)
Tasso di successo del CPM
Il tasso di successo può variare a seconda del grado in cui la persona è un candidato ideale per questo intervento chirurgico. Quando la disfagia da cibo solido è il sintomo principale e quando gli studi a raggi X mostrano il mancato rilassamento del muscolo, la procedura può ripristinare drasticamente la capacità di deglutire dell’individuo.
La soddisfazione dei pazienti per i risultati è solitamente molto elevata. “Posso mangiare di nuovo tutto ciò che voglio”, si sente spesso dopo l’intervento chirurgico. Di tanto in tanto un individuo ha più di un deficit di deglutizione, di cui il CPMD è solo uno. In questo caso, la deglutizione potrebbe essere migliore, ma non ancora perfetta dopo il CPM.
Rischi del CPM
A meno che tu non abbia problemi di salute significativi, i rischi sommati insieme sono molto piccoli. I rischi possono includere:
- Una reazione al farmaco, un problema cardiaco, ecc., durante l’anestesia generale.
- Trauma dentale: ad esempio, dente scheggiato, graffiato, rotto o spostato.
- Se l’intervento viene eseguito all’interno dell’esofago esiste un piccolo rischio di un’infezione speciale, potenzialmente grave, chiamata mediastinite. (Non abbiamo riscontrato questo problema con un totale BVI di circa 120 interventi CPM).
- Se l’intervento viene eseguito attraverso un’incisione sul collo, esiste un piccolo rischio aggiuntivo di paralisi temporanea – o raramente permanente – di una corda vocale, che viene gestita in modo relativamente semplice.
