Necrosis is the death of cells or tissue. In laryngology, it is seen most commonly after radiation therapy to the larynx for cancer treatment. Radiation kills the tumor but at the same time damages the blood supply of normal tissue on a permanent basis. Necrosis in this instance is called “radionecrosis.”
Necrosis could also result from trauma (a physical wound) that disrupts blood supply, or occasionally in the context of ulcerative laryngitis, which seems to necrose the superficial layers of the vocal cords. Necrotic tissue typically sloughs off down to viable (living) tissue.
Necrosis, Before and After Discontinuing Bevacizumab
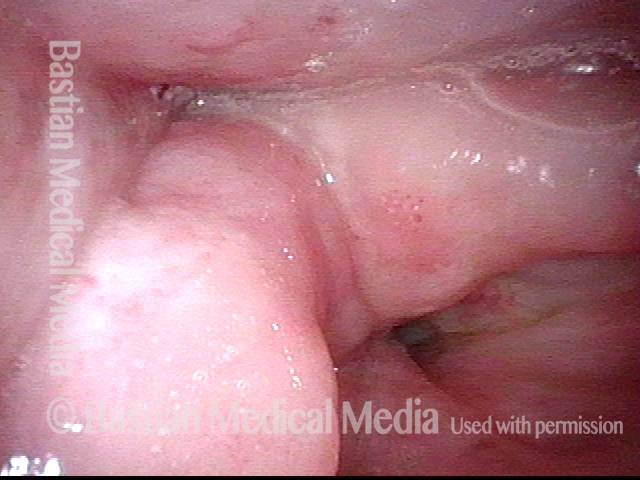
Necrosis (1 of 6)
Biopsy of hazy, superficially ulcerated lesion on right vocal cord (left of image) shows only “necrosis.” There is no proof but only a question whether this necrosis may be a side effect of the bevacizumab (Avastin) the patient is taking for lung cancer.
Necrosis (1 of 6)
Biopsy of hazy, superficially ulcerated lesion on right vocal cord (left of image) shows only “necrosis.” There is no proof but only a question whether this necrosis may be a side effect of the bevacizumab (Avastin) the patient is taking for lung cancer.
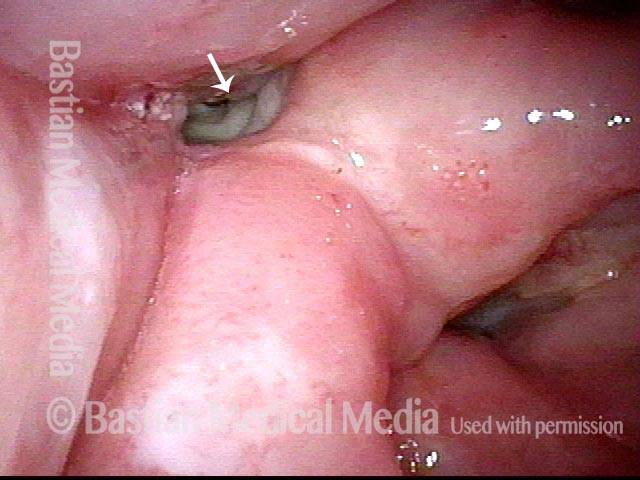
Necrosis (2 of 6)
Open phase of vibration (strobe light) shows that only the left cord (right of image) oscillates.
Necrosis (2 of 6)
Open phase of vibration (strobe light) shows that only the left cord (right of image) oscillates.
Necrosis (3 of 6)
Closed phase of vibration (strobe light) shows that closure is result of left cord excursion.
Necrosis (3 of 6)
Closed phase of vibration (strobe light) shows that closure is result of left cord excursion.
Necrosis, after discontinuing bevacizumab (4 of 6)
Several months after discontinuing bevacizumab, the right vocal cord ulcer has healed.
Necrosis, after discontinuing bevacizumab (4 of 6)
Several months after discontinuing bevacizumab, the right vocal cord ulcer has healed.
Necrosis, after discontinuing bevacizumab (5 of 6)
Narrow band illumination accentuates the ingrowth of new capillaries.
Necrosis, after discontinuing bevacizumab (5 of 6)
Narrow band illumination accentuates the ingrowth of new capillaries.
Necrosis, after discontinuing bevacizumab (6 of 6)
Phonatory match (standard light) is improved, but the right vocal cord (left of image) remains stiff, as the ulcer has been replaced by scar tissue.
Necrosis, after discontinuing bevacizumab (6 of 6)
Phonatory match (standard light) is improved, but the right vocal cord (left of image) remains stiff, as the ulcer has been replaced by scar tissue.
