Paralisi Unilaterale delle Corde Vocali
La paralisi monolaterale delle corde vocali è l’incapacità neurogena di muovere una corda vocale. È associata a una voce debole di intensità variabile da individuo a individuo.
Vedi anche: Paralisi delle corde vocali, bilaterale, Paresi delle corde vocali.
Quali Sono le Cause della Paralisi delle Corde Vocali?
Se il nervo laringeo ricorrente viene danneggiato in qualsiasi punto del percorso dal tronco encefalico alla laringe, alcuni o tutti i muscoli delle corde vocali potrebbero risultare indeboliti (paretici) o completamente immobilizzati (paralizzati), compromettendo così la voce o la respirazione della persona.
Il Nervo Può Guarire da Solo?
Se il nervo danneggiato è ancora intatto, può guarire da solo, completamente o almeno quanto basta per soddisfare le esigenze vocali della persona. Questo recupero può richiedere fino a un anno perché il tessuto nervoso guarisce molto più lentamente della pelle o persino delle ossa.
A volte, però, il nervo non guarisce, o non abbastanza da soddisfare le esigenze vocali della persona. Non è necessario attendere una potenziale guarigione se un tumore ha invaso il nervo o se si sa che il nervo è reciso.
Paralisi delle Corde Vocali Definita dalla Denervazione di 3 Muscoli Individuali Piuttosto che dalla Mancata Funzionalità del Nervo Ricorrente
La paralisi delle corde vocali è solitamente definita come una corda immobile e il pensiero corre direttamente alla lesione del nervo ricorrente. La “definizione” visiva più universalmente utilizzata è la perdita di abduzione (sebbene vi sia anche una perdita di compressione mediale). In altri termini, tendiamo a pensare che il nervo ricorrente sia “fuori uso”, ma non che i tre muscoli individuali siano denervati di conseguenza. Al contrario, la paresi è definita dalla denervazione di uno (o due) dei seguenti muscoli:
- Cricoaritenoide posteriore (PCA)
- Cricoaritenoide laterale (LCA)
- Tiroaritenoide (TA)
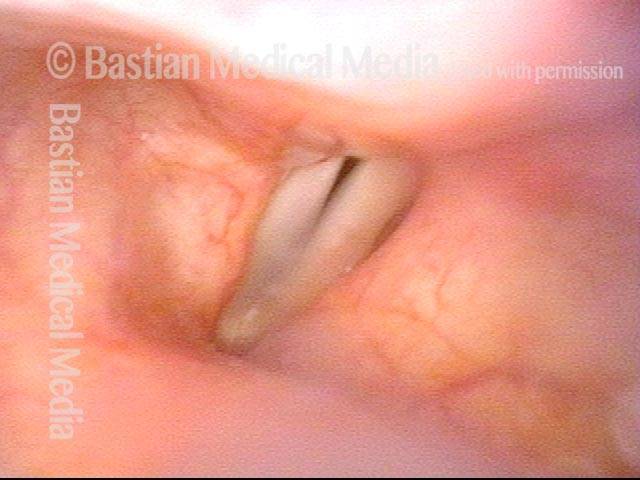
Tornando al termine “paralisi”, si potrebbe definire come la denervazione di tutti e tre i muscoli: PCA, LCA e TA. Questo è chiaramente mostrato nella seguente serie di immagini. Si noti che in genere omettiamo il muscolo interaritenoideo (IA) perché è innervato bilateralmente e non sembra spesso essere presente nella paralisi delle corde vocali.
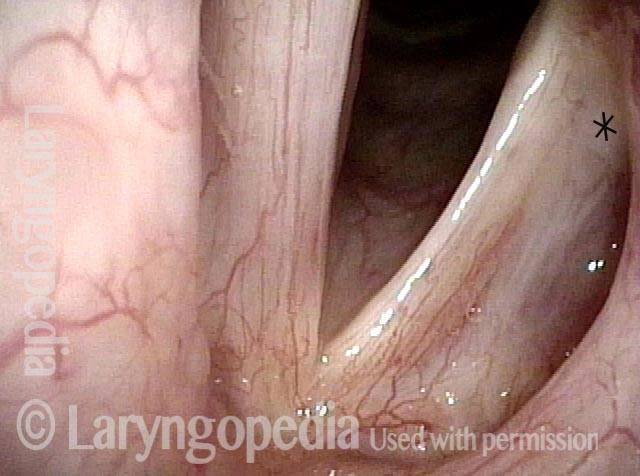
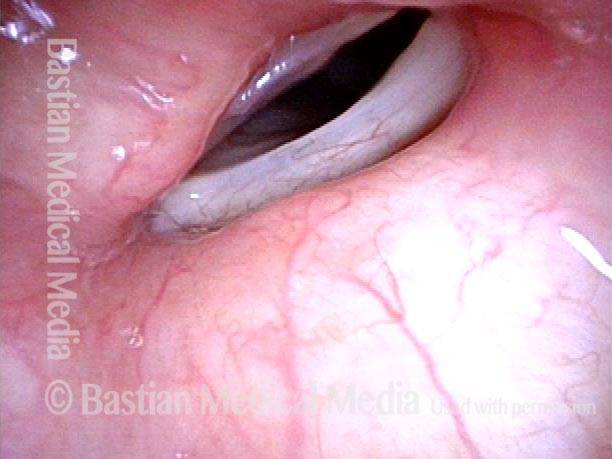
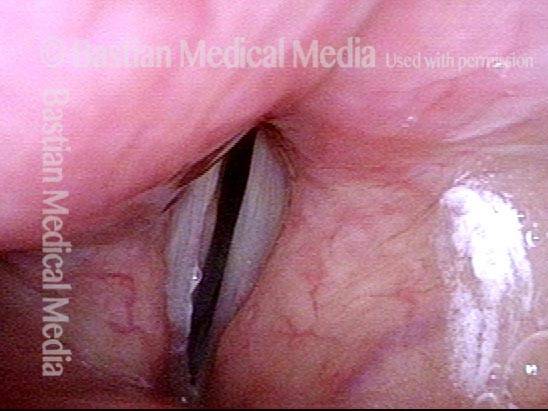
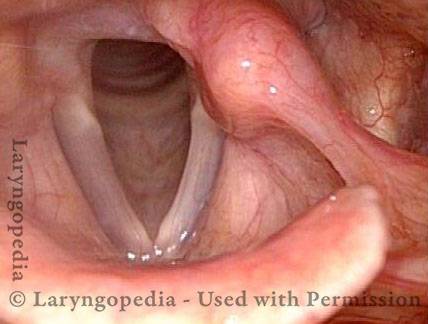
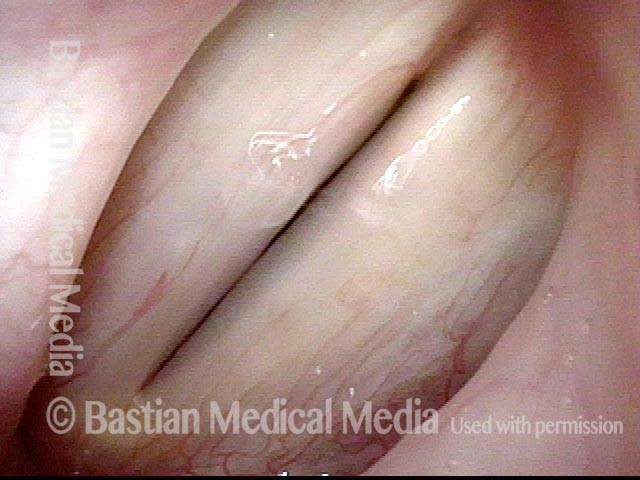
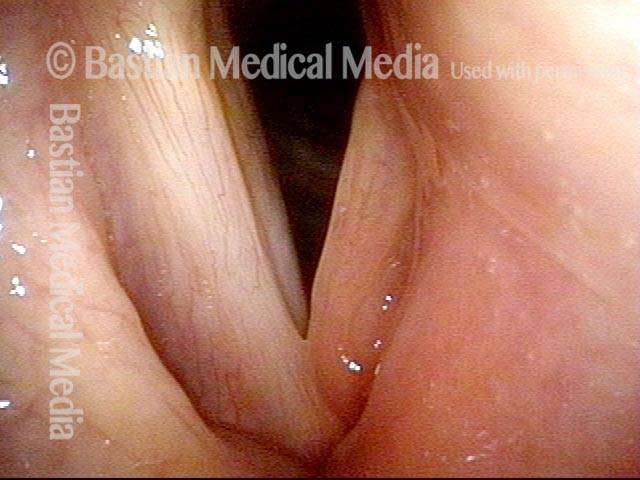
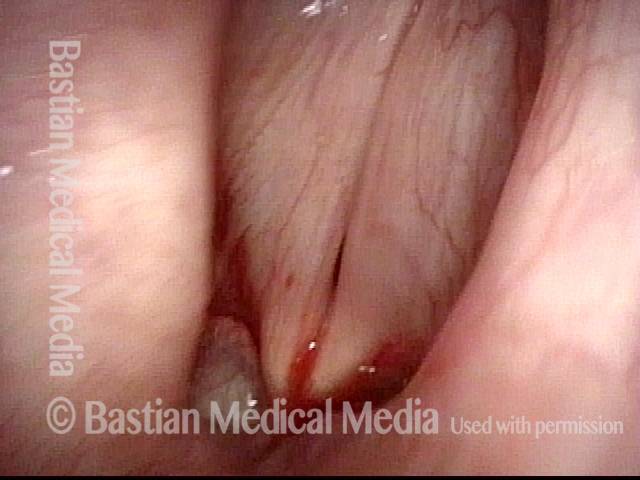
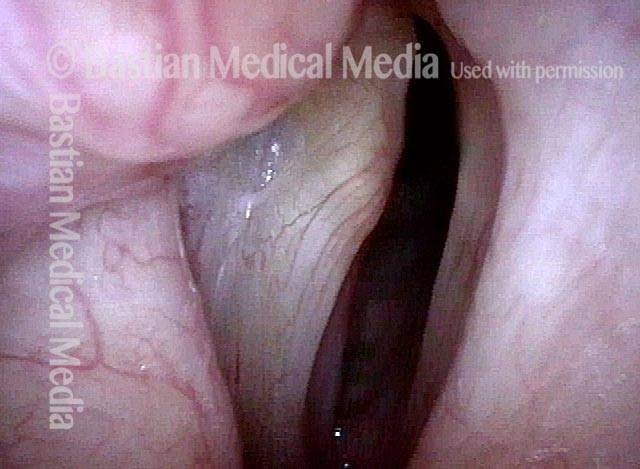
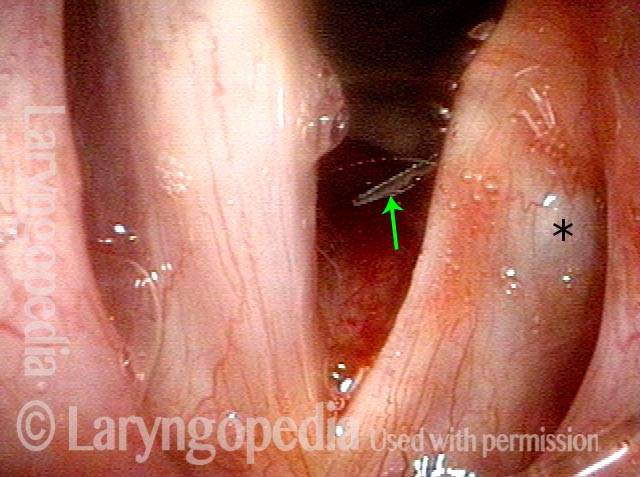
Muscolo PCA non lateralizzante (1 di 3)
In questa vista aperta (con respirazione), la corda sinistra (a destra nella foto) è completamente abdotta. L’intera foto è ruotata in senso antiorario, dando l’impressione che anche la corda destra (a sinistra nella foto) sia lateralizzata. In realtà è paramediana. Questo dimostra che il muscolo PCA non sta lateralizzando la corda destra.
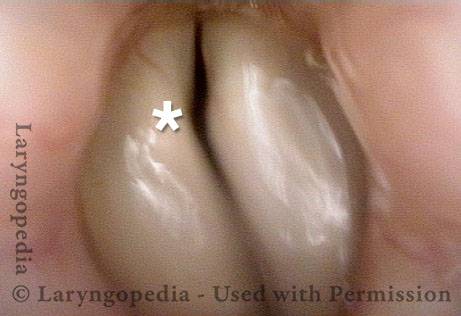
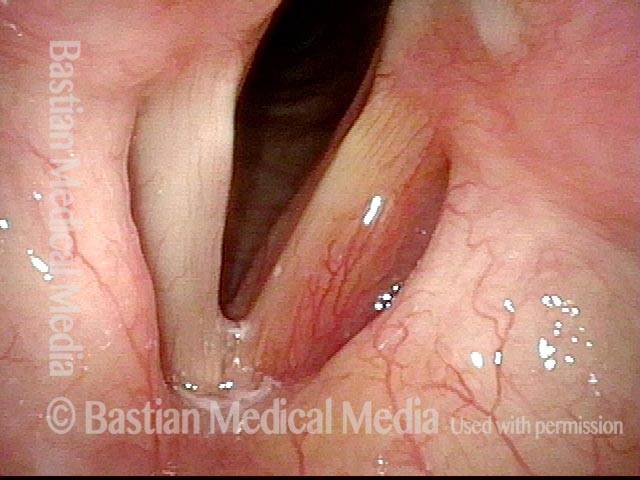
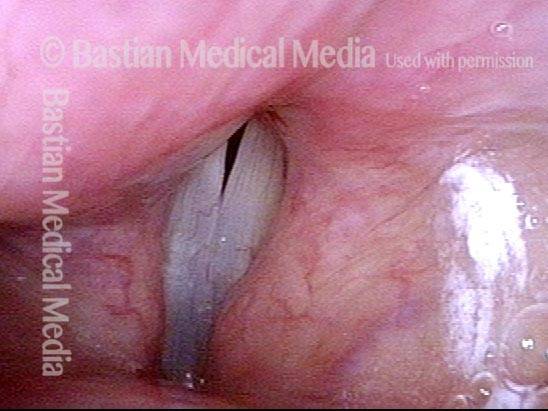
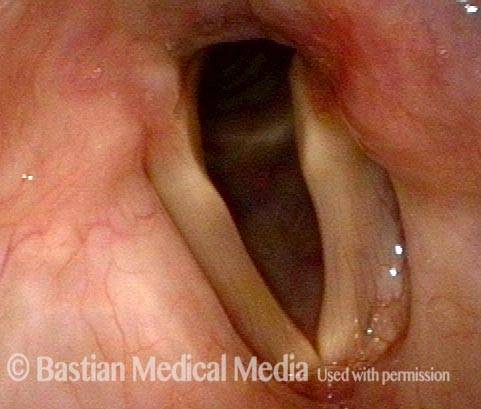
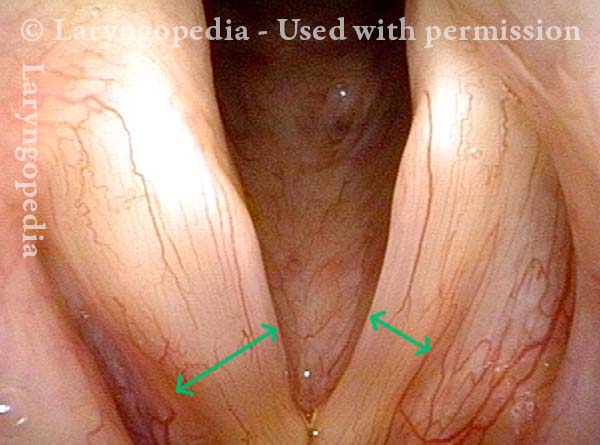
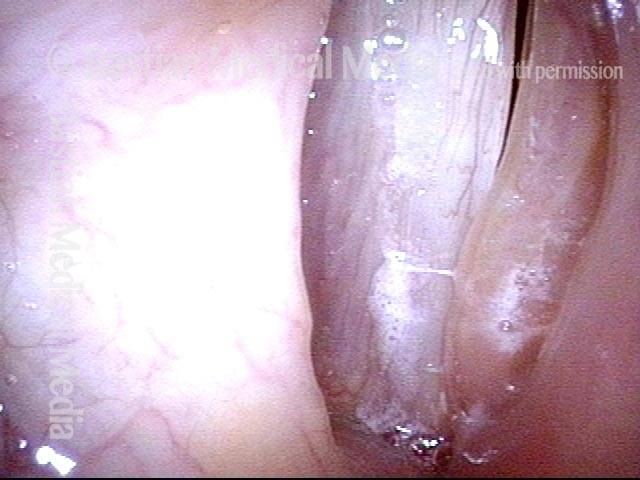
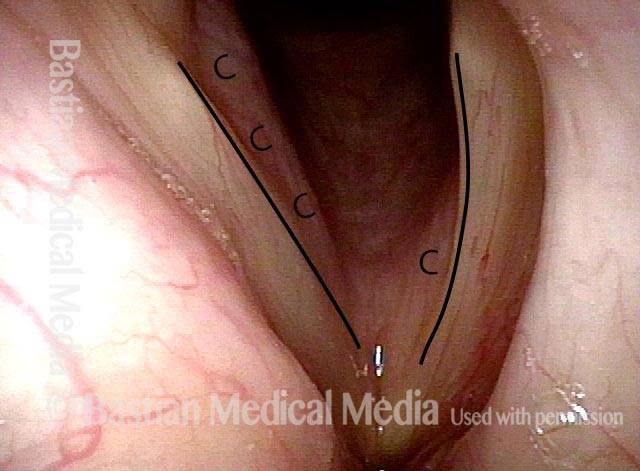
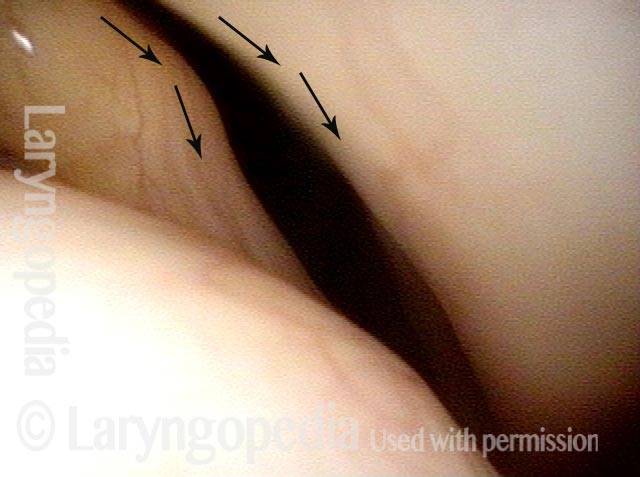
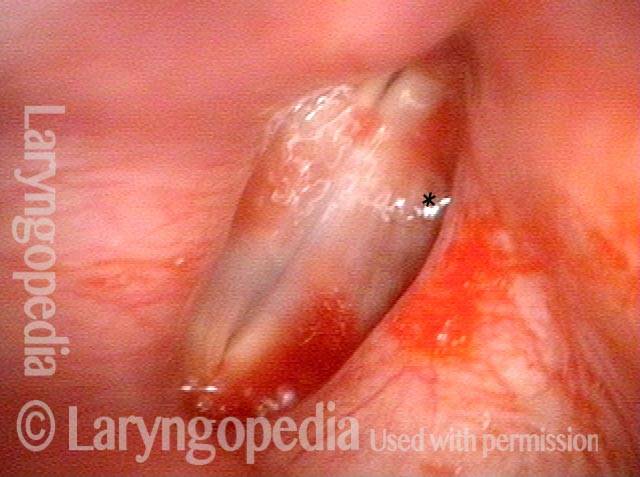
Perdita della funzione LCA (2 di 3)
Durante la fonazione, si noti che la punta del processo vocale destro in corrispondenza di * punta lateralmente, anziché in linea con il resto della corda. Ciò indica la perdita della funzionalità dell’LCA.
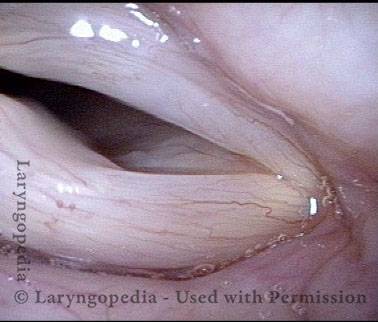
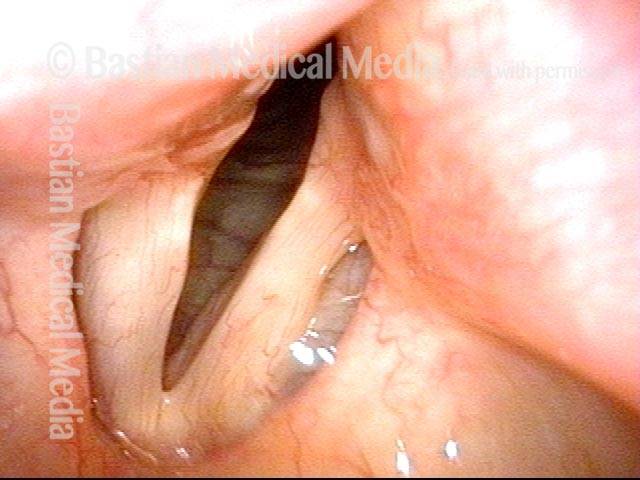
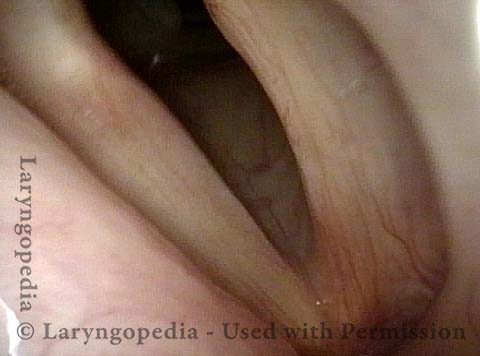
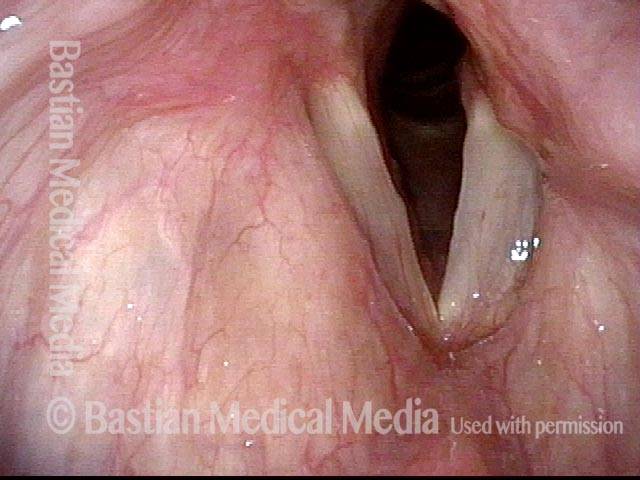
