Granulomatosis with Polyangiitis (GPA, Wegener’s Granulomatosis)
Granulomatosis with polyangiitis (GPA) is a rare inflammatory disease of small arteries and veins (vasculitis) that classically involves vessels supplying the tissues of the lungs, nasal passages (sinuses), and kidneys. Up until recent decades, the disease has been re-named from Wegener’s Granulomatosis (WG), because of the Nazi association of Dr. Friedrich Wegener.
GPA is an autoimmune disorder. Autoimmunity means that the body’s immune system begins to recognize as “foreign” one or more of its own tissues.
The immune system must of course recognize when a truly foreign object (e.g. splinter in the finger) or organism (virus, bacterium, or parasite) invades the body so that it can respond and fight off the foreign element. Unfortunately, when the immune system is mobilized against one of the body’s own tissues, it can be devastating.
Examples of damage to one’s own body include rheumatoid arthritis (joints), rheumatic heart disease (heart valves), and inflammatory bowel disease (the GI tract). In the case of WG/GPA, there are four common sites of attack:
- Nose and sinus;
- Subglottis and trachea;
- Lungs;
- Kidney
Is GPA Terminal?
Up until only decades ago, WG / GPA was uniformly fatal. That is no longer the case, though persons with this disease can be very ill at diagnosis, and life expectancy can be reduced.
GPA of the Subglottis and Treachea
