Stridor
Stridor is a harsh, wheezy, or rough respiratory sound most often heard on inspiration to indicate laryngeal, subglottic, or tracheal partial obstruction or stenosis. Compare with involuntary inspiratory phonation.
Tracheal Stenosis, before and after Tracheal Resection and Primary Reanastomosis
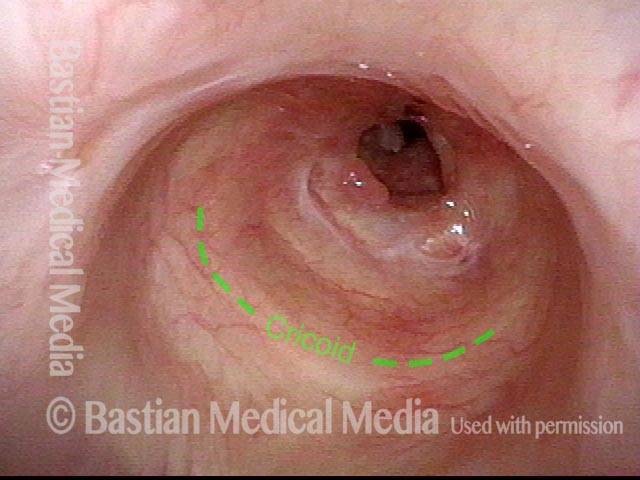
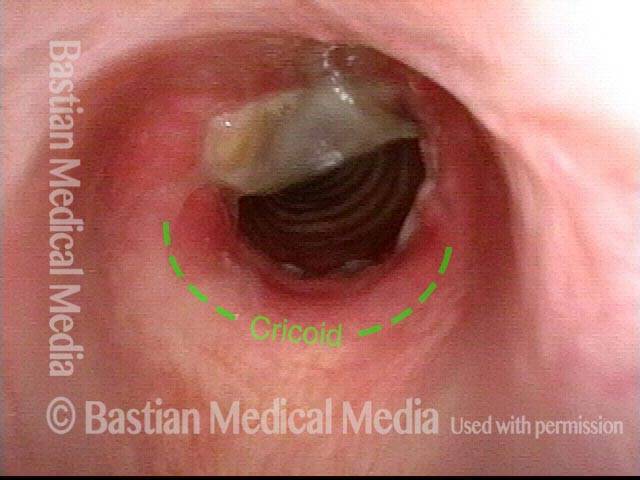
Tracheal stenosis (1 of 8)
This view from the level of the vocal cords shows high-grade tracheal stenosis, involving rings two, three, and four; the airway here is an estimated 30% of its normal diameter. For reference, a dotted line marks the level of the cricoid cartilage.
Tracheal stenosis (1 of 8)
This view from the level of the vocal cords shows high-grade tracheal stenosis, involving rings two, three, and four; the airway here is an estimated 30% of its normal diameter. For reference, a dotted line marks the level of the cricoid cartilage.
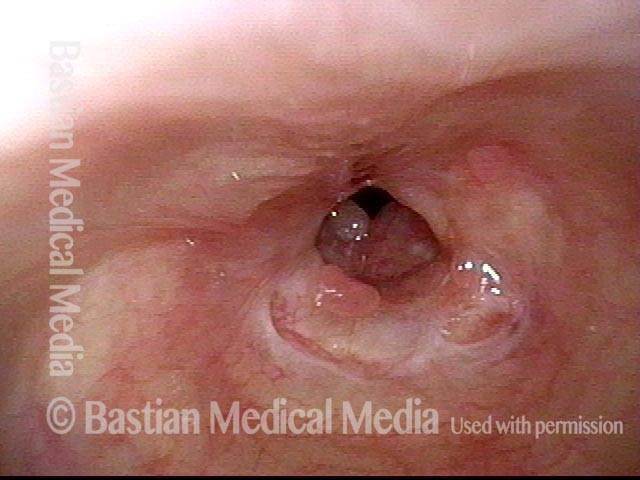
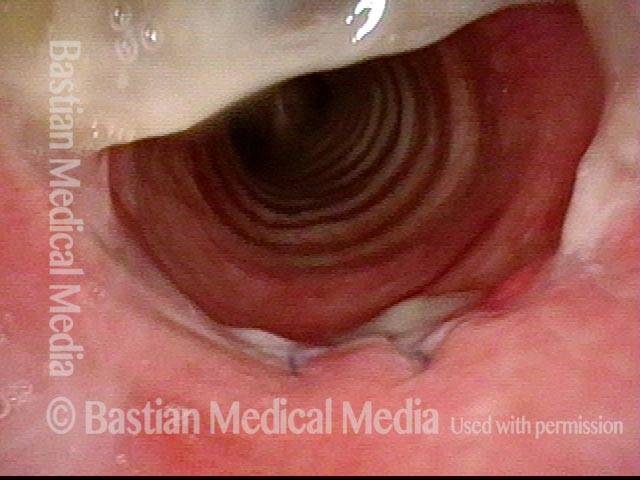
Tracheal stenosis (2 of 8)
Slightly closer view. This patient is very short of breath with minimal activity and, even at rest, has audible stridor. Elsewhere, across a span of several prior weeks, she had undergone three dilation procedures with only minimal, transient benefit.