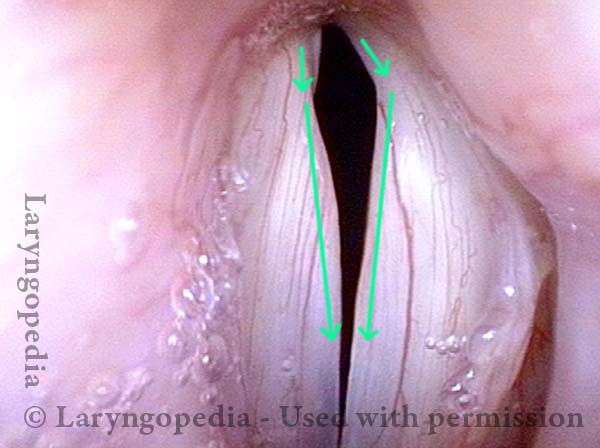
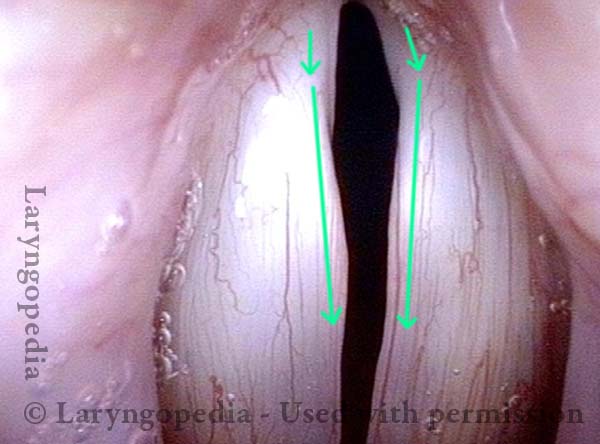
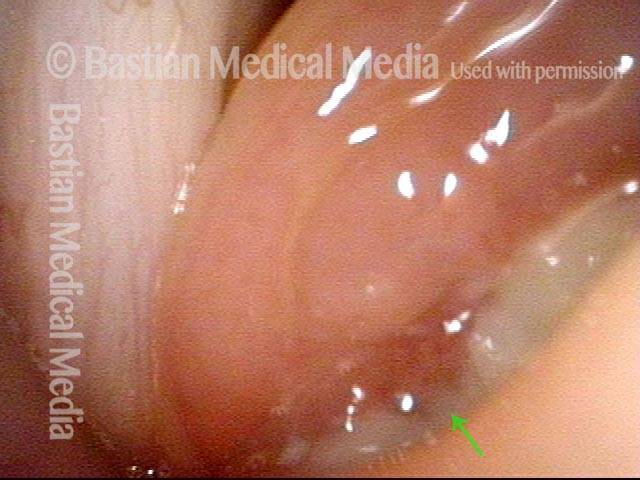
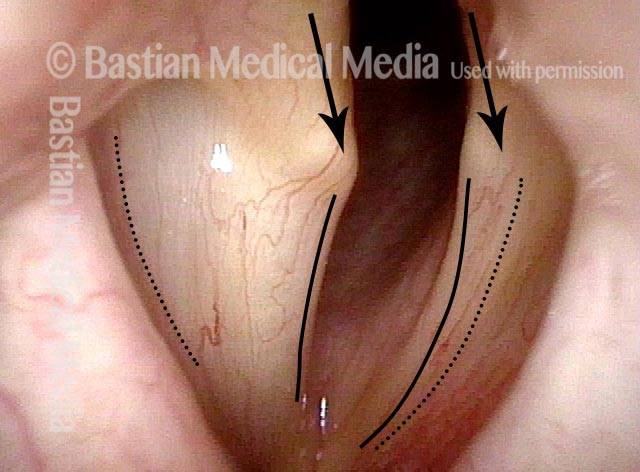
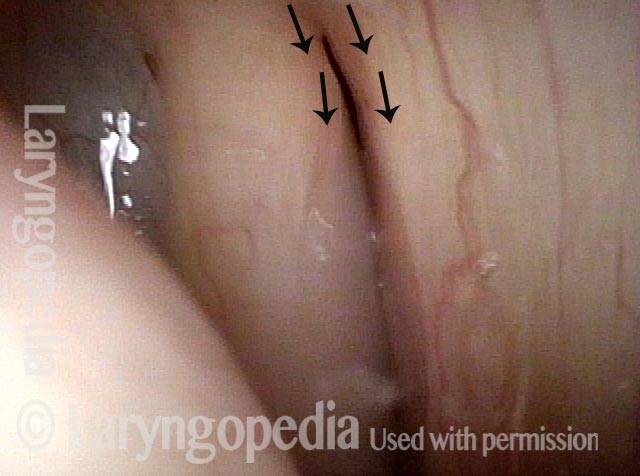
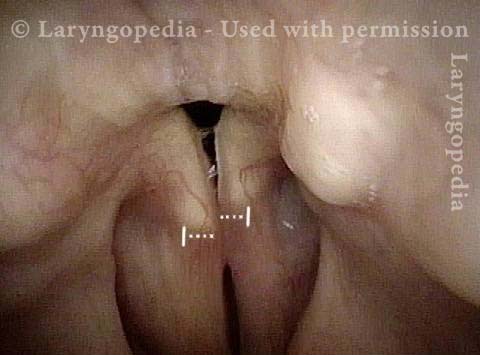
Denervazione dell’TA (3 di 3)
Sotto la luce stroboscopica, si noti l’ampiezza molto maggiore (escursione laterale) del midollo destro (parte inferiore della foto), compatibile con la denervazione e la flaccidità dell’TA.
Sintomi
Uno degli scenari più comuni è che, dopo le indagini, la causa sia sconosciuta: questi casi vengono definiti idiopatici. In questi casi, si sospetta un coinvolgimento virale.
Altre due cause di paresi o paralisi sono tumori e traumi. In questi casi, i tumori possono essere localizzati alla tiroide, ai polmoni, all’esofago, ecc. I traumi sono spesso dovuti a interventi chirurgici eseguiti lungo il percorso del nervo vago, come nel caso di problemi alla tiroide, alla colonna vertebrale, ai polmoni o al cuore.
Altri sintomi possono includere:
- Disfonia debole con perdita d’aria: la voce può essere affannosa, debole, a doppia tonalità o manifestamente strozzata. La persona potrebbe essere in grado di pronunciare solo poche parole con un solo respiro o non essere in grado di proiettare la voce in luoghi rumorosi.
- Impossibilità di essere uditi in luoghi rumorosi.
- Tendenza della voce a essere leggermente più forte al mattino, ma ad “affievolirsi” con l’uso.
- Tendenza a tossire quando si bevono liquidi poco consistenti.
Esami che possono essere eseguiti
Videostroboscopia Laringea
Se eseguito a distanza ravvicinata, questo esame aiuta a determinare quali muscoli sono interessati.
CT
Questo esame aiuta a escludere lesioni massive lungo il decorso del nervo. La TC non è necessaria se la causa è già nota (ad esempio, intervento chirurgico alla tiroide).
EMG
Questo esame è facoltativo/controverso e non necessario nelle cliniche in cui viene eseguita una videostroboscopia laringea a distanza ravvicinata.
Opzioni di trattamento
Non fare nulla
- Accettare semplicemente i sintomi nell’attesa, soprattutto se si ritiene possibile una guarigione (ad esempio dopo un intervento chirurgico alla tiroide con un nervo intatto o dopo una presunta lesione virale).
Esercizi vocali con un logopedista
- Di solito utili se il paziente è taciturno. Ad alcuni pazienti viene erroneamente consigliato (da familiari o amici benintenzionati) di far riposare la voce. Il riposo vocale è in realtà controproducente, tranne quando l’affaticamento generale causato dall’uso di una voce che perde aria rende appropriato un breve riposo vocale.
Gel vocale (laringoplastica iniettiva) – un impianto iniettato a lento assorbimento e quindi temporaneo
- Questo non è per il ripristino definitivo della voce, ma può offrire un aiuto in attesa di una possibile guarigione. L’obiettivo è un beneficio modesto o maggiore.
- Gli impianti di gel vocale vengono spesso eseguiti in ambulatorio con anestesia topica e, occasionalmente, una leggera sedazione. Il gel, acido ialuronico, si infiltra nel tessuto per rimpolparlo e rassodarlo in modo che l’altra corda vocale abbia un punto di pressione.
- La durata del beneficio è in genere di quattro-dodici settimane, poiché il gel si assorbe lentamente. Si spera che il recupero del nervo avvenga durante questo periodo, ma l’iniezione può essere ripetuta se il beneficio svanisce prima che sia appropriato posizionare un impianto permanente.
Gel vocale + idrossiapatite — Un impianto iniettato semipermanente
- Questa opzione viene utilizzata principalmente se il paziente non desidera una laringoplastica di medializzazione (opzione n. 5 di seguito). Se il posizionamento del filler non è ideale, potrebbe essere necessario un aggiustamento chirurgico.
Laringoplastica di medializzazione con un impianto in silastic
