The palate is a structure which serves as both the roof of the mouth and the floor of the nasal cavity and nasopharynx. It has two parts: the hard palate and the soft palate. The hard palate, which is the anterior two-thirds of the palate, begins just behind the upper central teeth and is made up of bone. The soft palate, which is the posterior one-third of the palate, is made up of muscle; the soft palate is therefore movable, and it elevates to help with swallowing and speech.
See also: palate paralysis; palate deviation
High Vagus Nerve Injury
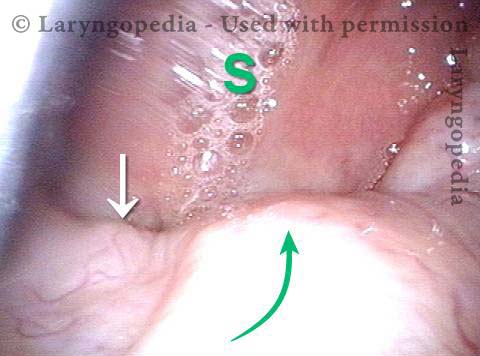
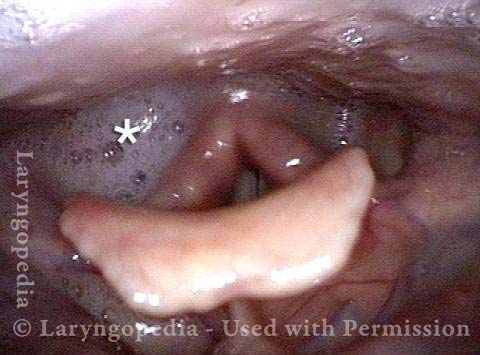
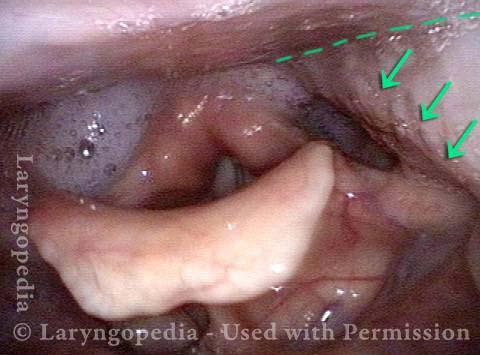
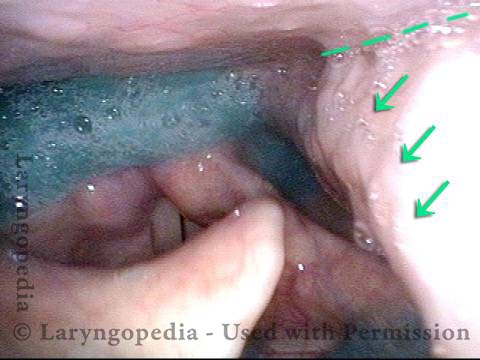
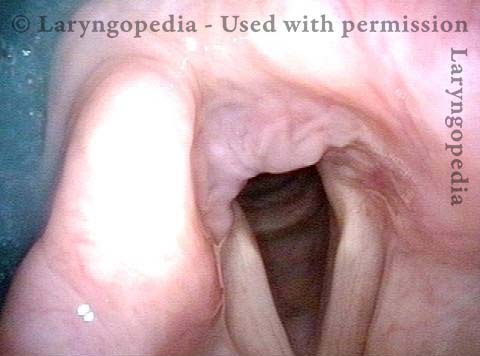
