An Open Letter to Gastroenterologists about R-CPD
Introduction
Many patients with inability to belch and severe associated gastrointestinal distress struggle for years to find the recently established diagnosis of retrograde cricopharyngeus dysfunction (R-CPD). This disorder has received a lot of exposure, including in peer-reviewed journals, yet even when they bring peer-reviewed articles to their doctors, many say they are not taken seriously.
As the person who first described R-CPD and codified details of diagnosis and treatment, I was approached by a worried parent requesting a letter that could be given to doctors caring for his child, who had been treated aggressively for other diagnoses without benefit. This parent was sure the child matched the distinct syndrome of R-CPD.
I set out to write something brief. It turned out to be much longer than I thought. It became so long because I found myself striving, perhaps to a fault, with not only lack of awareness of R-CPD on the part of well-intentioned doctors, but also from a subset of doctors, a huge composite cloud of possibly well-intentioned scepticism and sometimes worse: gaslighting, and lack of openness my patients have described.
Over and over, they have told me of their endless doctor visits and tests which led nowhere. And then, of the relief they felt when we at Bastian Voice Institute finally validated their experience (and solved their problem). In fact, here is a response I received just the day before finalizing this letter (with my emphasis added), from a 27-year-old woman treated a couple of years ago.
“This procedure has been truly life changing for me. I feel so much more comfortable and have so much control over my burping now. I also believe this has fixed a lifelong string of crippling episodes of abdominal pain that have landed me in the hospital multiple times and even led to the removal of my gallbladder (which was not the problem).”
It seems to be primarily Gastroenterologists who have taken a reputational hit in the R-CPD community. I have encountered much greater openness in the laryngology community. And so, in this letter I am channelling the enormous frustration of my patients. And as I wrote the letter for one individual, it occurred to me that lightly modified, it might serve as an open letter to physicians particularly in the GI community, since they are most likely to encounter unfortunate patients with R-CPD.
My Medical Background
I am an ear nose and throat surgeon who has practiced Laryngology (voice, swallowing, upper airway, sensory neuropathic cough, and no-burp disorders) exclusively for 37 years.
I initially had a 20-year academic career reaching the rank of Professor of Otolaryngology at Loyola University of Chicago. In 2003, I left academic medicine to establish Bastian Voice Institute, a tertiary care, now 4-clinician group in suburban Chicagoland. Our work with R-CPD has drawn patients from all 50 U.S States and nearly 30 countries across 6 continents.
On a variety of laryngology subjects, I have written book chapters, and many peer-reviewed articles. Five of the latter pertain to R-CPD. I have also been an invited speaker (keynote or guest faculty) in The United States, Canada, Mexico, Ireland, Australia, Belgium, France, Turkey, and via Zoom in the countries mentioned above. My presentations on R-CPD have so far been in the U.S., India, Philippines, and Brazil.
I have personally treated approximately 970 patients, who have come, so far, from all 50 states, and 26 countries. Patients during the week of this writing came to our suburban Chicago location from Nevada, New York, North Carolina, Washington State, and Texas. The number for all BVI physicians together is nearly 1,700 patients.
My driving ambition is to save patients from needless testing and delay in obtaining both a clear diagnosis of R-CPD and dramatic relief from the daily misery it causes.
Executive Summary
- R-CPD’s “birthplace” as a codified syndrome with an effective treatment is Bastian Voice Institute (BVI) in suburban Chicago, with the first patient “cured” in 2015. The experience with the first 51 patients was published in 2019 (See link in the sidebar). Within just a few years, the understanding of R-CPD has been transmitted to many places around the globe. I have had personal conversations with many physicians nationally and internationally. My early patients’ experiences and my several publications have also been spread/amplified in chatrooms like Reddit and Facebook.