- Il “rischio” o il risultato finale è che il medico non può garantire il grado preciso di miglioramento, ovvero se il risultato sarà “buono”, “molto buono” o “spettacolare”. Ciò dipende in larga misura dalle componenti precise del problema originale; poiché il medico tende a conoscerli prima dell’intervento chirurgico, di solito può fare una stima ragionevolmente affidabile del miglioramento atteso.
Cosa aspettarsi dopo il CPM
Dopo l’intervento, i pazienti tornano a casa più tardi il giorno dell’intervento o la mattina dopo, con rare eccezioni. Naturalmente, la guida deve essere affidata ad un familiare o ad un amico. La maggior parte delle persone ha effetti collaterali minimi dell’anestesia. La nausea, ad esempio, è diventata relativamente rara.
Gli antidolorifici sono costituiti da Tylenol o Tylenol con codeina, salvo allergie o sensibilità. L’acqua può essere ingerita immediatamente dopo l’intervento chirurgico.
I primi cinque giorni la dieta dovrebbe consistere di liquidi e cibi molto morbidi. L’acqua è sempre l’ultima cosa ingerita dopo ogni “pasto”, per “risciacquare” l’area dell’intervento. Alcuni ritengono che cibi/liquidi salati o acidi brucino l’area dell’intervento.
Occasionalmente i denti sembrano un po’ doloranti e allentati, soprattutto gli incisivi centrali superiori.
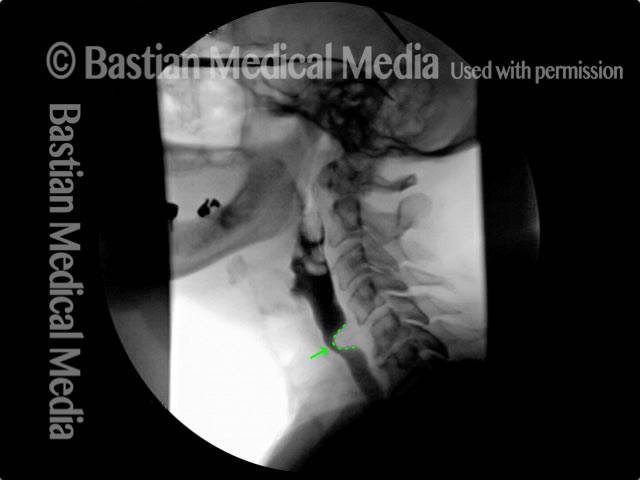
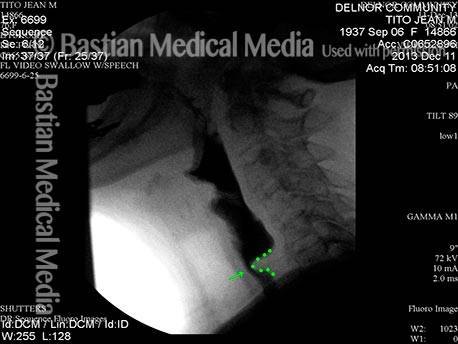
Disfunzione cricofaringea, prima e dopo la miotomia
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (2 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (2 of 2)
Esempio 2
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (1 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (1 of 2)