Tracheal stenosis (2 of 8)
Slightly closer view. This patient is very short of breath with minimal activity and, even at rest, has audible stridor. Elsewhere, across a span of several prior weeks, she had undergone three dilation procedures with only minimal, transient benefit.
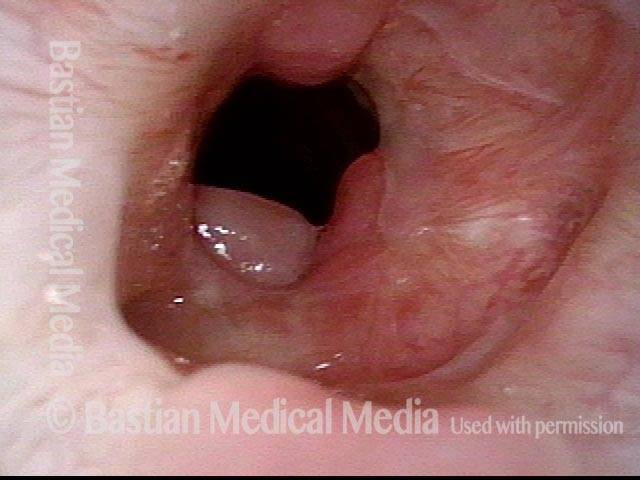
Close up view (3 of 8)
Close-up view shows scarring, collapse of tracheal walls, and some granulation tissue.
Close up view (3 of 8)
Close-up view shows scarring, collapse of tracheal walls, and some granulation tissue.
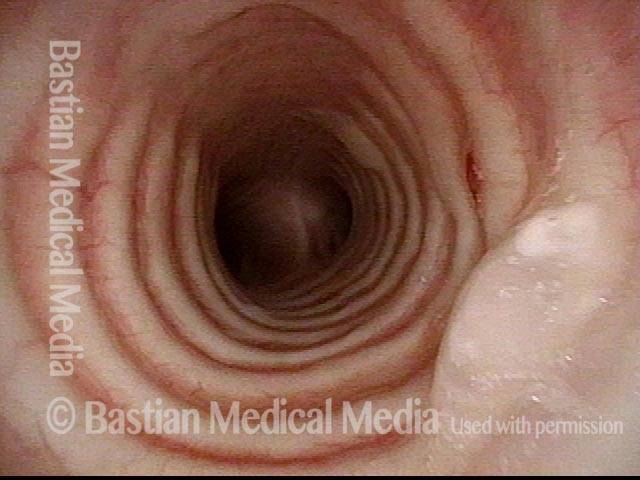
Just below the tracheal stenosis (4 of 8)
The trachea just beyond the stenosis is normal.
Just below the tracheal stenosis (4 of 8)
The trachea just beyond the stenosis is normal.
Tracheal stenosis, 5 days after surgery (5 of 8)
Five days after tracheal resection and primary reanastomosis. Compare with photo 1. Note that the airway’s diameter has at least tripled (part of the opening is obscured by tenacious mucus). The patient’s shortness of breath is now gone, as is the stridor.
Tracheal stenosis, 5 days after surgery (5 of 8)
Five days after tracheal resection and primary reanastomosis. Compare with photo 1. Note that the airway’s diameter has at least tripled (part of the opening is obscured by tenacious mucus). The patient’s shortness of breath is now gone, as is the stridor.
Tracheal stenosis, 5 days after surgery (6 of 8)
Close-up of the line of anastomosis, with a couple of sutures visible. Compare with photo 3. Again, tenacious mucus in the upper part of the photo is obscuring part of the view.
Tracheal stenosis, 5 days after surgery (6 of 8)
Close-up of the line of anastomosis, with a couple of sutures visible. Compare with photo 3. Again, tenacious mucus in the upper part of the photo is obscuring part of the view.