Journalists in the popular press have also written feature articles on the disorder. In addition to our very large caseload at BVI, large caseloads have also accumulated in Manchester and London, England, New York, Boston, Philadelphia, Baltimore, Seattle, Irvine, California, Roselaire, Belgium, Hamburg, Germany, Manila, Philippines, Australia, Vancouver and Toronto, Canada, and many other places.R-CPD is devastating
Patients with the severest cases are living a nightmare. In most patients it causes;- Inability to burp or burping insufficiency;
- Chest/throat gurgling;
- Abdominal bloating (sometimes with dramatic abdominal distention);
- Severe, even extreme, flatulence
Common but less universal symptoms include;
- nausea after eating;
- hiccups (often very painful);
- chest pain;
- mechanical shortness of breath;
- acid reflux;
- episodic hypersalivation;
- inability to vomit when they need to;
- and constipation.

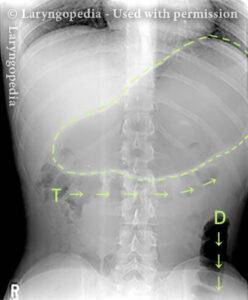
Late-day abdominal distension caused by inability to burp. The discomfort of R-CPD may cause hypersalivation and extra reflexive swallowing, which only adds to the air in his GI tract. He is athletic; the distension represents air in stomach and intestines that could not be burped—not excess weight. Some patients (only those who can vomit) are able to gag themselves and air-vomit. This is like a massive burp but is so loud, they say, as to “shake the walls.” One described it as “letting the devil out.” In another subset of patients, when buildup of air reaches a certain point, they may feel overwhelming “throat nausea” and vomit involuntarily and violently.
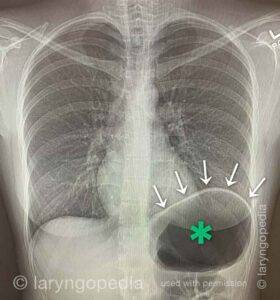
A small subset of unfortunate patients experience abdominal crisis (massive abdominal distention with organ distortion /inability to pass stool/gas) that mimics bowel obstruction. When highly symptomatic as just described, a few also have autonomic symptoms like rapid heartbeat and flushing, or pallor.Remarkably, the common explanation tying all these symptoms together is the inability to burp, or to burp enough, and overstretching of esophagus, stomach, and intestines after massive reflexive or instinctive air-swallowing.
- When patients see physicians who are unfamiliar with R-CPD, it seems to me that the above symptoms are most often evaluated somewhat in isolation, since each symptom taken alone may have its own differential diagnosis. What is often overlooked is that all or virtually all these GI symptoms can be traced to the single explanation of R-CPD, using the principle of Occam’s Razor.
- Unfortunately, the availability of the above understandings notwithstanding, some patients continue to experience a lot of “friction” in the medical system that often prolongs suffering needlessly and induces understandable/justifiable frustration, desperation, cynicism, anger, and medical jadedness. I would propose that the time has come to say that when the diagnosis of R-CPD is presented to them by patients, the onus is now squarely on the medical profession and its bureaucracy, and particularly on gastroenterologists.
- I would argue that R-CPD is best diagnosed and managed via a match to a syndrome, and not via an extensive battery of tests. It is a prima fascia diagnosis, as explained below. Patients can easily recognize it in themselves with virtually 100% accuracy. Doctors who are open to learn about this disordercan do the same.
- To put emphasis on how high the stakes are for patients, I repeat from above, a typical response from a patient, after she was treated for R-CPD:
“This procedure has been truly life changing for me. I feel so much more comfortable and have so much control over my burping now. I also believe this has fixed a lifelong string of crippling episodes of abdominal pain that have landed me in the hospital multiple times and even led to the removal of my gallbladder (which was not the problem).”
More about R-CPD
My initial publication of 51 patients in 2019, contains all the information treating physicians need (though not all that medical scientists will want) to successfully diagnose and treat persons with R-CPD. I have put an additional 4 articles into the peer-reviewed literature.
In the interest of improving accessibility to physicians and patients, I have created a large body of work here on my personal teaching and public service website. A simple search there of the term “R-CPD” will bring up not only my published articles, but also several hours of information (articles, blogposts, video programs, panel discussions, etc).
The names of other physicians knowledgeable about R-CPD and with successfully treated caseloads can be found on Bastian Voice Institute.
