Selective Laryngeal Adductor Denervation-Reinnervation (SLAD-R)
Selective Laryngeal Adductor Denervation-Reinnervation (SLAD-R) is a newer surgical treatment for adductory spasmodic dysphonia, introduced by Dr. Gerald Berke of UCLA[1] in the late 1990s. During the procedure, the anterior branch of the recurrent laryngeal nerve, which supplies the thyroarytenoid (TA) and lateral cricoarytenoid (LCA) muscles—both essential for voice production—is severed. This eliminates the strained, squeezed quality of the voice, as well as the characteristic “catching” or “cutting out,” of speech. However, without additional intervention, the voice would remain permanently weak, or dystonic nerve impulses could reestablish unwanted connections.
To avoid this, SLAD-R includes a simultaneous reinnervation process. A branch of the ansa cervicalis nerve, which typically serves less critical neck muscles, is harvested and connected to the severed nerve. This helps restore function while preventing unwanted nerve regeneration. However, the reconnection process takes time, leaving patients with a breathy, whispery voice for three or more months before some muscle tone and vocal volume return.
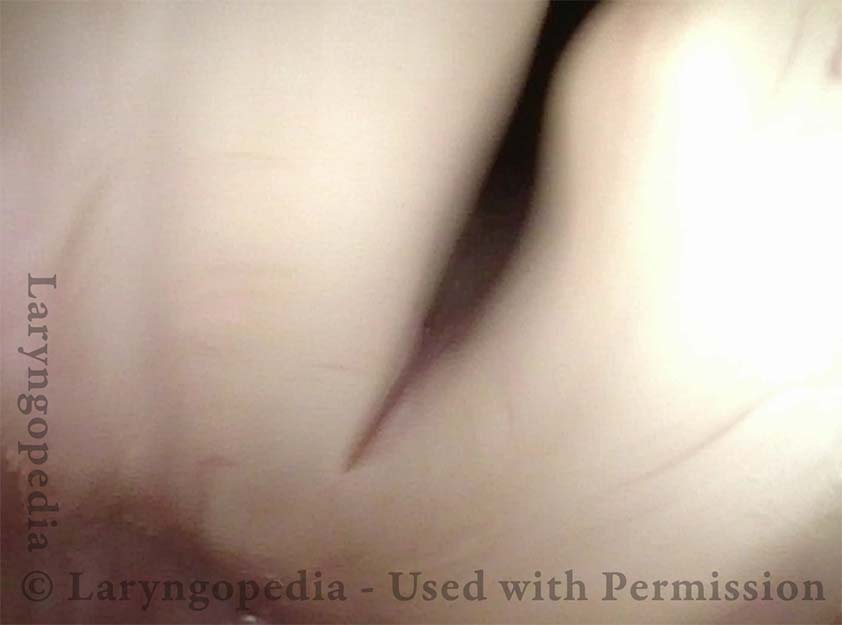
While many patients experience long-term improvement, others may redevelop spasms and require additional treatments, such as Botox injections or vocal cord muscle debulking. The effectiveness of SLAD-R varies, and outcomes are difficult to predict for any individual. It would be helpful to have an online source of voice recordings of many patients at various times: before SLAD-R surgery, and also at 3 months, 6 months, 1 year, and 2 years after surgery.
