Vocal Cord Microsurgery (Microlaryngoscopy)
Vocal cord microsurgery (microlaryngoscopy) is an endoscopic procedure focused upon the larynx, performed under general anesthesia. A hollow lighted tube rests on the upper teeth and the base of the tongue and allows the physician to see the vocal cords. An operating microscope is used to brightly illuminate and highly magnify the vocal cords. Then, tiny instruments and/or a laser are used to remove the abnormality from the vocal cord or cords.
Who Needs Microlaryngoscopy?
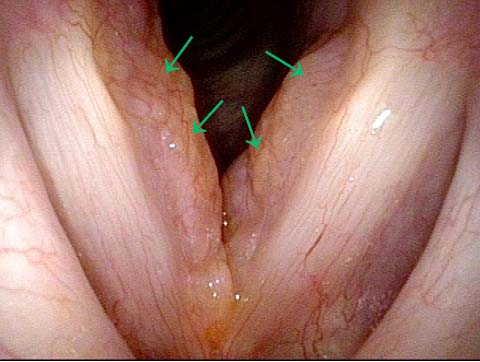
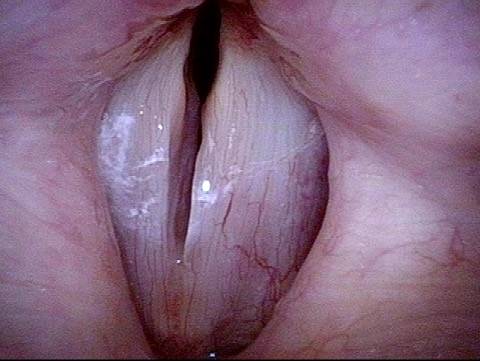
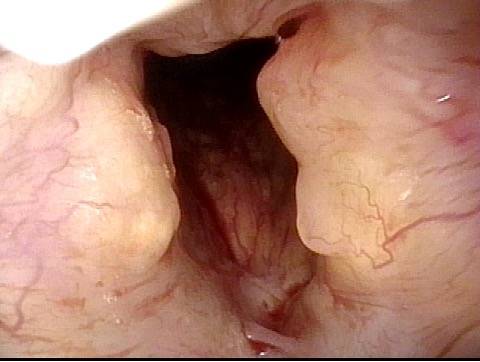
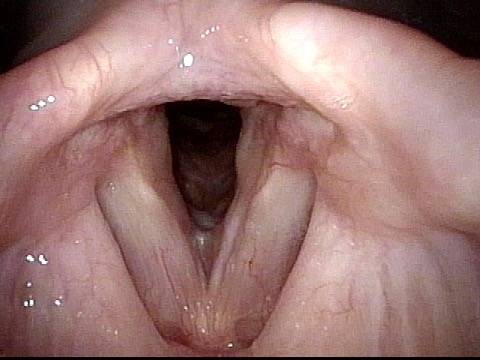
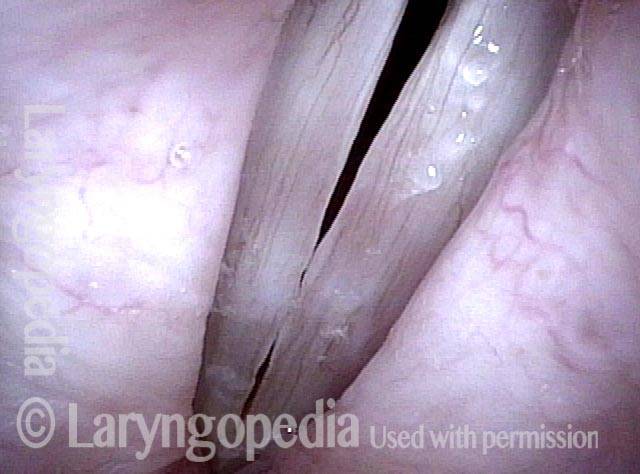
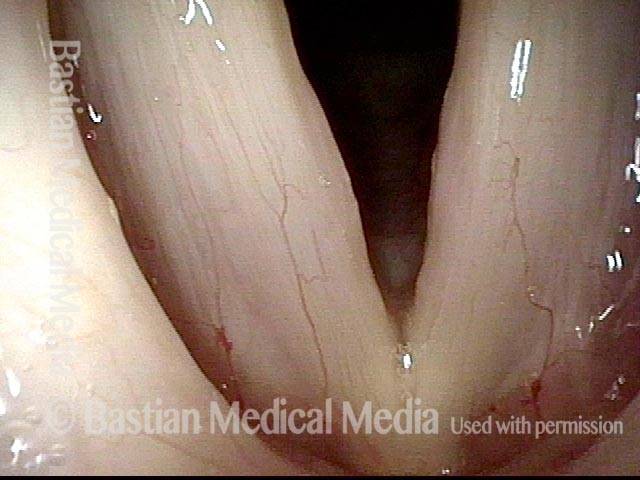
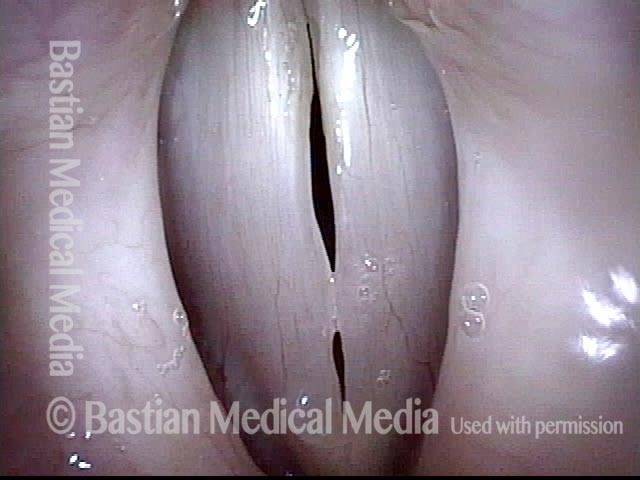
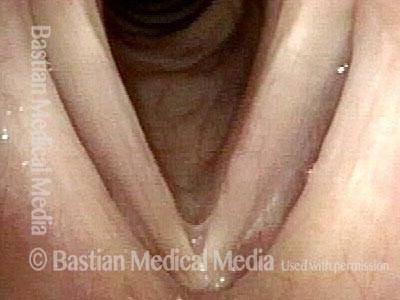
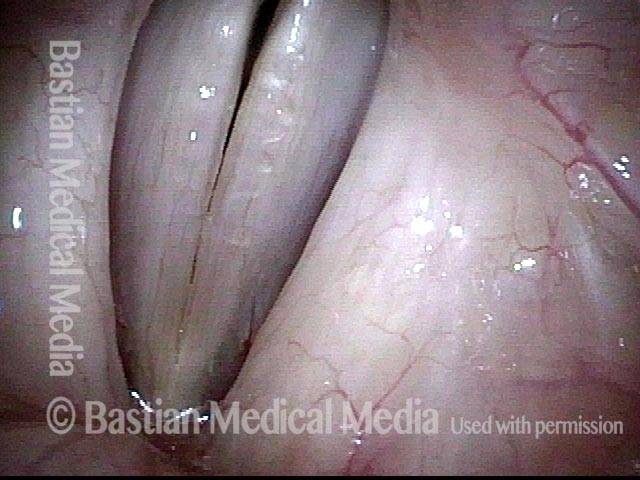
The commonest reason is that there is a visible lesion such as nodules, polyps, capillary ectasia (dilated capillaries), epidermoid or mucus retention cyst, glottic sulcus, papilloma, or a known vocal fold cancer. The point is to remove the lesion to improve the sound or capabilities of the voice.
Of course, if a tumor is involved, voice takes second place to removal of the lesion. Removed tissue is always examined by the pathologist, but for most individuals, the need for biopsy is much less than the need for a better voice.
How Is the Procedure Accomplished?
The procedure, aka Microlaryngoscopy, is typically performed in an outpatient operating room during relatively brief general anesthesia. After you are completely asleep, a hollow, lighted “tube”—called a laryngoscope—is placed on the back of the tongue and against the sidewall of the throat, where it rests during the procedure. A microscope is brought into position, aligned with the laryngoscope, and the vocal folds are highly magnified and brightly illuminated.
Then, the surgeon uses tiny instruments and / or the carbon dioxide laser, to remove or ablate the problem. Both laser and non-laser tools / methodologies are available for every case, but which tools are used depend upon the nature of the problem. There is nothing innately superior about either method; it is the surgeon and not the tools that matter most. Nevertheless, one tends to use instruments for nodules, polyps, cysts, while the laser is more likely to be used for vascular abnormalities or removal of a vocal fold carcinoma.
Time required for the procedure is usually short—10 to 45 minutes of operating time.
Potential Risks
Unless you have significant health issues, risks added together are very small indeed. The three main risks include:
- A truly remote possibility of drug reaction, heart problem, etc., during general anesthesia.
