Inflammation of mucosa caused by cancer-treating radiation. Mucositis is to mucosa as dermatitis is to skin. This inflammation appears reddish with patches of greyish superficial necrosis or ulceration. Typically, radiation mucositis fully resolves four to six weeks after the last radiation treatment.
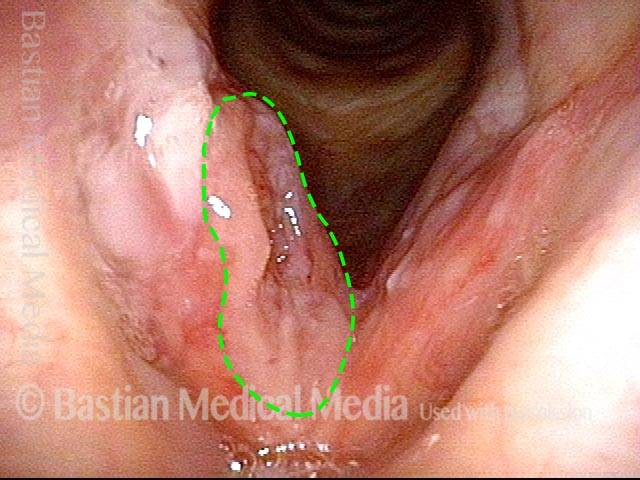
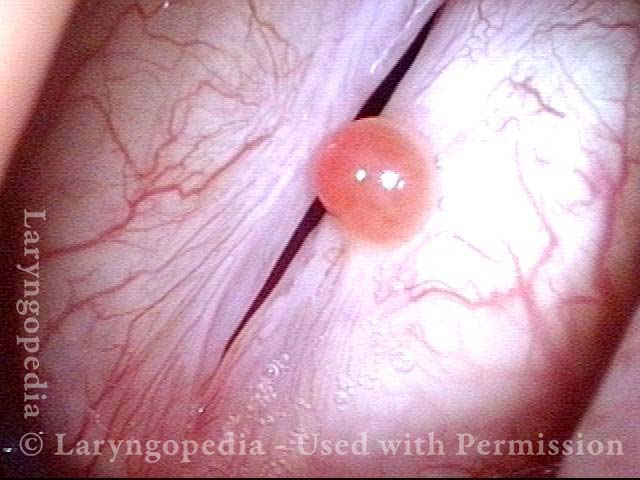
Prior to start of radiation (1 of 4)
Prior to start of radiation (1 of 4)
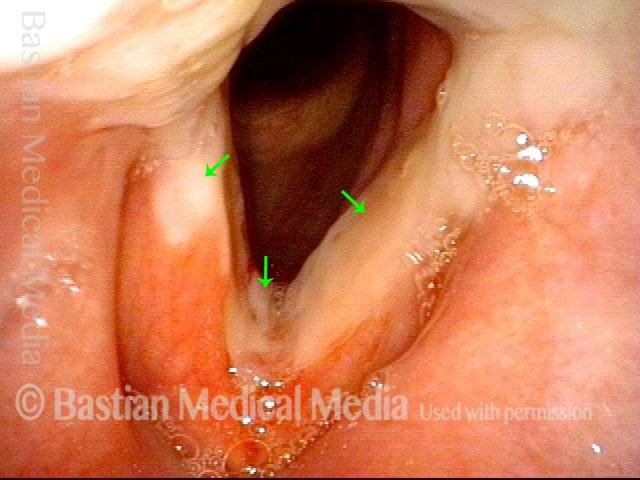
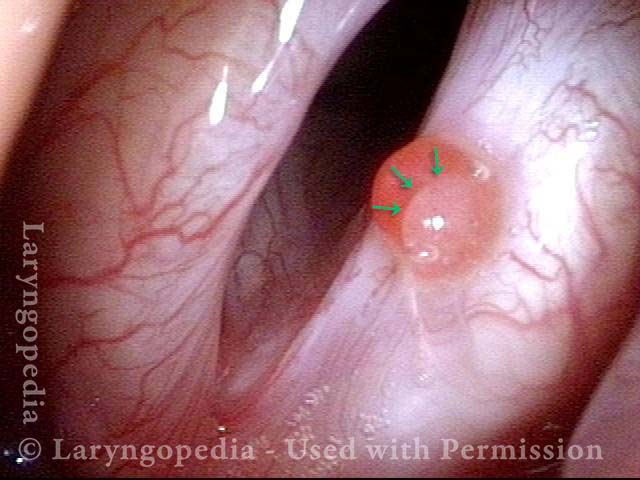
Radiation mucositis, 1 week after radiation (2 of 4)
Radiation mucositis, 1 week after radiation (2 of 4)
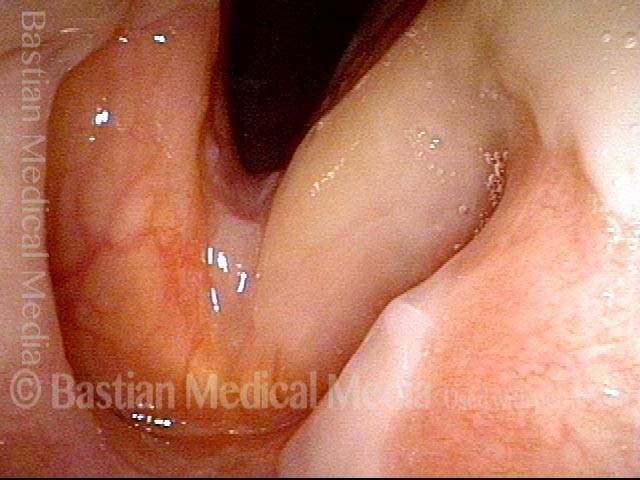
Radiation mucositis, 4 weeks after radiation (3 of 4)
Radiation mucositis, 4 weeks after radiation (3 of 4)
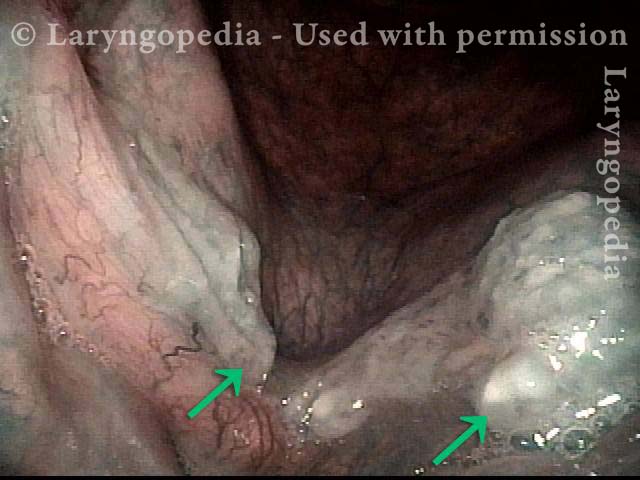
Disappearing radiation mucositis, 10 weeks after radiation (4 of 4)
Disappearing radiation mucositis, 10 weeks after radiation (4 of 4)
Laser Removal of Vocal Cord Cancer with Bilateral Disease
For treatment of early vocal cord cancer, both laser excision and radiotherapy are in competition as good treatment modalities. See also Early Vocal Cord Cancer: Remove with a Laser, or Radiate? Often, radiation is used when disease is bilateral, in the interest of preserving voice. This is an example of the ability to do fairly extensive laser surgery bilaterally, yet preserving good voice. This man had a friend who had severe difficulty with radiation, and he was therefore opposed to that option.