- Questo intervento viene eseguito in sala operatoria ambulatoriale in anestesia locale con sedazione profonda (“crepuscolo”). L’intervento chirurgico richiede un’incisione orizzontale di circa 2,5 cm sulla parte anteriore del collo e prevede il posizionamento di un cuneo o “spessore” per medializzare e irrigidire permanentemente la corda vocale paralizzata.
- Vi sono piccoli rischi di lividi e infezioni. Circa un paziente su dieci necessita di un secondo intervento in sala operatoria per aggiustare l’impianto.
Cosa Aspettarsi Dopo la Medializzazione?
- Devo far riposare la voce? No. Usatela “con prudenza” per qualche giorno.
- Quanto tempo ci vorrà perché la mia voce guarisca? La voce sarà rauca per alcuni giorni o settimane prima di “assestarsi”. Alla luce di ciò, la maggior parte dei pazienti si prende da pochi giorni a una settimana di pausa dal lavoro.
- Quanto miglioramento posso aspettarmi? Un buon risultato consiste nel passare dal 20% al 70-80% della voce normale, ma non è garantito.
- Cosa succede se non sono soddisfatto del risultato? A volte aspettiamo un’ulteriore evoluzione; a volte proviamo qualche seduta di logopedia; a volte eseguiamo un intervento chirurgico di revisione. Tutto questo dipende dalle esigenze del paziente e da altri dettagli.
È Necessario un Intervento Chirurgico per la Paralisi delle Corde Vocali?
Purtroppo non c’è molto che si possa fare per accelerare la guarigione. Nel reportage fotografico “Paresi delle Corde Vocali Accentuata dal Disuso“, la paziente ha avuto un recupero spontaneo sufficiente a restituirle una voce “adeguata”. La cosa principale è NON far riposare la voce come ha fatto questa donna, poiché questo non fa altro che atrofizzare qualsiasi muscolo ancora funzionale. E si può provare a “costruire” la voce per vedere se si ottiene un aumento di forza.
Se queste soluzioni non funzionano e sono trascorsi 9 mesi o più dall’inizio della paralisi, le uniche opzioni sono accettare la “nuova” voce o procedere con la medializzazione.
Tenete presente che un tipo di medializzazione è una semplice iniezione (opzioni #3 e #4), mentre l'altro è un intervento chirurgico attraverso un'incisione di circa 2,5 cm (opzione #5).
Paralisi delle Corde Vocali Definita dalla Denervazione di 3 Muscoli Individuali Piuttosto che dalla Mancata Funzionalità del Nervo Ricorrente
La paralisi delle corde vocali è solitamente definita come una corda immobile e il pensiero corre direttamente alla lesione del nervo ricorrente. La “definizione” visiva più universalmente utilizzata è la perdita di abduzione (sebbene vi sia anche una perdita di compressione mediale). In altri termini, tendiamo a pensare che il nervo ricorrente sia “fuori uso”, ma non che i tre muscoli individuali siano denervati di conseguenza. Al contrario, la paresi è definita dalla denervazione di uno (o due) dei seguenti muscoli:
- Cricoaritenoide posteriore (PCA)
- Cricoaritenoide laterale (LCA)
- Tiroaritenoide (TA)
Tornando al termine “paralisi”, si potrebbe definire come la denervazione di tutti e tre i muscoli: PCA, LCA e TA. Questo è chiaramente mostrato nella seguente serie di immagini. Si noti che in genere omettiamo il muscolo interaritenoideo (IA) perché è innervato bilateralmente e non sembra spesso essere presente nella paralisi delle corde vocali.
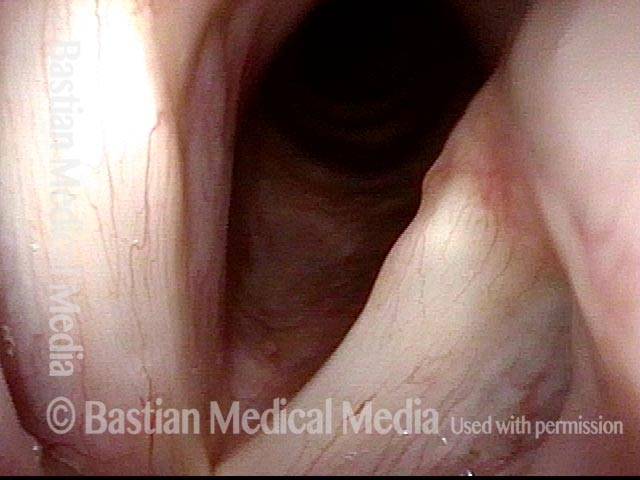
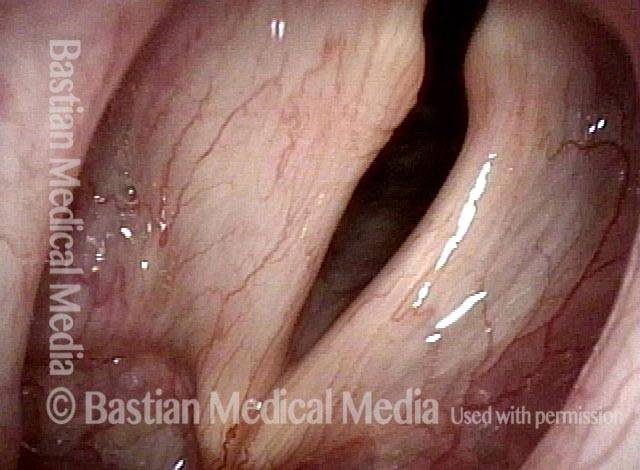
Paralisi delle corde vocali: prima della medializzazione (1 di 12)
Un classico esempio di corde vocali “a spaghetti-linguine”, qui in posizione di respirazione. La corda “a linguine” (a sinistra nell’immagine) è normale; la corda “a spaghetti” (a destra nell’immagine) è paralizzata, probabilmente dalla nascita. Sul lato paralizzato, si noti il ventricolo profondo e ampio, la lieve curvatura del margine della corda e la ridotta larghezza della superficie superiore della corda (simile a “spaghetti”), rispetto al lato non paralizzato.