We have often referred to our large caseload of inflammatory idiopathic subglottic stenosis as having a limited expression or forme fruste of the disease. And they might be described formally as having an undefined autoimmune disorder, aka undifferentiated connective tissue disorder (UCTD), because the classical criteria (clinical manifestation and laboratory testing) are not fully met. But with patients who have both WG / GPA and those with what we call Forme Fruste WG / GPA have strikingly similar inflammatory subglottic stenosis.
Thus far, no patient of an estimated 150-patient caseload has manifested anything more than laryngeal / tracheal disease and in some, sino-nasal manifestations. The latter can be crusting, bleeding, and “autoimmune” vascular markings on the septum, and a few have slowly-progressive saddle nose deformity.
Is GPA Hereditary?
To date, none of the patients in a large GPA caseload have yet described another family member with the disorder.
Subglottic Stenosis, Due to Wegener’s Granulomatosis
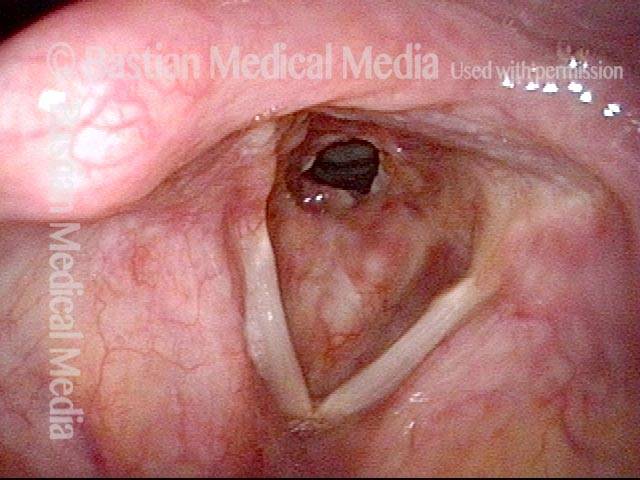
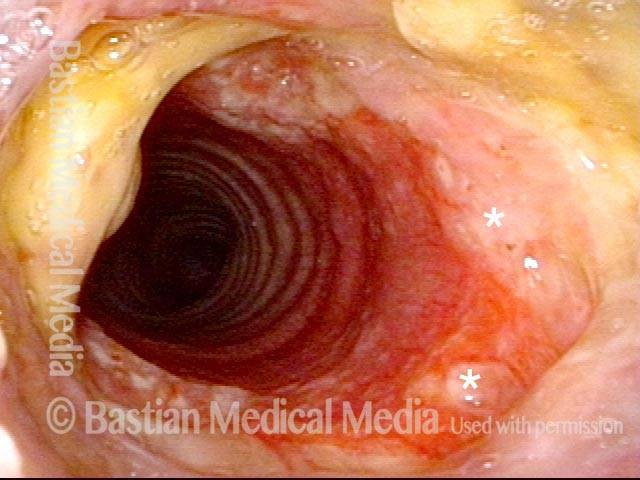
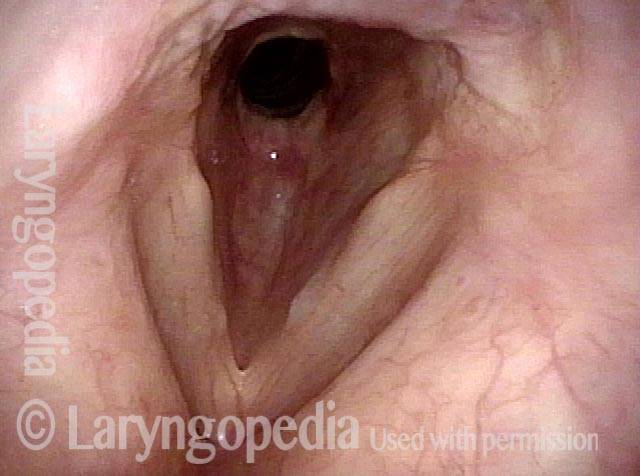
Subglottic stenosis, due to Wegener’s (1 of 2)
Subglottic stenosis, due to Wegener’s (1 of 2)
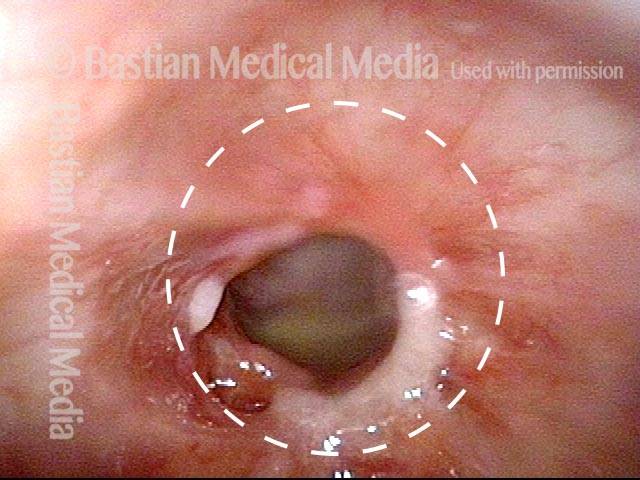
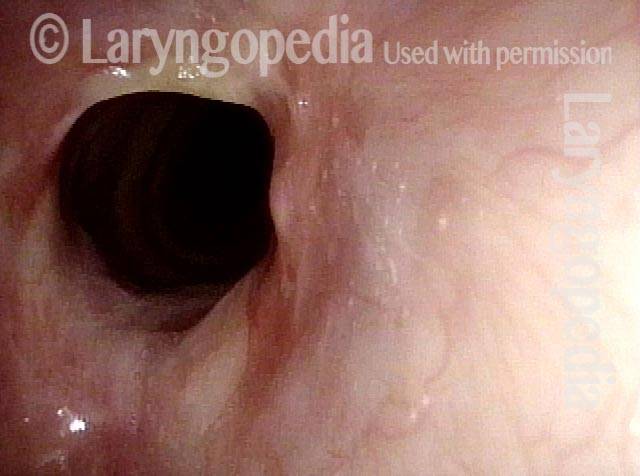
Subglottic stenosis, due to Wegener’s (2 of 2)
Subglottic stenosis, due to Wegener’s (2 of 2)
Airway Stenosis Caused By Wegener’s Granulomatosis, Before and After Dilations
Airway stenosis (1 of 5)
Airway stenosis (1 of 5)
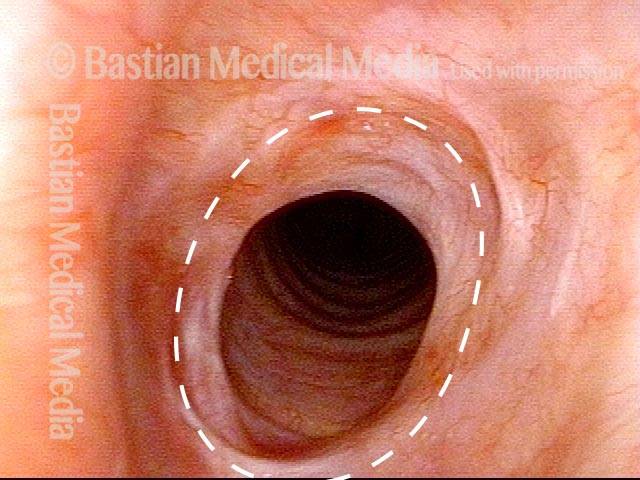