Differential Re-Innervation after SLAD-R Surgery
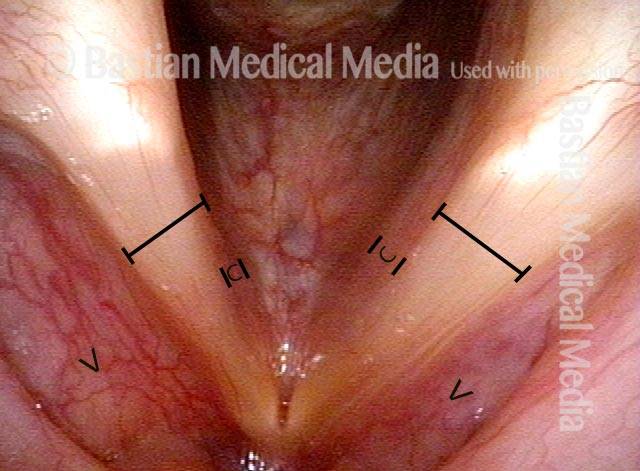
Six years post SLAD-R (1 of 4)
Six years post SLAD-R (1 of 4)
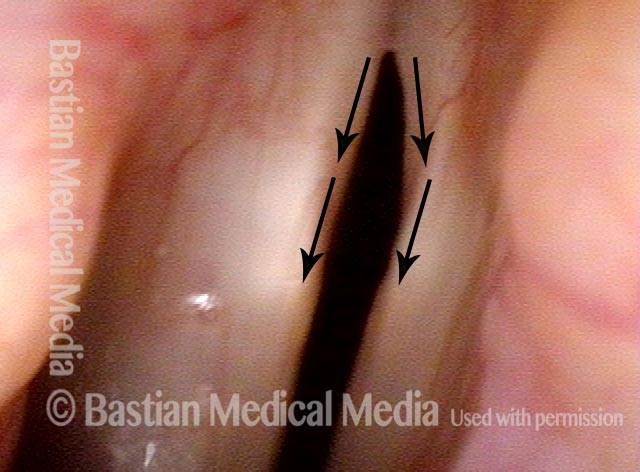
TA + LCA muscles (2 of 4)
TA + LCA muscles (2 of 4)
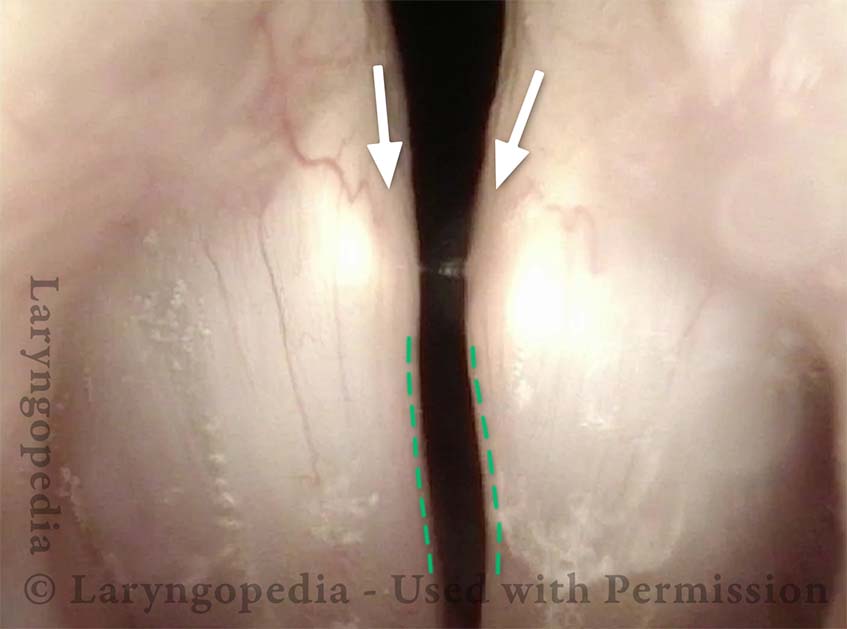
Greater amplitude of right cord (3 of 4)
Greater amplitude of right cord (3 of 4)
Patient has returned to Botox (4 of 4)
Patient has returned to Botox (4 of 4)
SLAD-R Findings in Spasmodic Dysphonia
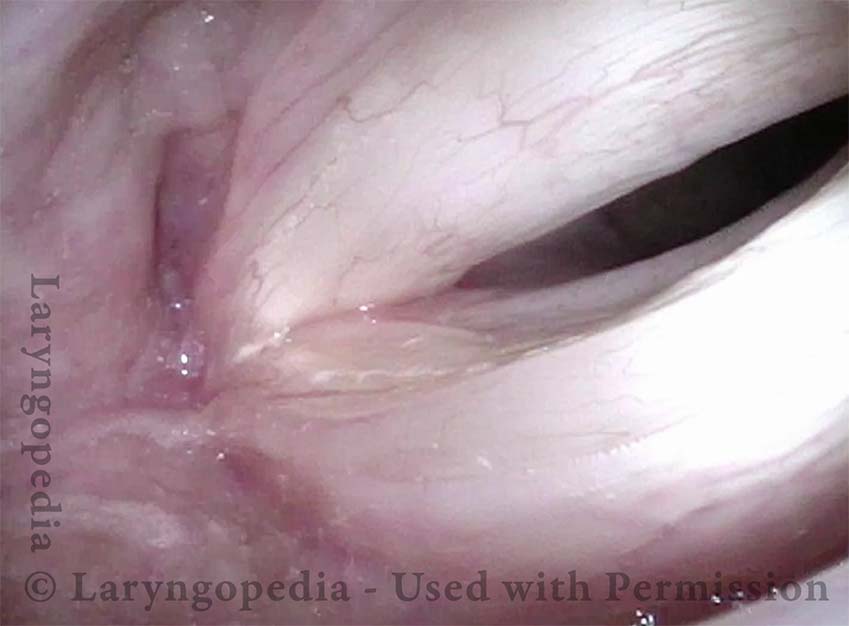
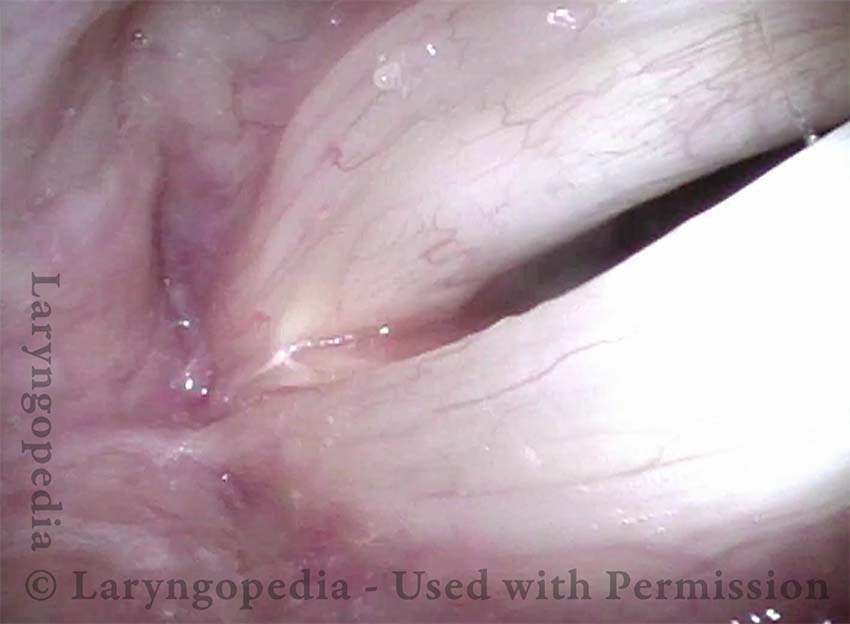
This man has had longstanding laryngeal dystonia causing adductory spasmodic dysphonia. More than a year before these photos, he underwent SLAD-R on the left side (right of photo). The left cord moves normally, and one can see full recovery of the LCA (lateral cricoarytenoid) muscle, but the TA (thyroarytenoid) muscle is atrophic and flaccid.
Angle of Abduction (1 of 5)
Angle of Abduction (1 of 5)
Concave Margin (2 of 5)
Concave Margin (2 of 5)
Lateral buckling (3 of 5)
Lateral buckling (3 of 5)
Mild bowing (4 of 5)
Mild bowing (4 of 5)
Greater amplitude (5 of 5)
Greater amplitude (5 of 5)
Share this article
One Man’s Experience Over Time with SLAD-R
SLAD-R is a surgical alternative to ongoing “botox” injections for treatment of adductory spasmodic dysphonia. The surgery involves intentionally cutting the nerves that close the vocal cords for voice and reconnecting a different nearby nerve supply (reinnervating the nerves).
This surgery requires the patient’s willingness to endure an extremely breathy voice for many months after the procedure, while awaiting reinnervation.