Paralisi delle corde vocali: prima della medializzazione (2 di 12)
Fonazione, visione più distante, con luce standard. Si noti il notevole spazio tra le corde vocali. Questo spazio è correlato alla qualità della voce debole e con perdita d’aria del paziente.
Aumento dell’ampiezza + incurvamento (3 di 12)
Open phase of vibration, under strobe light. The paralyzed cord (right of image) has a much increased amplitude (lateral or outward excursion) and exaggerated bowing, due to its flaccidity.

Il midollo paralizzato non può chiudersi (4 di 12)
“Closed” phase of vibration, which is of course not closed at all, because the paralyzed cord (right of image) cannot come fully to the midline.
I sintomi visivi sono diminuiti (5 su 12)
One week after surgical medialization of the paralyzed cord (right of image), using a silastic implant buried deeply within the cord. Notice that the ventricle is no longer capacious, and the free margin is no longer bowed. Furthermore, in contrast with photo 1 of this series, the “spaghetti-linguine” description of these vocal cords is no longer apt.

Il divario è sparito! (6 di 12)
Fonazione, in condizioni di luce standard. Lo spazio tra le corde vocali non è più visibile (confronta con la foto 2) e la voce spontanea della paziente suona normale. Riesce a ottenere un volume sonoro efficace senza alcun affaticamento o debolezza osservabile.