I have come to understand from overwhelming experience that R-CPD is really a disorder handled best by doctors who are classical physicians, focused on patient care. Those who lean more to being medical scientists, admirable though they may be, may suffer a disadvantage.
I have wondered if the doctors with the latter proclivity respect measurement, and are inclined to dismiss the power of patient history and observation for this diagnosis, to the detriment of their patients. (The two approaches are of course not mutually exclusive.)
I spoke only yesterday with a young woman and her parents from Ohio whose life has been ruined so far by unrecognized R-CPD. She has been to the most sophisticated centers and seen noted gastroenterologists. She even has a G-tube and receives an extremely slow drip of tube feedings 24/7, after her weight fell to just 88 lbs due to constant nausea. She has told doctors for years that her issue is that she cannot burp.
Sir William Osler was a noted father of medical science; nevertheless, he said something like: If you listen to the patient, he will tell you what is wrong with him. This is profoundly true for R-CPD. Testing will get you nowhere for this diagnosis. Arguably, testing can be viewed as harmful because it delays diagnosis and treatment for no benefit.
Why do I say such an outrageous thing? Because I cannot ignore my experience. Of the nearly 1700 patients in our R-CPD caseload (we clinicians compare notes), the aggregate number of major tests must approach at least 10,000. It is likely closer to 15,000. Some patients have endured multiples of tests like barium swallows, endoscopies (upper and lower), bolus scintigraphy, manometry, stool examination for SIBO, gluten and lactose intolerance testing, KUB and CT xrays … and on and on.
And the result? Physicians arrived at a correct diagnosis of R-CPD in exactly zero patients. Instead, there were a lot of “findings” such as slow esophageal transit, hypotonic LES, and a great deal of “normal.” After all this, patients are discouraged and “hopeless,” to put it mildly. They have missed so much work, have endured endless tests and treatments, and have nothing to show for it, or are burdened with diagnoses and treatments that lead nowhere. They sometimes reach a state of what I call “medical jadedness.”
For emphasis, I would repeat that based in exhaustive testing, there have indeed been diagnoses made, like acid reflux, irritable bowel syndrome, myenteric plexus disorders, gastroparesis, aerophagia, SIBO, gluten intolerance, etc.
To date, these have all been dead ends in terms of providing relief to the patient.
The test findings that triggered these diagnoses have almost all been the result rather than cause of the patient’s syndromic disorder (R-CPD) and not independent disorders. The most vigorous treatment of these many diagnoses either does nothing, or at most in a few, mutes some symptoms modestly.

When instead of exhausting patients with unnecessary tests, we recognize the syndrome prima fascia and both test and treat them for R-CPD with a botulinum toxin injection to the UES, virtually all these other diagnoses have fallen away, with the exception of a lot of acid reflux (the result, and not cause, of years of untreated R-CPD, we believe), and gluten intolerance at a rate that I am sure mirrors the general population.
This is why I have come to say, “If you match the syndrome of R-CPD, all GI symptoms are the result of R-CPD until proven otherwise AFTER successful treatment of your R-CPD.
We have one patient who has seen 13 different GI doctors. She says that the last of them, a famous esophagologist, told her, “If you do the botox treatment you will aspirate and die.” We have several who have seen 3. And many, many who have seen one, often repeatedly. Even my own GI colleagues had been dubious until our caseload had reached into the hundreds.
What about the diagnostic accuracy of match to the syndrome? It is as close to 100% as one ever finds in medicine. We offer advance Zoom conversations with faraway patients. Yet, as testimony to my confidence in the power of the syndromic diagnosis in the hands of patients, we also permit them to fly to us from Miami, Dallas, San Francisco, Canada, South America, etc. before we ever meet them. We see them in the office one afternoon, validate their self-identification as having R-CPD, and treat them the following morning.
So far in my personal caseload, only 2 of nearly 1000 have so far been turned away as not having matched themselves adequately to the syndrome. If memory serves, we have only a handful whose first injection did not initiate burping and deliver relief of the associated symptoms above. I speculate that it may have been an issue with botulinum toxin quality, or targeting issue, not an incorrect diagnosis. And a subsequent injection then validated the diagnosis…
Approximately 80% of those treated achieve what we call “once and done” results, meaning that they continue to burp and have relief from R-CPD symptoms for (to date) as many as 8 years after a single injection.