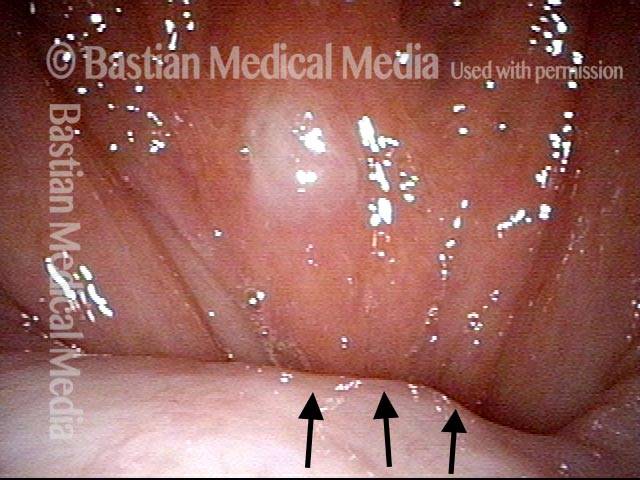
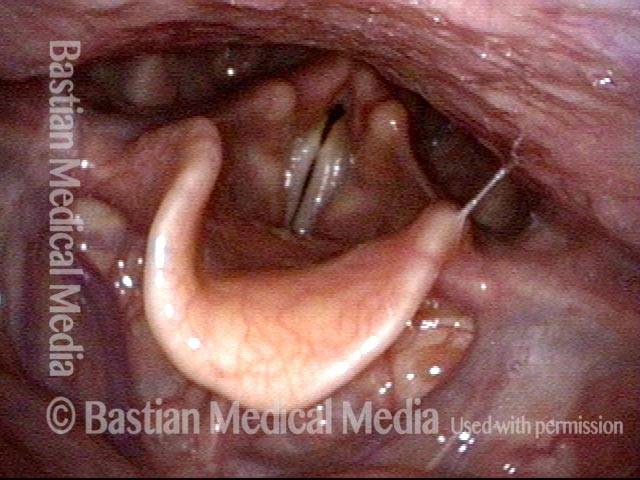
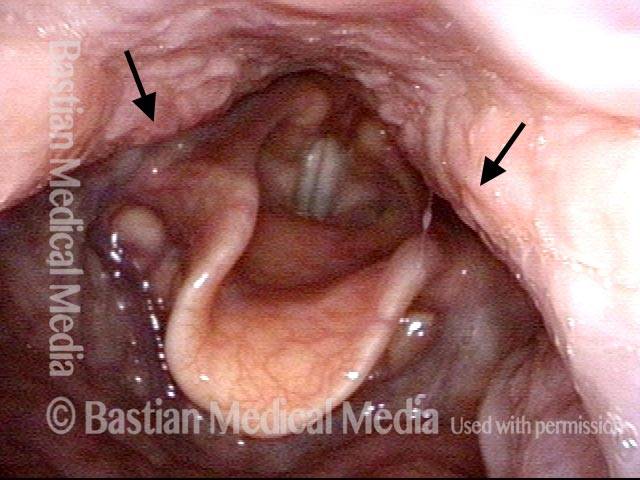
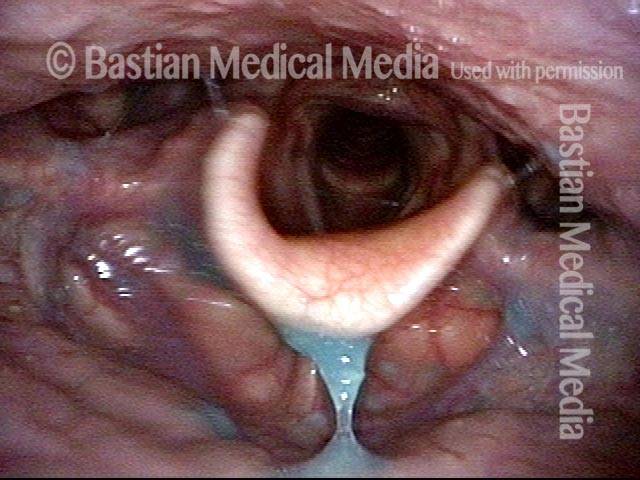
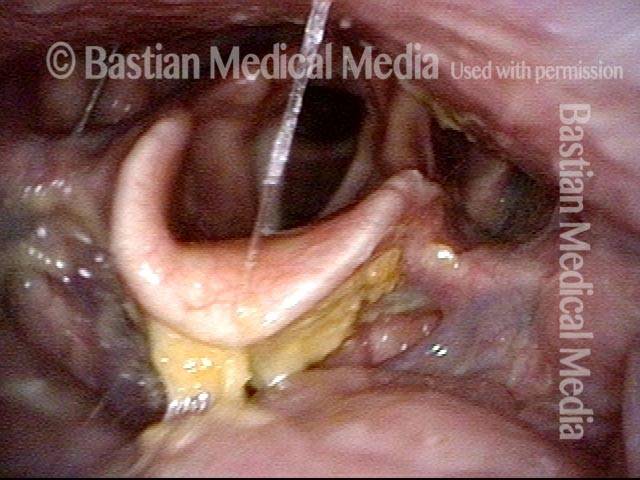
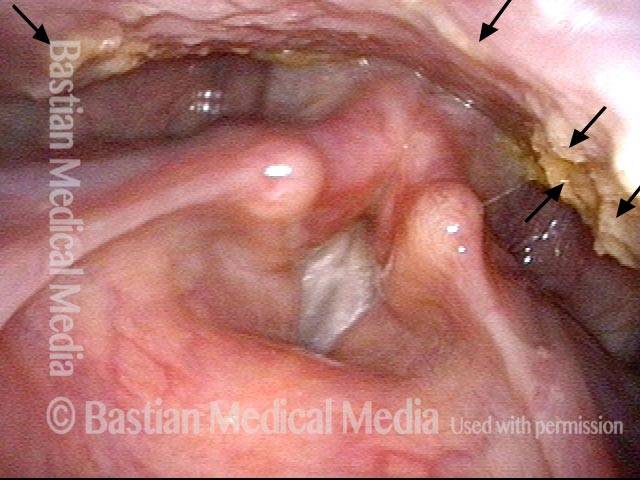
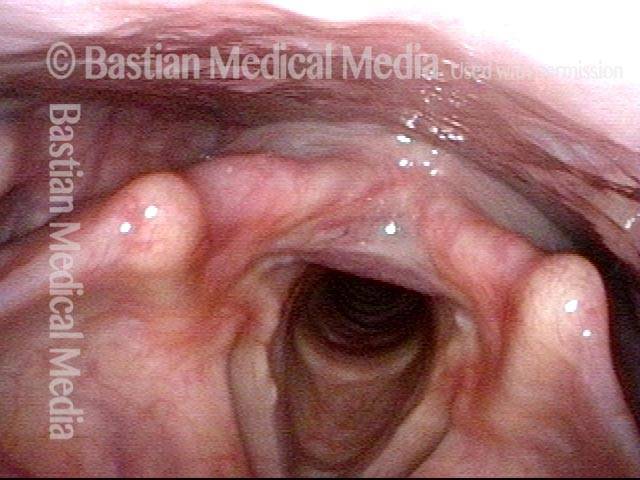
The vagus (10th cranial) nerve originates from the medulla (part of the brainstem), exits from the base of the skull through the jugular foramen, and among other things, supplies branches to the musculature of palate, pharynx, and larynx. Location of vagus nerve injury is sometimes evident by palate and pharynx findings. But these findings are sometimes overlooked as in this case, especially if palate and pharynx are weak but not completely paralyzed.
Case study: This 50-something woman developed a weak voice and moderate difficulty swallowing upon awakening 5 months prior to this visit. Fortunately, her symptoms of weak voice and difficulty swallowing were not devastating, and are improving. But up to this examination, there has been no diagnosis. This examination reveals a “lesion” of her right vagus nerve and it has to be at the base of the skull because palate, pharynx, and larynx muscles are all weak. Voice is functional but lacks the ability to project and has a “soft-edged” quality. A sophisticated listener can also hear mild hypernasality. The examination below prompts a scan with special attention to base of skull to be sure there is no mass lesion there.