Escursione laterale simile (7 di 12)
Fase aperta di vibrazione, sotto luce stroboscopica. L’escursione laterale o verso l’esterno del midollo paralizzato (a destra dell’immagine) è ora simile a quella del midollo non paralizzato. Confrontare con la foto 3.

Fase chiusa migliorata (8 su 12)
La fase chiusa della vibrazione è molto più chiusa rispetto alla fase preoperatoria. Confrontare con la foto 4.
5 mesi dopo la medializzazione (9 su 12)
Cinque mesi dopo la medializzazione. Confrontate questa posizione parzialmente abdotta con le foto 1 e 5 di questa serie.
5 mesi dopo la medializzazione (10 di 12)
Fonazione, in condizioni di luce standard, che mostra una sfocatura vibratoria. Confrontare con le foto 2 e 6 di questa serie.
5 mesi dopo la medializzazione (11 di 12)
Fase aperta di vibrazione, sotto luce stroboscopica. Come nella foto 7 di questa serie, e a differenza della foto 3, l’impianto non consente al midollo paralizzato (a destra nell’immagine) di “piegarsi” lateralmente o verso l’esterno. Anzi, l’escursione vibratoria del midollo non paralizzato (e non impiantato) è maggiore di quella del midollo paralizzato impiantato.
5 mesi dopo la medializzazione (12 di 12)
La fase chiusa della vibrazione è ora praticamente normale, simile alla foto 8 e in contrasto con la foto 4.
Evoluzione della Paralisi delle Corde Vocali: Paresi Solo della PCA
Per alcuni foniatri, la misurazione è considerata più importante dell’osservazione. Entrambe sono legittime, ovviamente, tuttavia la comprensione visiva (osservazione) della paralisi e della paresi rimane molto più utile delle misurazioni EMG, acustiche o aerodinamiche. Questo caso illustra chiaramente questo punto.
Questo uomo anziano è stato sottoposto a un intervento chirurgico toracico, ma a causa di complicazioni è stato anche intubato per gran parte di due giorni. Subito dopo il risveglio, la sua voce era alterata. Ha affermato di essere solo sussurrata.
Alla sua prima visita ambulatoriale, un mese dopo, pensava che la sua voce fosse migliorata al “10%” e l’esame ha mostrato una paralisi della corda vocale sinistra (muscoli TA, LCA e PCA tutti non funzionali). Tre mesi dopo, la sua voce era, secondo la sua descrizione, al 40% e migliorava ulteriormente di settimana in settimana. All’ottavo mese post-operatorio, verificato a 18 mesi, riteneva che la sua voce fosse recuperata al “99%”; l’esame ha mostrato il recupero di TA e LCA, ma non del muscolo PCA.
Diagnosi finale: paresi solo della PCA sinistra. Invece di essere completamente "fuori uso", la PCA sembra solo debole.
Incurvamento del margine del midollo spinale sinistro (debolezza dell’AT) (1 di 11)
Un mese dopo l’intervento chirurgico toracico che ha ridotto la voce dal “100%” preoperatorio a “0” postoperatorio (solo sussurro). La posizione respiratoria (parzialmente aperta) mostra un incurvamento del margine sinistro del midollo spinale (a destra nella foto).
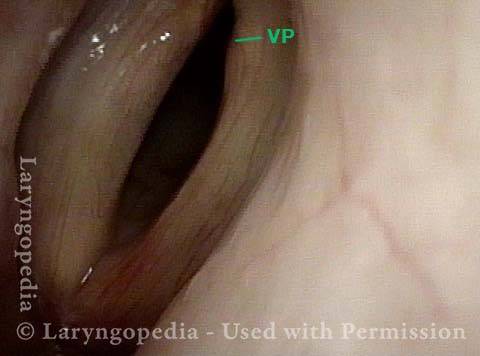
Paresi LCA identificata (2 di 11)
Poco prima dell’inizio della vibrazione (fonazione), si nota un ampio spazio tra le corde. L’incurvamento/atrofia correlata all’AT sinistro rimane evidente e la punta del processo vocale (VP) è ruotata lateralmente, a indicare debolezza del muscolo LCA sinistro.

La voce è sussurrata! (3 di 11)
Ora si crea una voce estremamente sussurrata (vedi sfocatura vibratoria) con un tempo di fonazione di pochi secondi a causa dello spreco d’aria tra le corde vocali. Due muscoli fondamentali per la produzione della voce, TA e LCA, non funzionano.
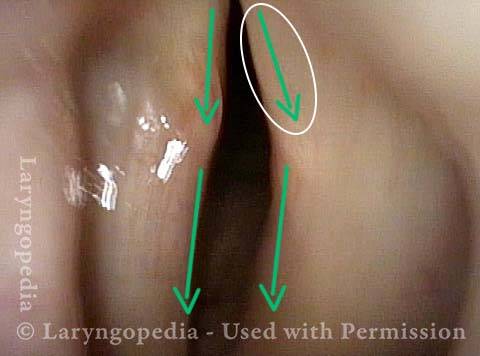
LCA Paresi Vista Migliore (4 di 11)
La vista principale si ha durante la vocalizzazione, quando si apprezza la debolezza dell’LCA notando la rotazione laterale del processo vocale sinistro (freccia cerchiata).