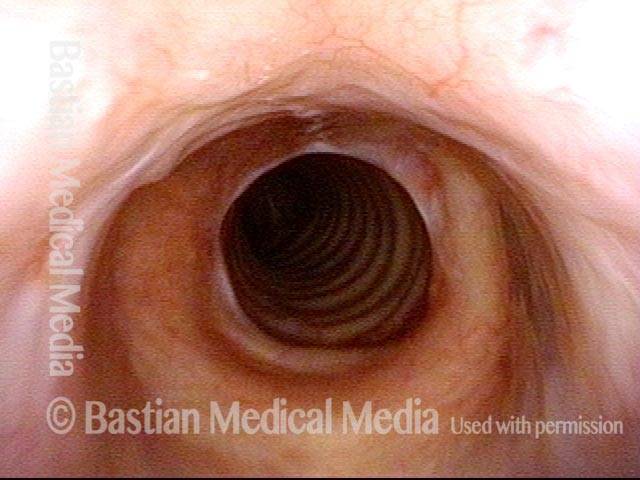
Tracheal stenosis, 2 months after surgery (7 of 8)
Another eight weeks later. The airway is wide-open and has also now healed since the surgery. Compare this view with photo 1 (pre-surgery) and photo 5 (early follow-up).
Tracheal stenosis, 2 months after surgery (7 of 8)
Another eight weeks later. The airway is wide-open and has also now healed since the surgery. Compare this view with photo 1 (pre-surgery) and photo 5 (early follow-up).
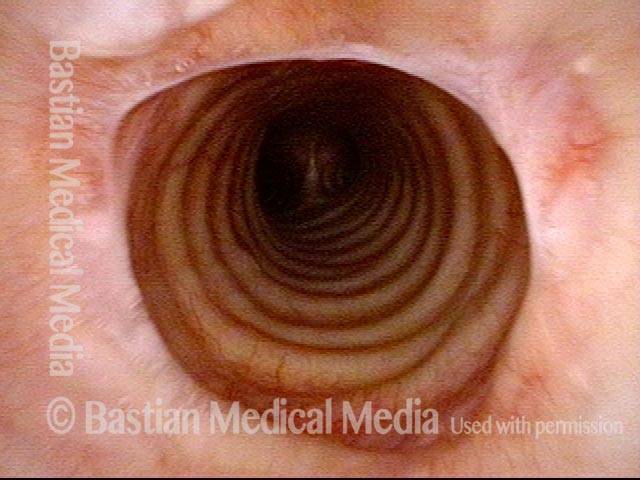
Tracheal stenosis, 2 months after surgery (8 of 8)
Compare this view with photo 2.
Tracheal stenosis, 2 months after surgery (8 of 8)
Compare this view with photo 2.
Local Rather than Topical Anesthesia can Permit Fairly Major Tracheal Surgery
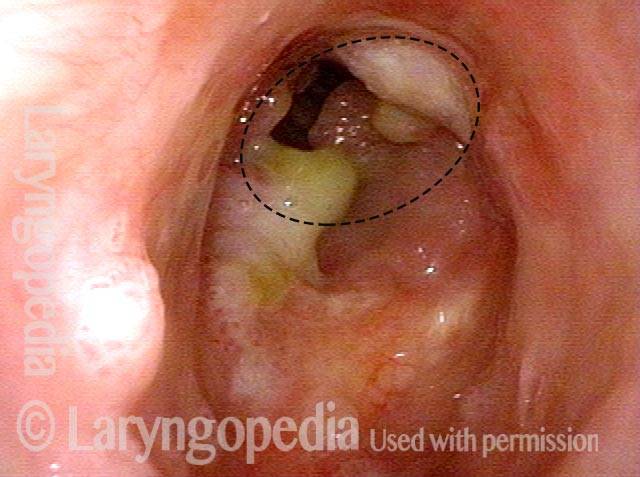
Obstructive papillomas (1 of 4)
This middle aged man has had lifelong RRP due to HPV 11. Primary focus of his recurrences for many years has been the trachea. Prior operative removals under general anesthesia have been challenging and recent work has used the thulium laser in an office setting. The papillomas seen here explain his mild pre-procedure stridor. His tracheal lumen should be approximately the size of the dotted circle.
Obstructive papillomas (1 of 4)
This middle aged man has had lifelong RRP due to HPV 11. Primary focus of his recurrences for many years has been the trachea. Prior operative removals under general anesthesia have been challenging and recent work has used the thulium laser in an office setting. The papillomas seen here explain his mild pre-procedure stridor. His tracheal lumen should be approximately the size of the dotted circle.