Considering all the above, you will understand why, when I teach a course on this disorder, I often say “If patients can self-diagnose this accurately, doctors can do as well or better.”
Questions Skeptical Doctors Might Ask
You have noted, and posted on Laryngopedia, chest x-rays or KUB films your patients have brought you, showing massive amounts of GI air. Doesn’t this mean that aerophagia more than inability to burp explains all the symptoms and findings of R-CPD?
As best we can understand, the aerophagia is the result of the misery of being unable to burp. Many patients describe discomfort and nausea-induced hypersalivation and repetitive reflexive swallowing. They say it is like the repetitive swallowing they do when “drooling” due to nausea just before they throw up. R-CPD feel discomfort and /or nausea regularly. They are sure they would not swallow repetitively if only they could burp!
A few have taken to spitting into a cup to try to stop swallowing air when they become uncomfortable, needing to burp. And this helps diminish symptoms somewhat.
Consider this: Whether you call the disorder (incorrectly) “Aerophagia and Refusal to Burp…” or “R-CPD,” our botox treatment nevertheless “fixed” 1700 people. The botox apparently didn’t care what the disorder was called… And if you ask patients whether they think the problem is in the first instance aerophagia, or inability to burp, they will answer in chorus, “Inability to burp.” They long to burp, but cannot.
You say in some of your articles and videos that extensive testing in many of your patients has revealed real abnormalities, such as slow esophageal transit; hypotonia of the LES; gastroparesis; SIBO; a floppy sigmoid colon, etc. And yet you seem to say that these abnormalities are not important! It seems so shallow! So simplistic!
I wouldn’t say they are unimportant. It is just that these secondary findings distract and misdirect attention from the primary diagnosis: R-CPD. These findings came from prior doctors’ workups before the diagnosis of R-CPD was made at BVI. And they had triggered all manner of treatments that failed to resolve the syndrome as a whole.
As for the findings themselves: What would we expect from a chronically over-stretched esophagus? Slow transit, and a hypotonic LES. From a dramatically stretched stomach on a daily basis for years? Gastroparesis. From a chronically stretched colon due to extreme flatulence? Constipation and even volvulus.
How can excess air alone lead to something as severe as volvulus or bowel obstruction?
Easily. We have seen patients who have had to visit ER several (sometimes numerous) times for NG placement and decompression. Dramatic pressure and kinking of bowel or marked displacement are documented elsewhere here on Laryngopedia. To find these, search “R-CPD” on this site. Here’s the link to the post on the abdominal distention of R-CPD that is so common.
And here’s a video that explains the difference between abdominal distention and abdominal crisis, represented by the thumbnail below.
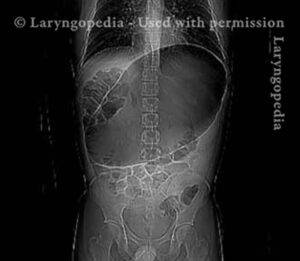
Such compression or displacement can be so severe that the person can neither burp nor pass gas or have a bowel movement. The patient in the x-ray above has experienced dramatic relief of his terrible daily distress for months after each of two botox injections. He slipped backwards a bit after injection #1. We are hoping to put him in the “twice and done” column.
And then consider that there are publications written before R-CPD had been described that link massive abdominal air from aerophagia with volvulus. Consider the following two articles: Transverse Colon Volvulus in a Child with Pathologic Aerophagia and Colon Perforation Due to Pathologic Aerophagia in an Intellectually Disabled Child. I speculate that the two case reports may have represented unrecognized R-CPD.
Regarding the second article, I have a personal patient who is intellectually disabled who—pre-Botox—appeared pregnant at the end of every day. Before treatment, she decompressed through the night and was flat each morning, only to start the same sequence over again the next day. After treatment with Botox, that patient’s mother sent a note of appreciation with a before—and after—Botox pair of photos that are heart-warming.