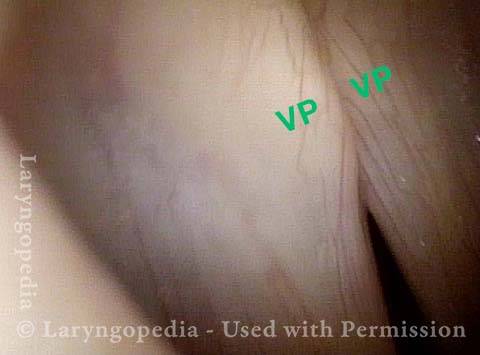
4 mesi dopo, la glottide si apre per respirare (5 di 11)
Ora, a 4 mesi dall’infortunio, questa vista è ruotata; la corda sinistra (a destra nella foto) è lateralizzata e la corda sinistra (curvata) è in realtà sulla linea mediana. La leggera rotazione mediale del processo vocale (VP) è immaginaria? Questo sarebbe in linea con il commento del paziente secondo cui la voce è notevolmente migliorata e continua a migliorare di settimana in settimana.

Gap durante la fonazione minore (6 di 11)
Durante la fonazione, la distanza tra le corde vocali è minore rispetto alla Foto 4 e la rotazione laterale del processo vocale sinistro (freccia) è meno accentuata. Ciò suggerisce un lieve recupero del muscolo LCA sinistro.
Escursione laterale simile (7 di 12)
A 8 mesi dall’infortunio, il paziente afferma che la sua voce è completamente recuperata. In questa posizione respiratoria, si può osservare che il muscolo PCA sinistro, che dovrebbe lateralizzare quella corda, non funziona ancora, il che spiega la posizione mediana della corda sinistra (a destra nella foto). Naturalmente, il deficit del muscolo PCA non influisce sulla voce, ma solo sulle dimensioni dell’apertura glottica durante la respirazione… Tuttavia, il tono del muscolo LCA sta chiaramente ruotando il processo vocale verso la medialità.
LCA recuperato: il processo vocale ora gira medialmente (8 di 11)
Entrambi i processi vocali ruotano medialmente per la fonazione, il che suggerisce il recupero del muscolo LCA sinistro, anche se il processo vocale destro si sposta sopra quello sinistro (cosa che si osserva non di rado nelle laringi più vecchie).

A 18 mesi, il midollo spinale sinistro non si abduce a causa della persistente debolezza della PCA (9 di 11)
A 18 mesi, e continua a sentire la voce normale. In questa posizione respiratoria, l’apertura glottica è ridotta perché la corda sinistra non si lateralizza, il che è compatibile con la debolezza persistente del muscolo PCA sinistro. L’incurvamento non è significativo perché la debolezza del PCA, abbinata a TA e LCA normali, crea un incurvamento durante la respirazione, anche nei bambini. Vedi anche la foto successiva.
La PCA sinistra può presentare una certa lateralizzazione (10 di 11)
Quando il paziente annusa, il suo debole muscolo PCA sinistro lateralizza in qualche modo il midollo, eliminando la “curvatura” visibile nella foto 9.

Recupero completo della voce, nonostante la paresi solo della PCA (11 di 11)
Nell’istante prefonatorio, entrambi i processi vocali entrano in contatto in linea retta (confronta con le foto 4 e 6). Tieni presente che la debolezza della PCA da sola non influisce sulla voce, ma la paresi della sola PCA si osserva solo durante la respirazione, come nella foto 10.
Laringoplastica Iniettiva con gel Temporaneo
Laringoplastica (1 di 4)
Questa persona si è svegliata con una voce debole e sussurrata dopo un intervento chirurgico addominale d’urgenza. Ora, a distanza di oltre 3 mesi, la voce sta tornando gradualmente, ma è ancora molto debole. In questa foto, il paziente respira tranquillamente. La corda vocale sinistra, debole, è più arcuata della destra.

Motivo dello spreco d’aria (2 di 4)
Quando cerca di produrre una voce, la corda vocale sinistra arriva solo in parte alla linea mediana, lasciando un ampio spazio che spiega la sua voce sussurrata e che spreca aria.

Gel vocale iniettato nella corda vocale (3 di 4)
Lo stesso giorno, a causa dell’urgente necessità del paziente, la corda vocale sinistra è stata “riempita” con un gel vocale. Questo materiale in genere offre un beneficio temporaneo di 6-12 settimane, con un assorbimento graduale durante tale periodo.

Le corde vocali si chiudono completamente (4 di 4)
La voce è notevolmente migliorata, ora che le sue corde vocali possono chiudersi più completamente, riducendo lo spreco d’aria e trasformando la voce da sussurrata a forte. Confronta con la foto 2.
Esempi di Paralisi
Paralisi delle corde vocali (1 di 2)
Paralisi della corda vocale sinistra (a destra dell’immagine), posizione respiratoria. Si noti che la corda sinistra è arcuata e atrofizzata rispetto alla destra.

Paralisi delle corde vocali (2 di 2)
Lo stesso paziente durante la fonazione mostra che le corde non si avvicinano; ciò è correlato a una qualità della voce debole, affannosa e che spreca aria.
Esempio 2
Paralisi delle corde vocali (1 di 5)
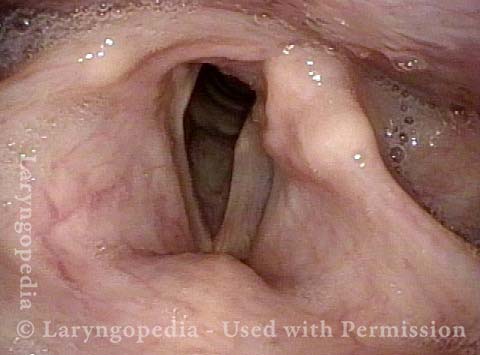
Questa persona ha una voce estremamente debole e che spreca aria. In questo caso, con le corde vocali in posizione di respirazione, la causa di questo problema vocale non è ancora evidente.

Fonazione (2 di 5)
La causa del problema non è ancora evidente.
Vista più ravvicinata (3 di 5)
La spiegazione diventa più evidente. Come si vedrà in seguito, questo paziente presenta una paralisi della corda vocale sinistra (a destra dell’immagine); ovvero, i muscoli TA, LCA e PCA di quel lato sono tutti interessati. Qui si nota meglio l’indebolimento della TA (curvatura del margine libero, perdita di volume della corda sinistra, soprattutto nell’area del “cono”, e dilatazione del ventricolo). La corda è paramediana, il che suggerisce che anche il muscolo PCA non funzioni. Il muscolo LCA è tuttavia difficile da valutare in questa proiezione.