Radionecrosis
Radionecrosis (1 of 4)
This patient was originally treated for early vocal cord cancer with radiation. Tumor persistence required hemilaryngectomy. Then nearly a year later, he developed a neck metastasis (in a lymph node). Neck dissection was performed, but the tumor was found to have penetrated the capsule of the lymph node (a high-risk finding for recurrence), so he received “insurance policy” proton beam radiotherapy of the right side of the neck. Unfortunately the posterior edge of the thyroid cartilage became necrotic due to the “double dose” of radiation. In this view, one only sees swelling of the right arytenoid mound, but the pyriform sinus is closed and the necrotic area cannot yet be seen.
Radionecrosis (1 of 4)
This patient was originally treated for early vocal cord cancer with radiation. Tumor persistence required hemilaryngectomy. Then nearly a year later, he developed a neck metastasis (in a lymph node). Neck dissection was performed, but the tumor was found to have penetrated the capsule of the lymph node (a high-risk finding for recurrence), so he received “insurance policy” proton beam radiotherapy of the right side of the neck. Unfortunately the posterior edge of the thyroid cartilage became necrotic due to the “double dose” of radiation. In this view, one only sees swelling of the right arytenoid mound, but the pyriform sinus is closed and the necrotic area cannot yet be seen.
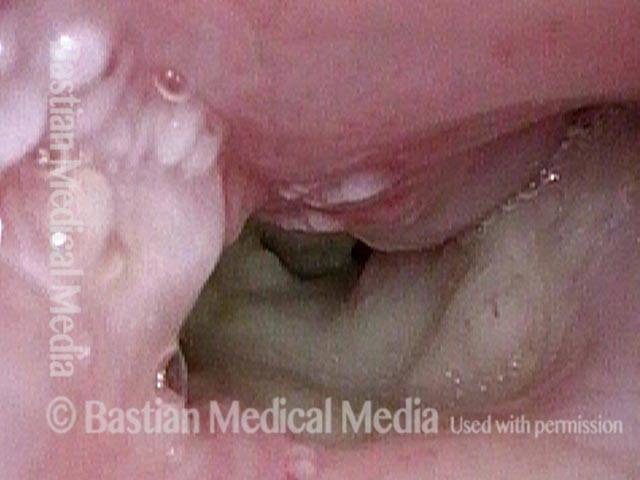
Radionecrosis (2 of 4)
Here, the patient is performing the trumpet maneuver to splay open the right pyriform sinus. The area of necrosis is beginning to be seen at arrow.
Radionecrosis (2 of 4)
Here, the patient is performing the trumpet maneuver to splay open the right pyriform sinus. The area of necrosis is beginning to be seen at arrow.
Radionecrosis (3 of 4)
The necrotic tissue is seen here at a much closer range.
Radionecrosis (3 of 4)
The necrotic tissue is seen here at a much closer range.
Radionecrosis (4 of 4)
An even closer view into the necrotic pyriform sinus. Multiple biopsies have been taken from this area to be sure there is no cancer. Eventually, this larynx had to be removed not for cancer, but for this radiation complication.
Radionecrosis (4 of 4)
An even closer view into the necrotic pyriform sinus. Multiple biopsies have been taken from this area to be sure there is no cancer. Eventually, this larynx had to be removed not for cancer, but for this radiation complication.
Anterior Commissure-to-subglottis Fistula Complication of Radiation
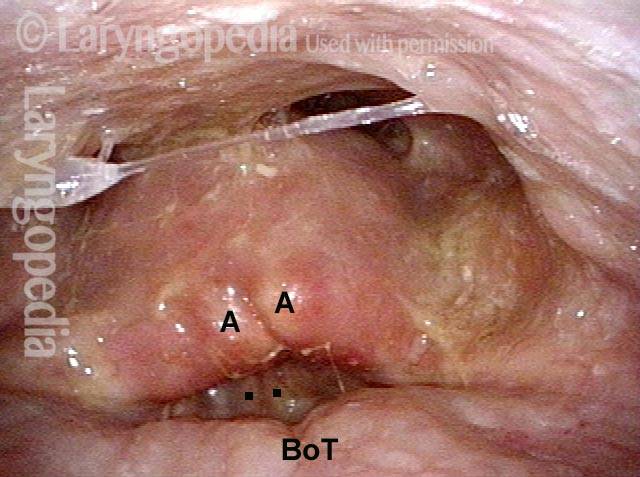
Larynx losing function (1 of 4)
This man underwent supraglottic laryngectomy and radiotherapy nearly 20 years ago. A biopsy was done some years later elsewhere, and triggered radionecrosis. Hyperbaric oxygen treatments back then saved the day. This larynx has continued to lose function slowly over time, necessitating tracheotomy, and with deteriorating voice quality. The latest problem is coughing on liquids, and they are coming out his tracheotomy tube. Here, you see the arytenoid apices (each marked with A). Epiglottis and false vocal cords are surgically absent. Base of tongue (BoT) was pulled down to the level of the vocal cords. Click to enlarge this photo to see the dots marking the upper surface of each cord.