- A very small chance of dental trauma—e.g., chipped, scratched, broken, or dislodged tooth. We have a few instances per year of roughened enamel that doesn’t need a dentist’s attention, but only to be smoothed off in the O.R. Beyond this, about once every 3 years something more significant, such as a broken or dislodged crown or tooth happens.
- We cannot guarantee the precise degree of improvement—whether the result will be “good,” “very good,” or “spectacular.” That depends to large degree on the difficulty of the original problem. And when a known tumor is being removed, we may expect possible worsening of voice quality, as compared to “normal.”
Common Questions about Microlaryngoscopy
What is the chance my voice will be worse after surgery?
The very point of most microlaryngoscopy surgeries is to improve the voice. When we do this kind of surgery in singers—the most discriminating judges of the results of this kind of surgery—both singer/patient and surgeon, not to mention voice teachers, are routinelypleased with the result of surgery. Our expectations do vary a bit, however, with the kind of lesion we are removing.
For example, we expect extremely good results within days with capillary ectasia, nodules, and polyps; good results after cyst or sulcus surgery, though with a much longer and more gradual recovery of voice over months’ time, and so forth. Your surgeon should be able to provide you with an estimate of what kind of voice result is realistic to expect after your surgery.
What about voice use?
Specific advice may vary with the individual. That said, here are the usual voice use restrictions:
Nodules, polyps, capillary ectasia
- No talking for 4 days—usually this means from the day of surgery (Wednesday, for example) to Sunday. During those days, we usually suggest gentle sighing sounds for 10 seconds or so every few hours.
- Talking resumes on Sunday (5th day), but at a restricted amount—you may be a “3” on our 7-point talkativeness scale for one week. If a singer, you may begin vocalizing for 5 minutes twice a day, also beginning Sunday.
- Additional details of postoperative voice use will be explained at your first post-operative visit—typically, you are a “4” for a week; a “5” for a week, and so forth. Vocalizing increases by 5 minutes each practice session, week by week. For singers, we suggest a first (short) voice lesson in the second or third week after surgery.
Cyst, sulcus, papilloma, stenosis, early vocal fold cancer
No voice rest at all, other than one week of what we term “vocal prudence.” This means to talk when you need to, to get the business of life done, but limit “pleasure” talking, and certainly don’t join any street demonstrations!”
When do I see my doctor after surgery?
Typically, we will see you for the first postoperative visit at about a week after surgery (7th day). You will have been talking a couple of days by this time.
If flying home, you may depart the morning after the surgery. It is preferred to see you at some point in the future, but we understand that logistical and cost issues may mean that we never get to see you again! In that case, we do telemedicine follow-ups, and suggest follow-up visits with a laryngologist nearer your home—usually the one who sent you to us in the first place.
What other issues should I expect after surgery?
- You will go home the day of surgery, with rare exception. Of course, you will have to be driven by family member or friend. Most have minimal after-effects from the anesthesia medication. Nausea, for example, has become relatively uncommon.
- You may choose to take medication for a sore throat consisting of either Tylenol or Tylenol with Codeine, barring allergy or sensitivity.
- You may eat whatever your appetite and throat discomfort allow. We do suggest that your first post-operative food be relatively bland, and a small amount, to be sure your stomach is “settled.” Occasionally, salty or acidic food / liquids will burn the sore area caused by pressure from the laryngoscope. Most commonly, that pain will be on the left side.
- Occasionally the teeth feel a little sore and loose, especially your upper central incisors.
What if I forget and talk, or talk in my sleep?
No harm done, just don’t talk knowingly during the initial post-surgery days.
The potential for harm to my teeth really bothers me.
Actually, though dental injury happens so infrequently, this possibility bothers us too! That’s why we use not only a tooth guard, but also all the care and gentleness we can muster while doing your surgery. That said, please keep in mind that you must NOT do this surgery if you cannot personally accept the very small chance of a dental problem. The only way for you to avoid this small risk, and its potential expense to you, is to not have the surgery.
What if my teeth do feel loose?
We suggest that you refrain from wiggling them, or from biting into tough foods until they tighten back up on their own. Most often this takes a week or so.
Suppose I develop a cough after surgery. Will that ruin my voice result?
No—so far the worst outcome I’ve seen in the few times this has occurred is that the person is hoarse a little longer after surgery—it takes somewhat longer for the very early “surgical laryngitis” to resolve. If you do experience a lot of coughing, over-the-counter Robitussin DM suffices for most people. If that is not effective, you can call your physician for a stronger prescription.