Evidenza di debolezza dell’LCA (4 su 5)
Fonazione nel registro toracico basso (si noti l’ampia zona di sfocatura del margine libero della corda vocale). Qui, si osserva chiaramente che il processo vocale si sposta lateralmente (freccia), indicando debolezza dell’LCA, oltre alla debolezza dell’AT e dell’ACP visibile nella foto 3.
Fonazione a tono molto alto (5 di 5)
Fonazione a toni molto alti (quindi, la sfocatura vibratoria si riduce). L’allungamento antero-posteriore della corda sinistra a questo tono acuto sposta il processo vocale sinistro verso la linea mediana (confronta con la foto 2), mascherando la debolezza dell’LCA. Questa differenza tra voce grave e voce acuta nella commessura posteriore si osserva di routine, ma non universalmente, con la debolezza dell’LCA.
Paralisi del Nervo Ricorrente del Ramo Anteriore
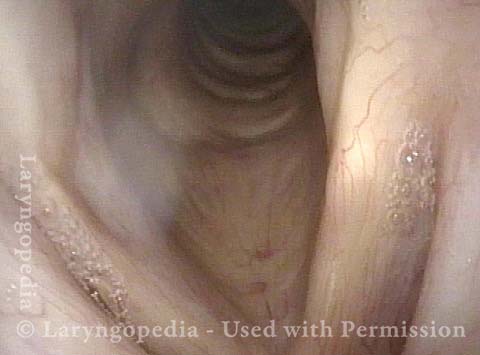
Spaghetti vs linguine (1 di 3)
Respirazione, con pliche in posizione abdotta. Si noti che la corda vocale sinistra è in posizione laterale, suggerendo l’integrità del muscolo cricoaritenoideo posteriore (PCA).
Si noti anche l’incurvamento del margine, il ventricolo capiente e la discrepanza tra “spaghetti (sinistra) e linguine (destra)” della piega muscolomembranosa (confronta parentesi).
Denervazione di TA + LCA (2 di 3)
La fonazione unisce il “tallone” dell’aritenoide grazie all’innervazione bilaterale del muscolo interaritenoideo. Il “dito” destro normale è rivolto in avanti a causa della tensione interna del tiroaritenoideo (TA) e della rotazione mediale del muscolo cricoaritenoideo laterale (LCA).
A sinistra, il processo vocale o “dito” dell’aritenoide ruota lateralmente a causa della denervazione e della conseguente inattività dei muscoli TA e LCA di sinistra.
Allungamento anteriore (3 di 3)
Si noti che alle alte frequenze, il processo vocale della cartilagine aritenoidea sinistra è leggermente ruotato medialmente a causa dello stiramento anteriore fornito dai muscoli cricoaritenoidei (intatti).
Estrusione dell’Impianto della Corda Vocale
Midollo sinistro infiammato (1 di 3)
Paziente con corda vocale sinistra paralizzata (a destra nell’immagine), che diversi anni fa era stata sottoposta con successo alla medializzazione di tale corda con un cuneo di silastic.
Più recentemente, diversi mesi fa, ha notato dolore e gonfiore durante un’intensa attività aerobica e successivamente una voce persistentemente ruvida. Questa immagine mostra che la corda sinistra è infiammata.
Estrusione dell’impianto della corda vocale (2 di 3)
Illuminazione stroboscopica. Notare la forma convessa dell’estremità anteriore del midollo spinale sinistro (quella inferiore, in questa foto). Questa convessità non è causata da una ipermedializzazione, ma dalla reazione infiammatoria.
Impianto esposto (3 di 3)
Una visione più ravvicinata mostra che il problema è l’esposizione dell’impianto in silastic. Il silastic è scoperto in corrispondenza della freccia. Un essudato biancastro ricopre l’impianto esposto rimanente. Questo è un evento raro dopo la medializzazione con un impianto in silastic.
Gel Vocale per un Aiuto Immediato
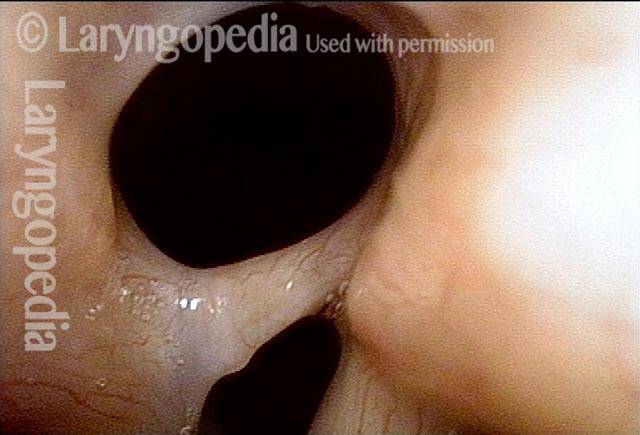
Paralisi della corda vocale sinistra (1 di 4)
Un uomo anziano con paralisi della corda vocale sinistra (a destra nella foto) dopo un intervento chirurgico al torace che ha coinvolto il mediastino superiore. Questa è la massima adduzione all’istante prefonatorio, che mostra incurvamento e atrofia della corda vocale sinistra (a destra nella foto). La voce è estremamente debole e con perdita d’aria.

Iniezione di gel vocale (2 di 4)
All’inizio dell’iniezione di gel vocale in un laboratorio vocale, con il paziente seduto sulla poltrona. La traiettoria dell’ago da 27 gauge è indicata dalla linea tratteggiata. Un secondo bolo di gel verrà iniettato più posteriormente.

Corda più vicina alla linea mediana (3 di 4)
Al termine dell’iniezione, il midollo spinale sinistro risulta ingrossato e spostato verso la linea mediana.
Adduzione completa delle corde! (4 di 4)
Ora le corde vocali possono chiudersi completamente per consentire la produzione vocale. La voce è notevolmente più forte e il paziente può pronunciare molte più parole con un solo respiro prima di rimanere senza fiato.
55 Anni di Paralisi con Ogni Scoperta Classica
Posizione di respirazione, corda sinistra curva (1 di 4)
Voce drasticamente debole dall’età di 21 anni in un uomo che ora ha superato i settant’anni. Posizione respiratoria. La corda destra normale (a sinistra nella foto) è completamente lateralizzata, ha un margine relativamente dritto (vedi linea) e il rigonfiamento del muscolo cono (la superficie inferiore più rosa della corda indicata dalla “C”) è piuttosto pieno. La corda sinistra anomala (a destra nella foto) è paramediana (leggermente laterale alla linea mediana), arcuata (vedi linea) e il suo rigonfiamento del muscolo cono praticamente inesistente (indicato dalla “C”).
Avvicinamento alla posizione di sonorizzazione (2 di 4)
Avvicinamento alla posizione di vocalizzazione in condizioni di luce standard. La corda destra (a sinistra nella foto) è arrivata quasi alla linea mediana. Il processo vocale è rivolto leggermente medialmente (freccia). La corda sinistra (a destra nella foto) mostra un processo vocale rivolto lateralmente (freccia), un margine arcuato (vedi linea) e il suo ventricolo è capiente. Il ventricolo si estende lateralmente dalla linea tratteggiata su ciascuna corda.
Chiusura delle corde vocali, grande spazio (3 di 4)
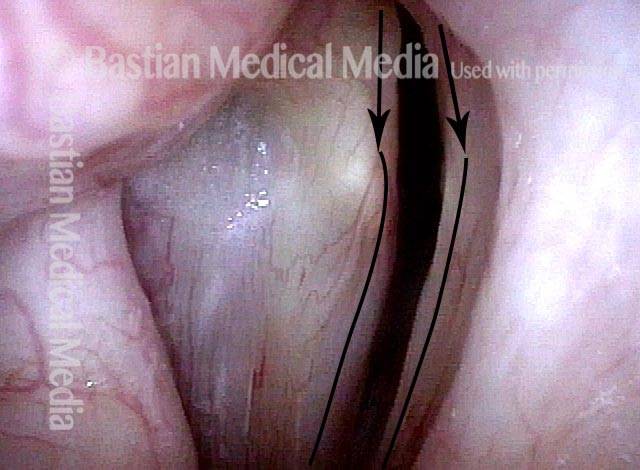
Vocalizzazione sotto luce stroboscopica, alla massima chiusura vibratoria. Un ampio divario spiega la disfonia con conseguente perdita d’aria. Si noti la direzionalità dei processi vocali che sembrano indicare che l’LCA stia lavorando a destra (a sinistra della foto) e non a sinistra (a destra della foto); si noti anche l’incurvamento della corda sinistra (a destra della foto).
Fase aperta della vibrazione, flaccidità della corda destra (4 di 4)
La fase aperta della vibrazione mostra quella che sembra essere flaccidità (escursione laterale molto ampia) del midollo destro (neurologicamente integro) (a sinistra nella foto). La flaccidità nel midollo attivo è spesso osservata: la domanda è se ciò sia funzionalmente “necessario” per consentire la vibrazione. In altre parole, un midollo normalmente teso non riuscirebbe a oscillare con così poca “presa” del flusso d’aria? Oppure la flaccidità è dovuta all’età e alla mancanza di un partner attivo che lo mantenga forte?
La Laringoplastica di Medializzazione in Genere non Risolve il “Reperto” dell’LCA

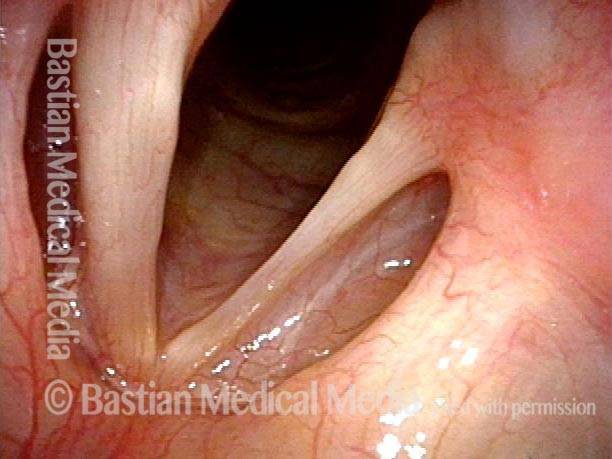
Paralisi della corda vocale sinistra (1 di 4)
Molti anni dopo il trattamento per il cancro ai polmoni, la voce di quest’uomo si è improvvisamente indebolita. Qui vediamo la paralisi della corda vocale sinistra (a destra della foto). Il riscontro più sorprendente (tra i tanti) in questa immagine è l’incurvamento del margine della corda vocale sinistra (confronta le linee tratteggiate a destra della foto).
Inchino durante la fonazione (2 di 4)
Durante la fonazione, il processo vocale destro (a sinistra nella foto) ruota medialmente a causa dell’LCA intatta; a sinistra (a destra nella foto), con l’LCA paralizzata, il processo vocale ruota lateralmente (confronta le frecce posteriori).