Larynx losing function (1 of 4)
This man underwent supraglottic laryngectomy and radiotherapy nearly 20 years ago. A biopsy was done some years later elsewhere, and triggered radionecrosis. Hyperbaric oxygen treatments back then saved the day. This larynx has continued to lose function slowly over time, necessitating tracheotomy, and with deteriorating voice quality. The latest problem is coughing on liquids, and they are coming out his tracheotomy tube. Here, you see the arytenoid apices (each marked with A). Epiglottis and false vocal cords are surgically absent. Base of tongue (BoT) was pulled down to the level of the vocal cords. Click to enlarge this photo to see the dots marking the upper surface of each cord.
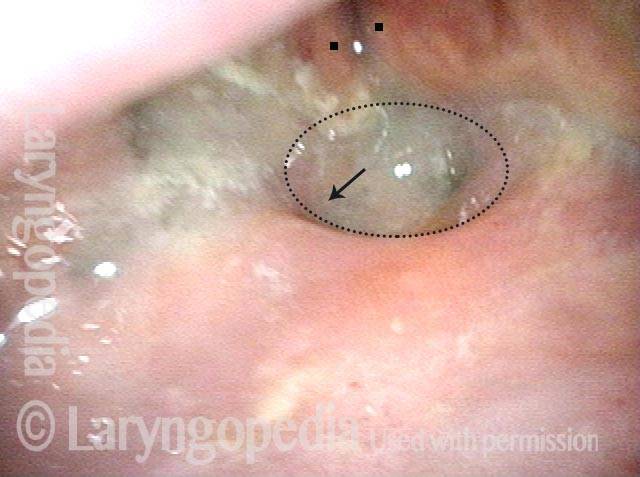
Swallowing (2 of 4)
Now looking deep into the surgically-minimized laryngeal vestibule, the two larger dots are again on the vocal cords, for comparison with photo 1. The fine dotted line encircles a fistula. When the patient swallows, food or liquid can enter in the direction of the arrow. Where it goes next is seen in the following photos.
Swallowing (2 of 4)
Now looking deep into the surgically-minimized laryngeal vestibule, the two larger dots are again on the vocal cords, for comparison with photo 1. The fine dotted line encircles a fistula. When the patient swallows, food or liquid can enter in the direction of the arrow. Where it goes next is seen in the following photos.
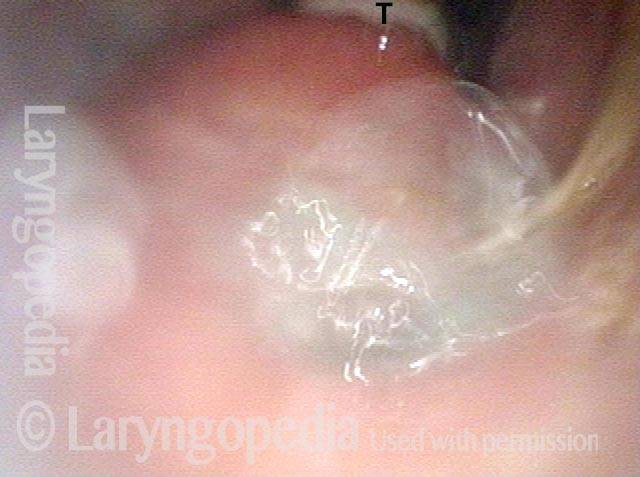
View from between vocal cords (3 of 4)
The scope has entered between the cords (between the dots in photo 2), and is now viewing the subglottis. “T” near the top of the photo marks where the tracheotomy tube is seen entering the trachea. The anterior subglottic fistula is seen at the bottom of the photo with the sidewall of the tracheotomy tube seen at the lower-case “t.”
View from between vocal cords (3 of 4)
The scope has entered between the cords (between the dots in photo 2), and is now viewing the subglottis. “T” near the top of the photo marks where the tracheotomy tube is seen entering the trachea. The anterior subglottic fistula is seen at the bottom of the photo with the sidewall of the tracheotomy tube seen at the lower-case “t.”
Swallowing water (4 of 4)
Remaining in the anterior subglottis while the patient swallows pale blue-stained water, you see a part of the bolus “exploding” through the fistula, and this series of 4 photos taken together fully explain why this man is having so much difficulty with liquids that he swallows coming out his tracheotomy tube.
Swallowing water (4 of 4)
Remaining in the anterior subglottis while the patient swallows pale blue-stained water, you see a part of the bolus “exploding” through the fistula, and this series of 4 photos taken together fully explain why this man is having so much difficulty with liquids that he swallows coming out his tracheotomy tube.