Esempio 3
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: after myotomy (2 of 2)
Cricopharyngeal dysfunction: after myotomy (2 of 2)
Miotomia cricofaringea per l’alimentazione ricreativa e la gestione della saliva
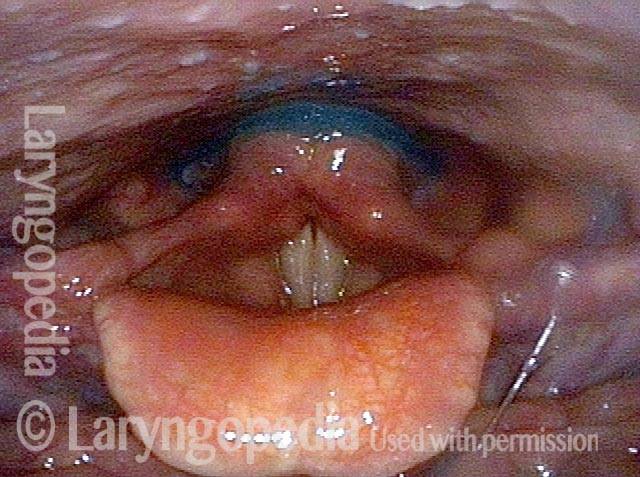
Panormaic view, post CPM (1 of 4)
Panormaic view, post CPM (1 of 4)
Trumpet maneuver (2 of 4)
Trumpet maneuver (2 of 4)
Closer view (3 of 4)
Closer view (3 of 4)
Well-managed saliva (4 of 4)
Well-managed saliva (4 of 4)
98 anni, prima e dopo la miotomia
Immediately after swallowing (1 of 10)
Immediately after swallowing (1 of 10)
Zenker’s (2 of 10)
Zenker’s (2 of 10)
Dysphagia (3 of 10)
Dysphagia (3 of 10)
Residue from Zenker’s (4 of 10)
Residue from Zenker’s (4 of 10)
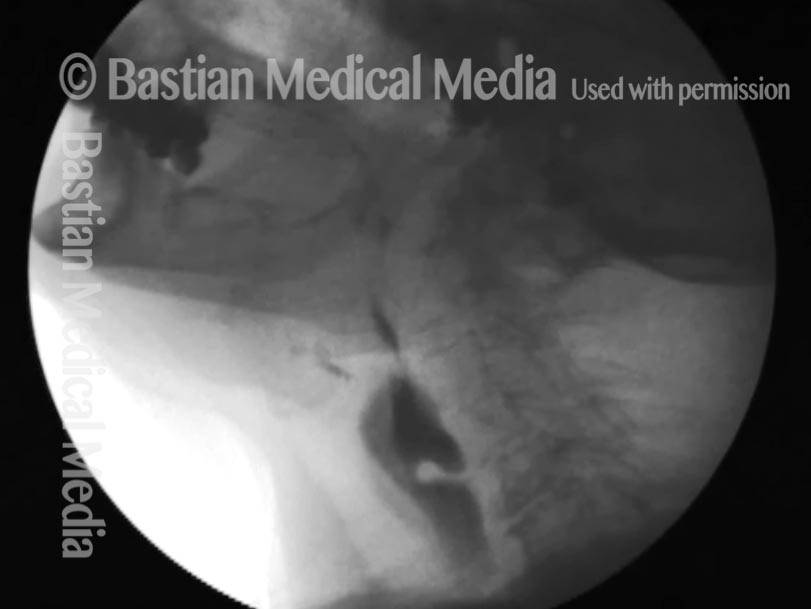
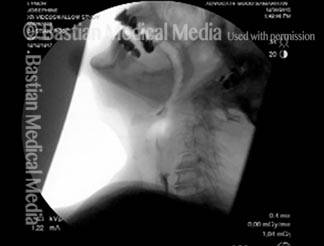
X-ray showing Zenker’s (5 of 10)
X-ray showing Zenker’s (5 of 10)
Moments later (6 of 10)
Moments later (6 of 10)
After myotomy (7 of 10)
After myotomy (7 of 10)
No residue (8 of 10)
No residue (8 of 10)
Zenker’s gone (9 of 10)
Zenker’s gone (9 of 10)
No barium in hypopharynx (10 of 10)
No barium in hypopharynx (10 of 10)
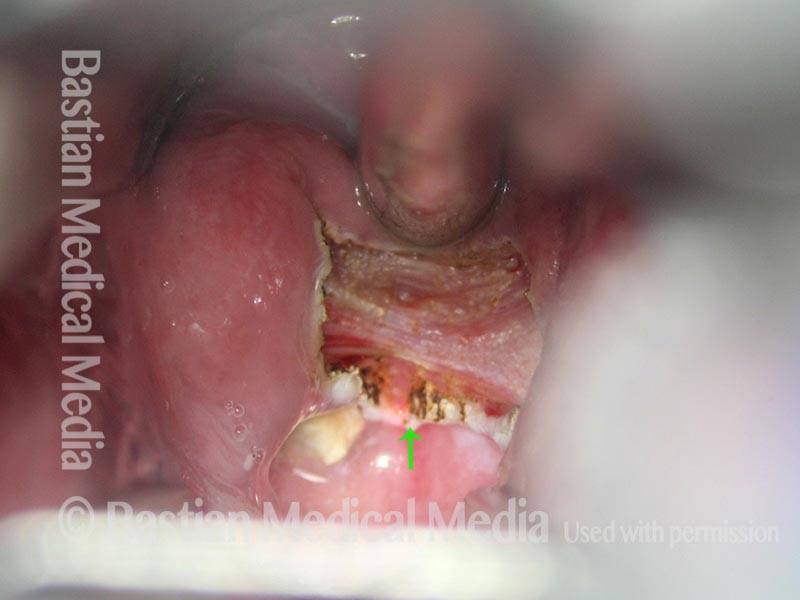
Ottima vista della ferita chirurgica della miotomia cricofaringea fresca
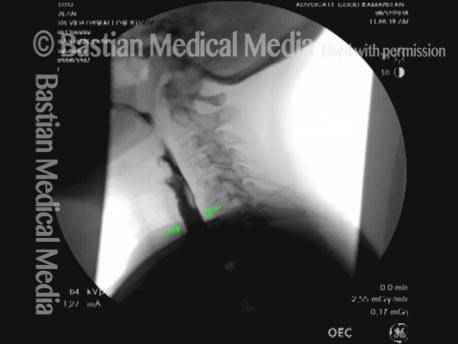
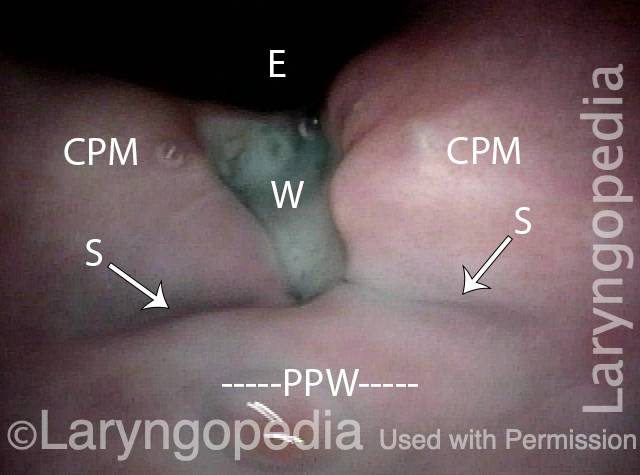
CPM dysfunction (1 of 4)
CPM dysfunction (1 of 4)
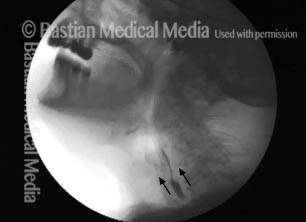
VFSS six years later (2 of 4)
VFSS six years later (2 of 4)
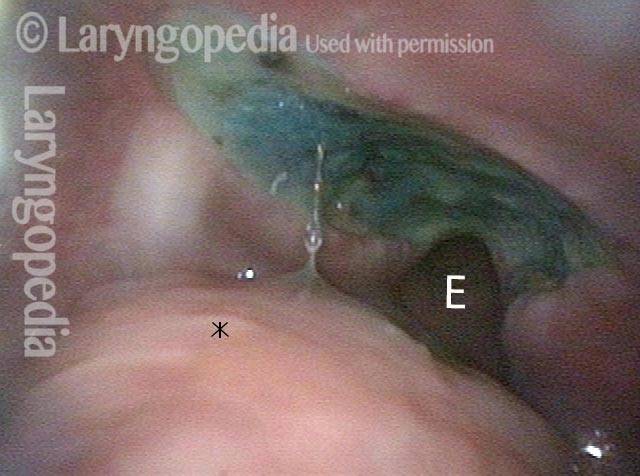
Five days post-op (3 of 4)
Five days post-op (3 of 4)