Dopo la medializzazione (3 di 4)
Pochi mesi dopo la medializzazione (un impianto posizionato in profondità nella corda vocale sinistra), il margine della corda vocale sinistra è ora dritto anziché arcuato (confronta con la foto 1).
La svolta laterale rimane invariata (4 su 4)
Durante la fonazione, un cambiamento sorprendente è la riduzione dello spazio tra le corde vocali, e questo spiega la sua voce molto più forte. La rotazione laterale del processo vocale sinistro (a destra nella foto) è ancora visibile, tuttavia. La medializzazione tende a “correggere” la flaccidità e la lateralizzazione della corda vocale paralizzata e a ridurre lo spazio tra le corde.
Confronta con la foto 2. Come si vede qui, la rotazione laterale del processo vocale è ancora visibile in una certa misura. Se la voce non fosse così buona e soddisfacente per il paziente, questo riscontro visivo sarebbe un argomento a favore dell’adduzione aritenoidea.
Iniezione di Gel Vocale per la Paralisi delle Corde Vocali
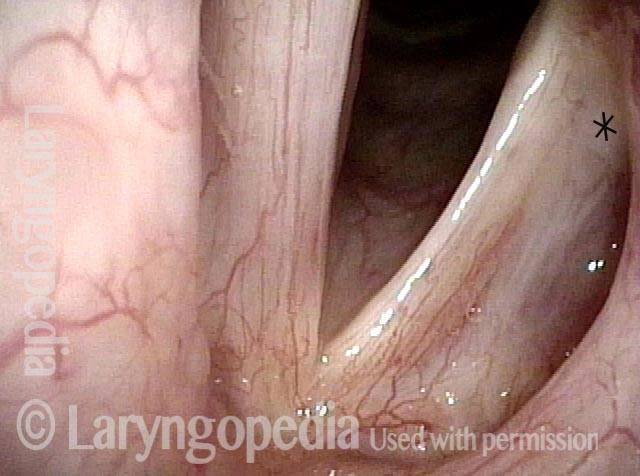
Paralisi della corda vocale sinistra (1 di 4)
Questa foto mostra la paralisi della corda vocale sinistra in posizione respiratoria. Si noti l’incurvamento del margine, la differenza di volume a “spaghetti-linguine” e il ventricolo capiente. Nota: l’asterisco (*) è per il confronto con la foto 3.

Posizione di emissione della voce (2 di 4)
Qui la paralisi è mostrata nella posizione di emissione vocale. Si noti la flessione laterale della corda vocale sinistra (a destra nella foto). Questa flaccidità e la distanza tra le corde vocali spiegano la qualità della voce affannosa (che perde aria) del paziente.
Iniezione di gel vocale (3 di 4)
Questo è lo stesso paziente all’inizio dell’iniezione di gel vocale. L’ago in corrispondenza della freccia proviene dalla sottoglottide verso l’alto e lateralmente. In * si può osservare l’inizio del rigonfiamento nel ventricolo posteriore. Anche la corda vocale appare leggermente spostata verso la linea mediana. Confrontare con la foto 1.
Dopo l’iniezione di gel vocale (4 di 4)
La posizione di emissione vocale dopo l’iniezione di gel vocale è completa e il rigonfiamento nel ventricolo a * è più evidente. La chiusura è molto migliore; la voce è notevolmente più forte e la perdita d’aria è molto minore. Confrontare con la foto 2.
La Discrepanza Aritenoidea che Causa una Qualità della Voce Roca è Difficile da Risolvere in Alcuni Casi di Paralisi delle Corde Vocali

Le aritenoidi non si allineano (1 di 5)
Quest’uomo aveva una corda vocale sinistra paretica. Alla diagnosi, le aritenoidi non erano compatibili. Dopo l’inserimento di un impianto alle corde vocali, ha riacquistato una buona forza, ma la sua voce è rimasta roca. A distanza ravvicinata, in posizione abdotta, la “massa” di entrambe le corde vocali appare simile.

Processi vocali (2 di 5)
A media distanza, quando le corde vocali cominciano a chiudersi, le punte dei processi vocali non sembrano allineate (asterischi), in modo simile a quanto accade prima dell’impianto.
I processi vocali non corrispondono quando si tocca (3 di 5)
Non appena i processi vocali entrano in contatto tra loro, si nota più chiaramente che le punte dei processi vocali non coincidono (vedere le linee tratteggiate).

Corde vocali disallineate (4 di 5)
Ora in pieno contatto fonatorio (vocale), l’aritenoide destro si solleva sopra la corda vocale sinistra. Anche le punte dei processi vocali rimangono disallineate (linee tratteggiate). Anche i ventricoli posteriori non coincidono (linee curve).

Vibrazione asimmetrica (5 di 5)
Considerando la diversa lunghezza effettiva delle corde membranose e la sovrapposizione della corda destra sulla sinistra, per non parlare dell’impianto nella corda sinistra, la vibrazione asimmetrica non sorprende. La voce è forte, ma roca.
Qual è la Soluzione?
Si potrebbe medializzare in modo più aggressivo posteriormente a sinistra, sperando di aumentare il livello della corda, ma spesso i tentativi di compensare la discrepanza aritenoidea, come quella osservata qui, hanno solo un modesto successo. La sovrastruttura aritenoidea non è utile per la valutazione della corrispondenza; l’esaminatore dovrebbe invece valutare la corrispondenza a livello dei processi vocali.
Sinechie della Commissura Posteriore

Corde vocali legate (1 di 5)
Quest’uomo è affetto da paralisi della corda vocale destra e, decenni fa, ha subito un’iniezione di Teflon nella corda vocale destra, con conseguente sinechia commissurale posteriore. Ha difficoltà a respirare, in parte a causa della fascia tissutale e in parte perché questa mantiene le corde vocali più vicine di quanto sarebbe altrimenti necessario, come si vede nella foto 4 dopo la rimozione della fascia. Vedi anche la foto 5.
Corde vocali legate (2 di 5)
A distanza ravvicinata.
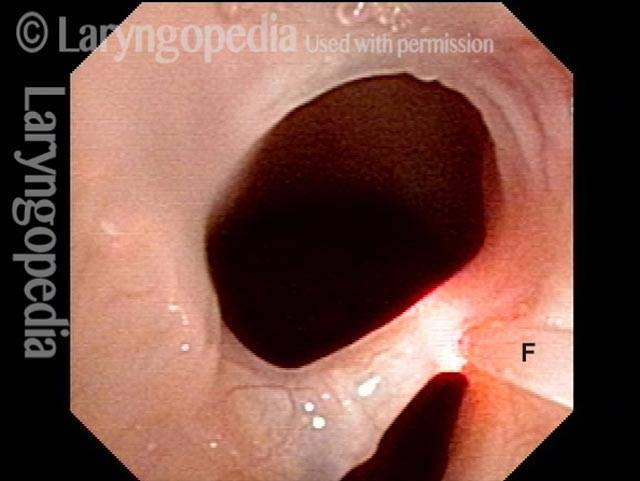
Prima della rimozione laser (3 di 5)
La fibra laser al tulio (F) tocca le sinechie e l’energia laser sta per essere erogata.
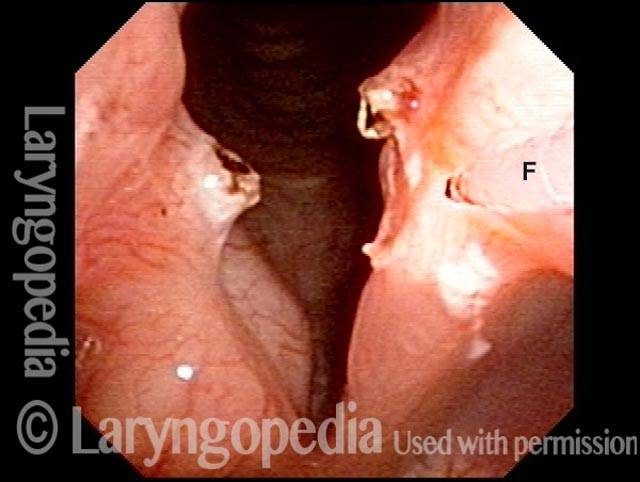
Subito dopo il laser (4 di 5)
Ciò avviene subito dopo la divisione della banda con laser al tullio, utilizzando solo anestesia topica e con il paziente seduto su una sedia.

Un mese dopo l’intervento (5 di 5)
Un mese dopo non si vede più alcun residuo di sinechie e le corde vocali possono allontanarsi di più rispetto alla foto 1.
Medializzazione iniettiva per paresi delle corde vocali
Guarda un esempio di una variante della paresi delle corde vocali e di come limita la voce. Quindi osserva una procedura di medializzazione in cui il gel vocale viene iniettato nella corda vocale colpita da paresi e ascolta come la voce migliora successivamente.
Quick Fixes to Bring Back Damaged Voices
BVI utilizza procedure come iniezioni di gel per aiutare i pazienti a ripristinare le corde vocali ferite...