Airway stenosis, after dilation (2 of 5)
Airway stenosis, after dilation (2 of 5)
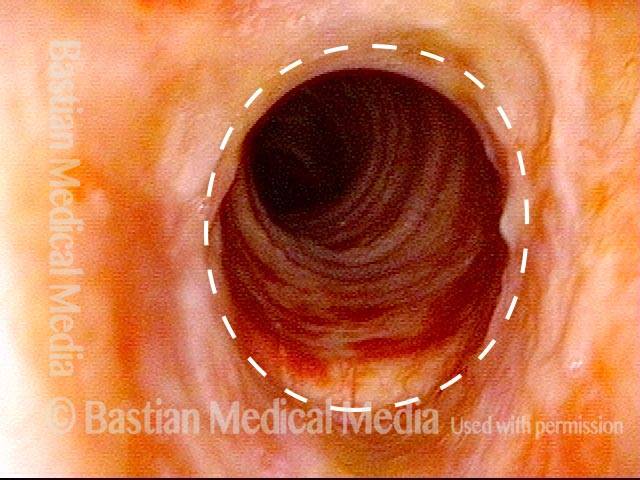
Airway stenosis, after dilation (3 of 5)
Airway stenosis, after dilation (3 of 5)
Airway stenosis, before another dilation (4 of 5)
Airway stenosis, before another dilation (4 of 5)
Airway stenosis, after another dilation (5 of 5)
Airway stenosis, after another dilation (5 of 5)
Vascular Manifestations of Wegener’s-related Septum Changes, and Subglottic Stenosis Indistinguishable from Forme Fruste Wegener’s
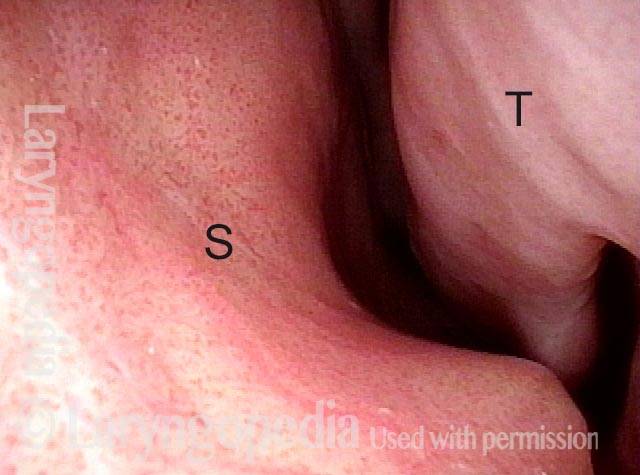
View inside left nostril (1 of 4)
View inside left nostril (1 of 4)
Narrow band light (2 of 4)
Narrow band light (2 of 4)
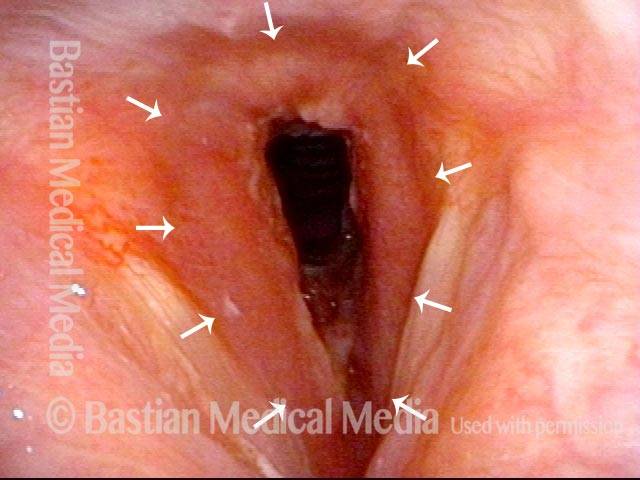
Distant view (3 of 4)
Distant view (3 of 4)
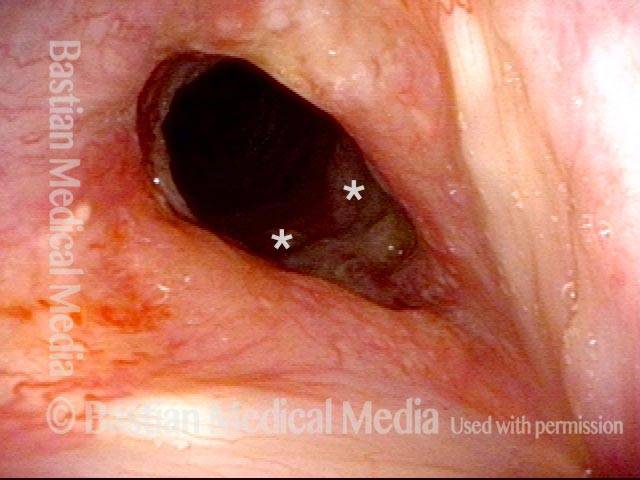
Closer view (4 of 4)
Closer view (4 of 4)

Wegener’s Granulomatosis: Forme Fruste (incomplete expression)
Wegener’s granulomatosis is a rare autoimmune disorder in which blood vessels become inflamed. The inflammation causes swelling and scarring. Three typical organs attacked are sinus/nasal cavities, lungs, and kidneys.
In the forme fruste variant, it is mostly an inflammatory stenosis (narrowing) of the area below the vocal folds, and also the trachea. A person becomes short of breath and begins to make harsh breathing sounds due to the narrowed passageway.
This is an example of one means of management: dilation of the narrowed area during a very brief general anesthetic in an outpatient operating room.