Cervical esopagus (4 of 4)
Cervical esopagus (4 of 4)
Bolus Stream prima e dopo la miotomia cricofaringea
Pre-myotomy (1 of 2)
Pre-myotomy (1 of 2)
Post-myotomy (2 of 2)
Post-myotomy (2 of 2)
Risultati VESS dopo la radioterapia
Narrowed pharyngeal wall (1 of 7)
Narrowed pharyngeal wall (1 of 7)
Swallowing applesauce (2 of 7)
Swallowing applesauce (2 of 7)
After sipping water (3 of 7)
After sipping water (3 of 7)
Gravity aiding in swallowing (4 of 7)
Gravity aiding in swallowing (4 of 7)
Lifting larynx (5 of 7)
Lifting larynx (5 of 7)
A closer look (6 of 7)
A closer look (6 of 7)
Gravity aiding again in swallowing (7 of 7)
Gravity aiding again in swallowing (7 of 7)
L’evoluzione di una ferita da miotomia cricofaringea
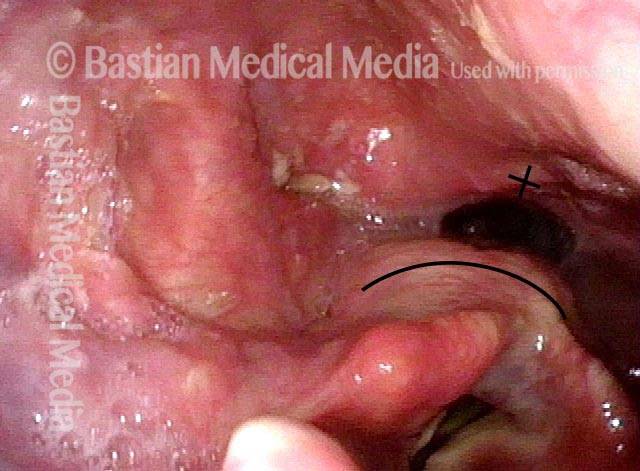
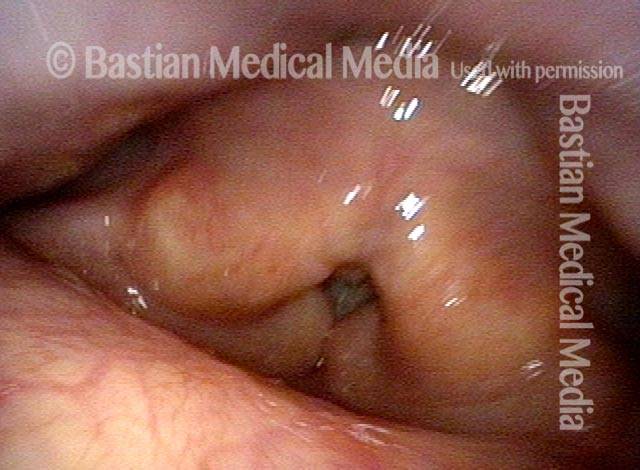
Difficulty swallowing solid foods (1 of 8)
Difficulty swallowing solid foods (1 of 8)
Pooled saliva (2 of 8)
Pooled saliva (2 of 8)
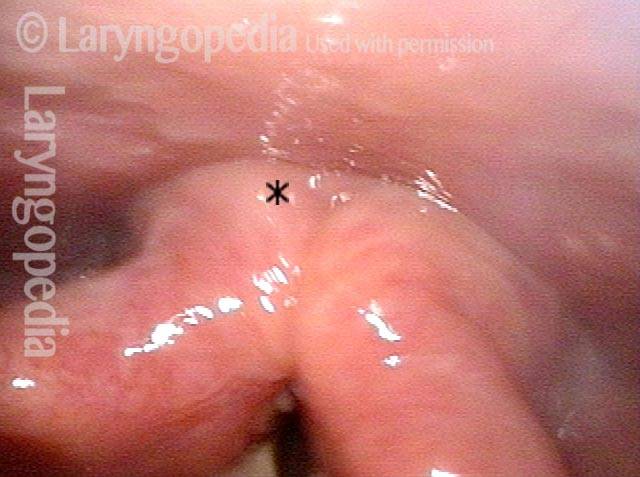
Muscle bulge (3 of 8)
Muscle bulge (3 of 8)
Residue in swallow crescent (4 of 8)
Residue in swallow crescent (4 of 8)
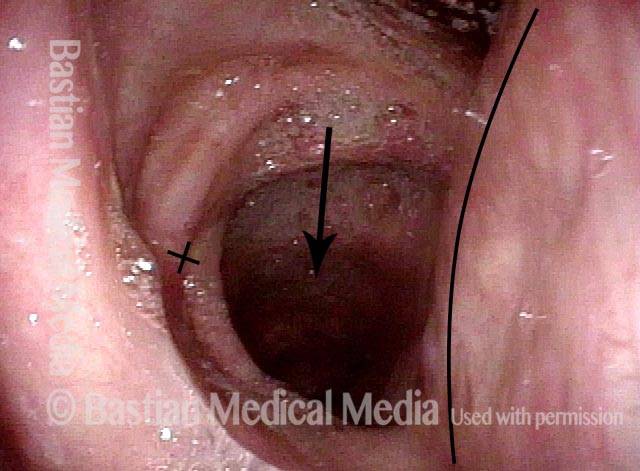
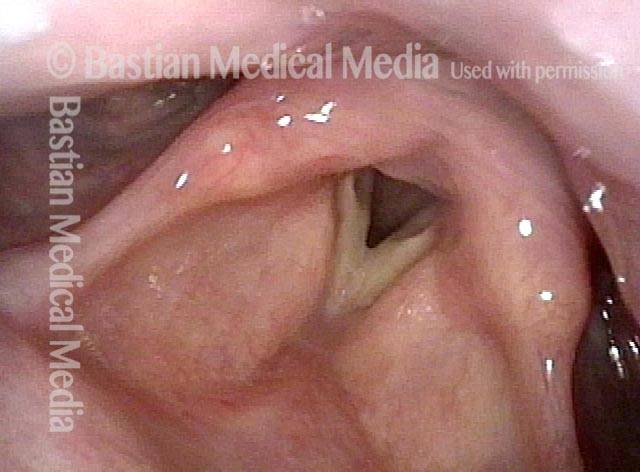
Three weeks later (5 of 8)
Three weeks later (5 of 8)
Residual “wound” (6 of 8)
Residual “wound” (6 of 8)
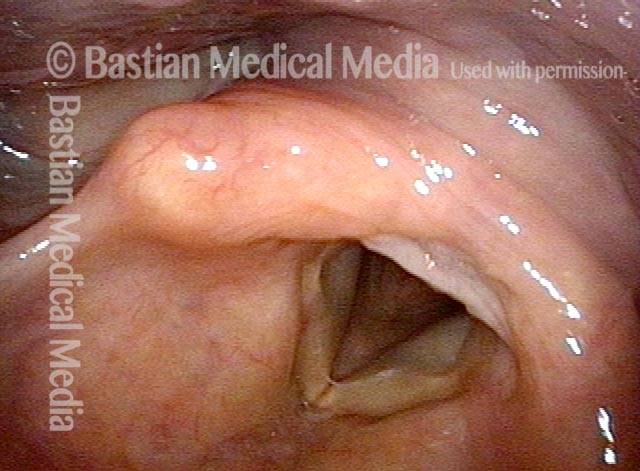
Three months post-op (7 of 8)
Three months post-op (7 of 8)
At close range (8 of 8)
At close range (8 of 8)
Diverticolo di Zenker una settimana dopo la miotomia del cricofaringeo
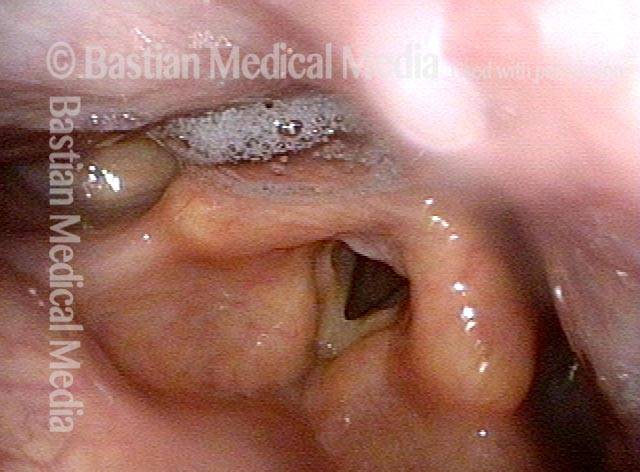
Zenker’s Sac (1 of 3)
Zenker’s Sac (1 of 3)