Don’t you think this is a functional disorder that might better be handled by a psychologist? To do something like cognitive-behavioral therapy to stop swallowing so much air?
If only this were a disorder that could be addressed that way! If only we could find some sort of secondary gain to put the spotlight on. But I believe that even the most sceptical person reading this open letter would swallow air reflexively not for secondary gain, but in response to the deeply miserable inability to burp. Even a highly sceptical gastroenterologist might eventually develop the entire syndromic features of R-CPD if she or he were unable to burp and developed the accompanying symptoms after a time.
I need to protest the simple-mindedness of your approach by asking again, how you can go straight to the diagnosis of R-CPD without running at least a few preliminary tests?
We of course do an office examination, to assess suitability for either office EMG or Operating Room endoscopic injection. Still, I repeat: experience with nearly 1000 personal (nearly 1700 group) patients by early 2024 has taught us that this is a prima fascia diagnosis. And, other than for a few outliers, the inability to burp / severe burping insufficiency has been lifelong. (They may initially say “it started when I was 18” but they mean that was when it started to become noticeable. When the full-blown syndrome expressed itself. When asked if they could burp before that age, they all say “no.”)
Furthermore, we would ask, rhetorically: If there is a lengthy list of intellectually appealing tests, why not do the botulinum toxin “test” first? It is far easier on patients (they tell us) than manometry. And colonoscopy. And likely less expensive than approximately two other tests put together. And the risk is essentially nil.
You mention risk: Has anybody come to harm from proceeding directly to the combined diagnostic test/ treatment represented by botulinum toxin injection?
I personally have a case of prevertebral cellulitis and another small perforation of the pyriform sinus. These were anatomically the two most difficult patients in my caseload (extreme retrognathism, very large teeth, short neck, etc.). These complications were—or could have been in one case treated elsewhere—managed very simply. We have a few with a roughened area on a tooth that we “smoothed off” at the conclusion of the case. Nobody to my memory has needed to see a dentist.
But I insist on something objective to define this disorder.
Done! A group in Amsterdam took 8 patients already diagnosed with inability to burp (note my emphasis) and measured high UES pressure and lack of burping by administering effervescent granules into the esophagus.
I’ve already said that standard manometry has defined this problem in zero of my patients. I would estimate maybe 100 had submitted to that test prior to coming to BVI. The Amsterdam group has given us a test that tells us when a patient can’t burp. But haven’t patients already told us this?
Conclusion
We all proceed by our own lights. But doctors who do not believe R-CPD is a valid syndrome after being presented with the idea are resisting a torrent of peer-reviewed and other information available from doctors all around the world about R-CPD and the results of treatment.
And so, doctors who still do not accept this diagnosis should send their patients to doctors who have extensive experience with R-CPD. To withhold consideration of this diagnosis and its requisite test/treatment would seem to me a breach of medical ethics.
Share this article
What is the Relationship between R-CPD and GERD? SIBO? IBS?
Often, and almost routinely, persons with easily-diagnosed R-CPD may initially be diagnosed instead as “gastroesophageal reflux disease” (GERD), or “irritable bowel syndrome,” (IBS) or “small intestine bacterial overgrowth” (SIBO).
Do GERD, IBS, and SIBO symptoms and findings point to coexisting and separate diagnoses, or are those symptoms part of the larger, umbrella diagnosis of R-CPD? Dr. Bastian discusses these questions in this video.
RCPD Workup – Do You Need Testing for a Diagnosis?
What is necessary to diagnose R-CPD? What is sufficient? Do we need to spend thousands of dollars for x-rays, manometry, upper GI scopes, gastric emptying studies?
Can’t Burp? This May Explain Why
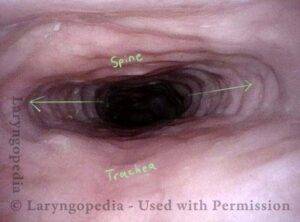
You may have R-CPD or retrograde cricopharyngeus dysfunction. In this condition, the upper esophageal sphincter (cricopharyngeus muscle) works normally from above to permit swallowing, but it refuses to relax from below to let air be belched out.