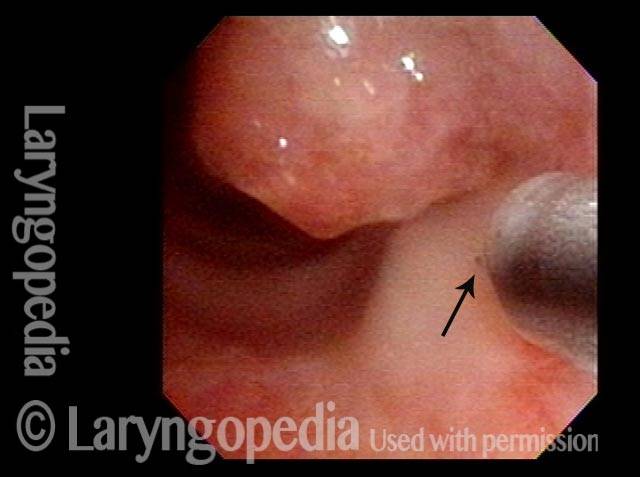
Local injections (2 of 4)
A needle catheter passed through the channel of the scope is embedded at arrow, and is injecting 1% lidocaine with epinephrine (see blanched area). Numerous areas are similarly injected.
Local injections (2 of 4)
A needle catheter passed through the channel of the scope is embedded at arrow, and is injecting 1% lidocaine with epinephrine (see blanched area). Numerous areas are similarly injected.
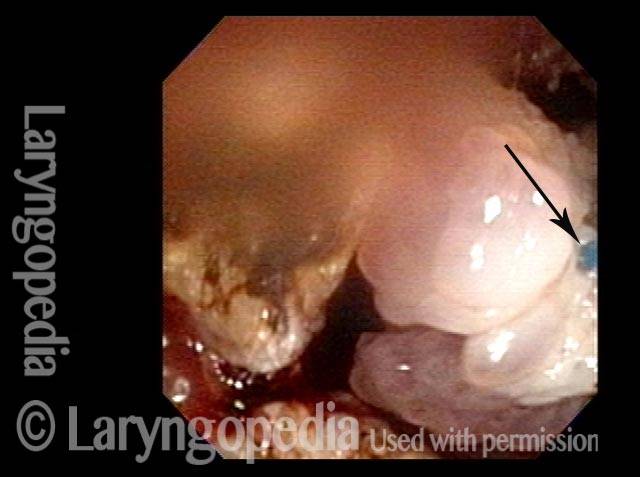
Removal of papilloma (3 of 4)
Here a large chunk of papilloma (stuck to the laser fiber at arrow) is being pulled away.
Removal of papilloma (3 of 4)
Here a large chunk of papilloma (stuck to the laser fiber at arrow) is being pulled away.
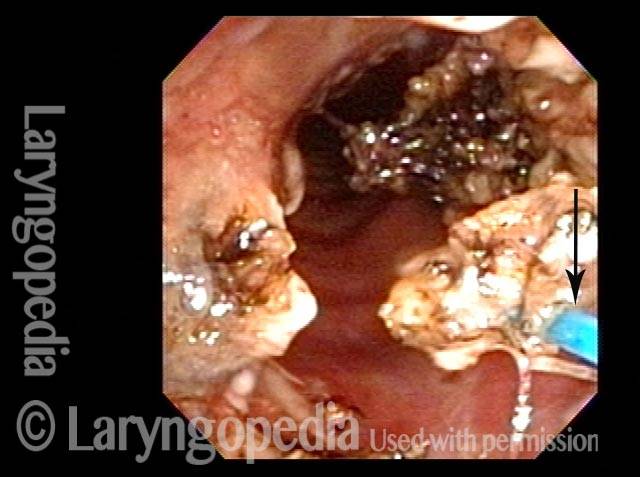
Improved breathing with papilloma removal (4 of 4)
An additional chunk is being detached. The patient’s breathing at the conclusion of this procedure is much improved. The tracheal lumen will be even larger when a lot of remaining coagulated papillomas slough away.
Improved breathing with papilloma removal (4 of 4)
An additional chunk is being detached. The patient’s breathing at the conclusion of this procedure is much improved. The tracheal lumen will be even larger when a lot of remaining coagulated papillomas slough away.
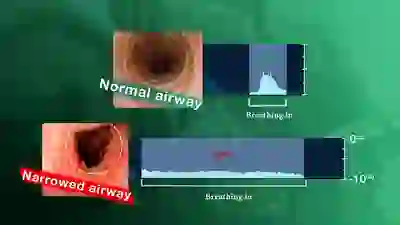
Using Your EARS to Understand Airway Narrowing
A narrowing anywhere in the breathing “pipe” that leads to the lungs causes shortness of breath, typically with harsh inspiratory noise on exertion. Such a narrowing can follow injury, intubation, cancer treatment, auto-immune disorders, etc.
It is possible to gain an immediate understanding of the magnitude of the airway narrowing within minutes by using a simple test “graded” with one’s ears. The severity of the problem can be understood before any examination or X-ray evaluation.
Tagged Airway disorders, Disorders