Zenker’s Sac (2 of 3)
Zenker’s Sac (2 of 3)
Zenker’s Sac (3 of 3)
Zenker’s Sac (3 of 3)
Condividi questo articolo

A-CPD può essere trattato con la miotomia cricofaringea
Una piccola percentuale di (soprattutto) persone anziane sviluppa un disturbo della deglutizione progressivo ma curabile chiamato disfunzione cricofaringea anterograda (A-CPD). Inizialmente hanno difficoltà con cibi solidi e pillole.
Con il passare dei mesi e degli anni, la tendenza del cibo a depositarsi in gola aumenta gradualmente. Alla fine, devono limitare la loro dieta a cibi più morbidi e “facili”, sempre più simili agli “alimenti per bambini”. Particolare attenzione è posta su un’efficace procedura laser endoscopica (attraverso la bocca): la miotomia cricofaringea.
Disfunzione cricofaringea: prima e dopo il CPM
This video shows x-rays of barium passing through the throat, first with a narrowed area caused by a non-relaxing upper esophageal sphincter (cricopharyngeus muscle), and then after laser division (myotomy) of this muscle.
Preoperatively, food and pills were getting stuck at the level of the mid-neck, and the person was eating mostly soft foods. After the myotomy, the patient could again swallow meat, pizza, pills, etc. without difficulty.
Difficoltà di deglutizione 101
Questo video offre una panoramica di come funziona la deglutizione, di come a volte può andare storto (presbifagia o A-CPD) e dei possibili modi per trattare questi problemi (terapia della deglutizione o miotomia cricofaringea).
Cosa succede se i miei denti si allentano dopo il CPM?
