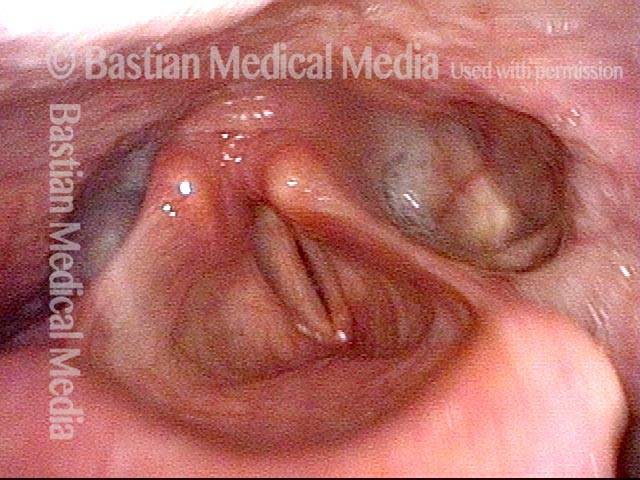
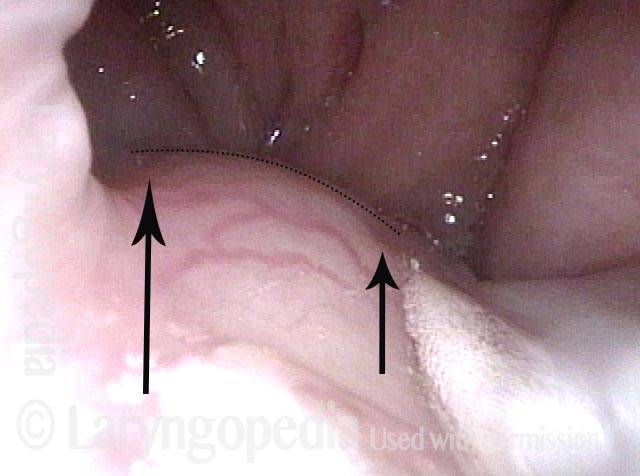
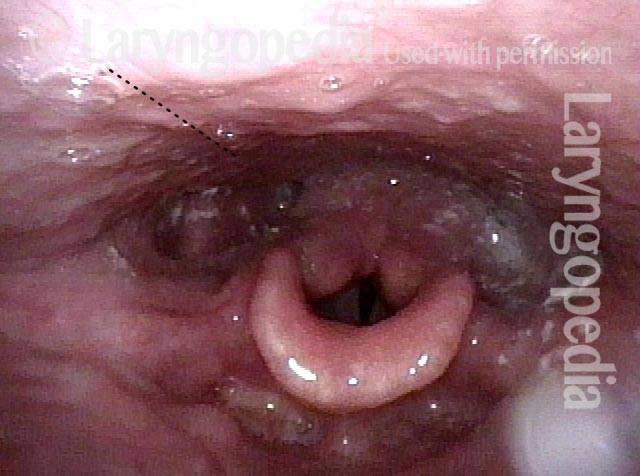
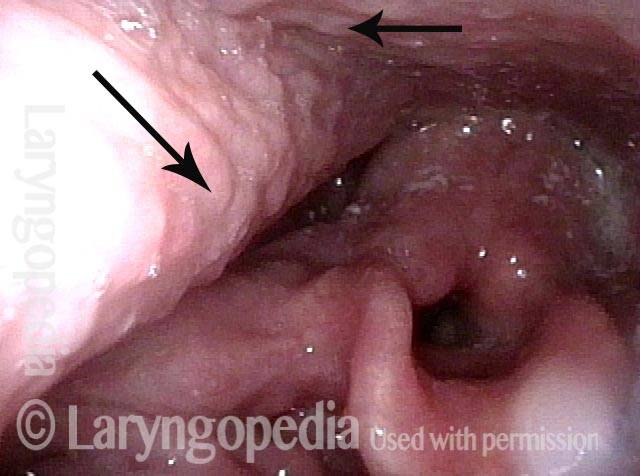
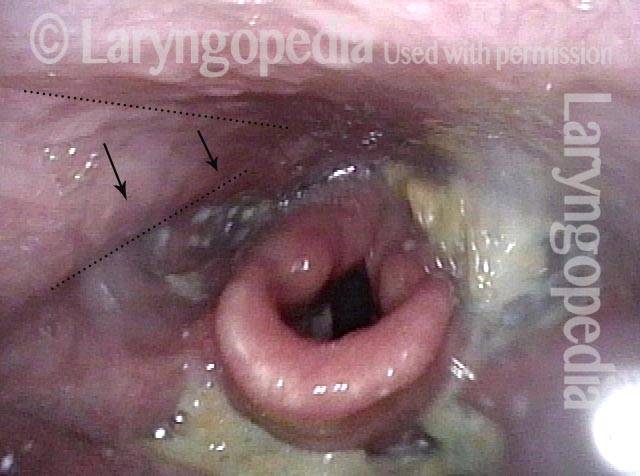
Palate paralysis is loss of motion of the muscle in the soft palate, so that the palate does not properly elevate. Normally, the soft palate elevates to seal the nasopharynx when swallowing or when pronouncing any non-nasal sounds (in English, all sounds except for “n,” “m,” and “ng”). However, if the vagus nerve is damaged high in its course, near the base of skull, then the palate on that side can lose its ability to lift, and it remains down during the aforementioned tasks.
Symptoms
A patient with palate paralysis might experience not only hypernasality (speech resonance quality resembling that heard with cleft palate) but also nasal regurgitation, especially of liquids (“water comes out my nose when I swallow”), and also nasal emissions (a slight hissing sound that comes through the nose when the person produces strong consonants).