Evita di muoverli o di mordere cibi duri finché non si irrigidiscono da soli. Molto spesso ciò richiede circa una settimana.
Quando dovrei consultare il mio medico dopo la procedura?
Circa sei settimane dopo l’intervento è previsto uno studio video-fluoroscopico della deglutizione (VFSS) da confrontare con quello effettuato prima dell’intervento.
Porti con te una copia di quello studio alla visita postoperatoria con il tuo chirurgo più tardi lo stesso giorno in cui è stata eseguita la VFSS.
Quali sintomi postoperatori richiederebbero attenzione immediata?
Tutti i seguenti sono molto improbabili, ma lo sono:
- Incapacità di deglutire liquidi.
- Dolore al torace o alla schiena che aumenta di gravità dal momento dell’intervento chirurgico.
- Febbre o brividi.
- Qualsiasi altra cosa che ti preoccupa!
Come faccio a sapere in anticipo in che modo verrà eseguito l'intervento?
I candidati al CPM dovrebbero accettare entrambi i metodi. In questo modo, il chirurgo può tentare il metodo preferito dall’interno dell’esofago. Se questo metodo non è possibile, passeranno al CPM attraverso un’incisione sul collo.
La maggior parte delle persone, quando escono dalla sala operatoria, vogliono sapere se il problema è stato risolto, “in un modo o nell’altro”.
Se la disfagia si verifica anni dopo l’intervento chirurgico, è possibile eseguire nuovamente il CPM?
Le 2 spiegazioni principali che ho riscontrato in una vasta serie:
- Il precedente chirurgo non ha eseguito una miotomia completa e/o;
- Sono passati molti anni, l’individuo è veramente anziano e ha problemi non con lo sfintere ma con il vigore del lato propulsivo della deglutizione.