The subglottis is the lower part of the larynx, from just below the free margin of the vocal cord to the upper end of the trachea.
Does this Person Really Need Tracheal Resection? Let’s see…
Distant view of vocal cords (1 of 3)
Wide-angle view of vocal cords and subglottis, with white tracheotomy tube in evidence. This person was sent for resection of a stenotic (scarred, narrowed) tracheal segment, and repair. The patient can barely breathe when her trach tube is plugged for one or two breaths as a test. In this distant view, we can't evaluate the trachea, but do see posterior vocal cord tissue loss caused by a prior endotracheal tube injury (area enclosed by dotted lines).
Distant view of vocal cords (1 of 3)
Wide-angle view of vocal cords and subglottis, with white tracheotomy tube in evidence. This person was sent for resection of a stenotic (scarred, narrowed) tracheal segment, and repair. The patient can barely breathe when her trach tube is plugged for one or two breaths as a test. In this distant view, we can't evaluate the trachea, but do see posterior vocal cord tissue loss caused by a prior endotracheal tube injury (area enclosed by dotted lines).
Trach tube (2 of 3)
Sometimes, as depicted here, the tube itself obstructs a stenotic segment that, without the tube, might be large enough that tracheal resection/ reanastomosis is not needed.
Trach tube (2 of 3)
Sometimes, as depicted here, the tube itself obstructs a stenotic segment that, without the tube, might be large enough that tracheal resection/ reanastomosis is not needed.
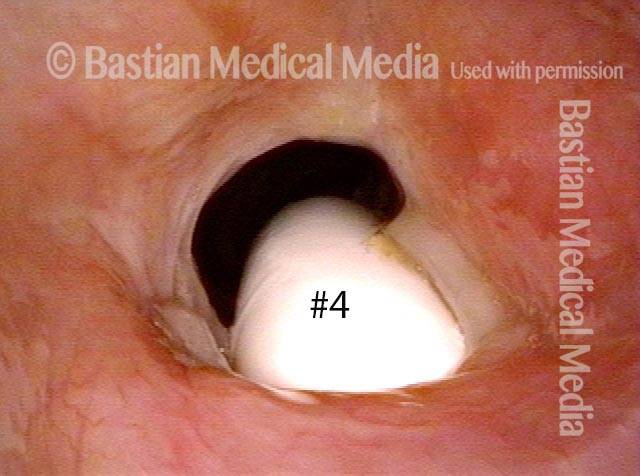
Smaller tube (3 of 3)
The #6 tube in photo 2 has been replaced here with a #4 (smaller) tube. The posterior thrust of the curvature of the smaller tube is less; furthermore, the diameter is smaller. For both reasons, there is much more space for "blow-by" and the patient can breathe quite well with the tube plugged. If she can tolerate it plugged 24/7 except for routine cleaning, the tube can be removed, giving even more space for passage of air. This careful process may remove the need for surgical repair.
Smaller tube (3 of 3)
The #6 tube in photo 2 has been replaced here with a #4 (smaller) tube. The posterior thrust of the curvature of the smaller tube is less; furthermore, the diameter is smaller. For both reasons, there is much more space for "blow-by" and the patient can breathe quite well with the tube plugged. If she can tolerate it plugged 24/7 except for routine cleaning, the tube can be removed, giving even more space for passage of air. This careful process may remove the need for surgical repair.
Pinhole Opening in Near-Complete Subglottic Stenosis
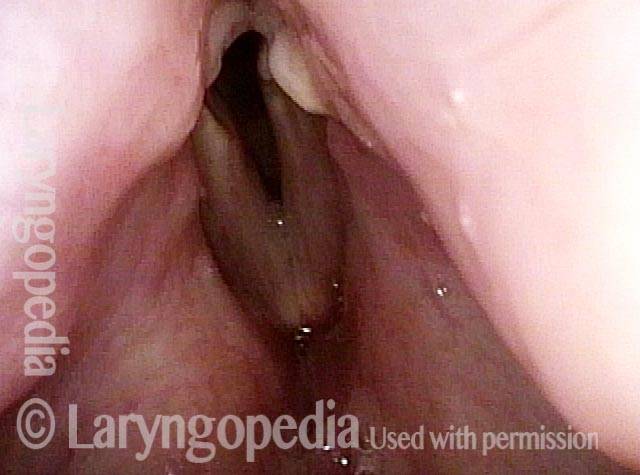
Narrowed space for breathing (1 of 4)
This man was gravely ill and intubated for several weeks. He is now well, but tracheotomy-dependent. The vocal cords do not abduct fully due to scarring of the cricoarytenoid joints. However, the narrowed space for breathing between the posterior vocal cords is not the main reason he is tracheotomy-dependent, as seen in the next photos.
Narrowed space for breathing (1 of 4)
This man was gravely ill and intubated for several weeks. He is now well, but tracheotomy-dependent. The vocal cords do not abduct fully due to scarring of the cricoarytenoid joints. However, the narrowed space for breathing between the posterior vocal cords is not the main reason he is tracheotomy-dependent, as seen in the next photos.
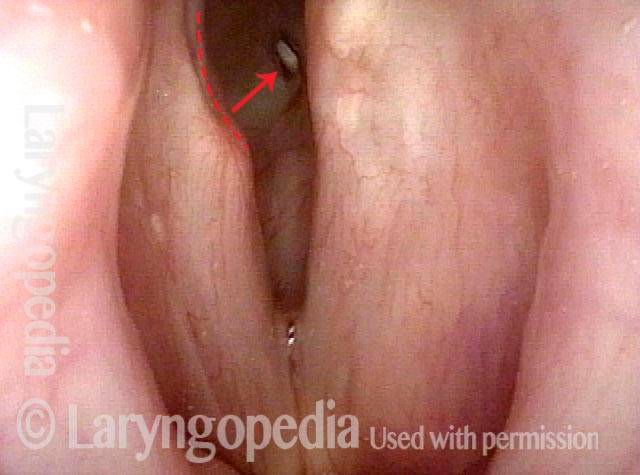
Looking between the vocal cords (2 of 4)
At closer range, a deep erosion “divot” of the right posterior vocal cord (left of photo at dotted line) is the result of pressure necrosis of the endotracheal tube. Looking between the vocal cords into the subglottic airway, a small white oval is seen (arrow). This is the upper surface of the white plastic tracheotomy tube.
Looking between the vocal cords (2 of 4)
At closer range, a deep erosion “divot” of the right posterior vocal cord (left of photo at dotted line) is the result of pressure necrosis of the endotracheal tube. Looking between the vocal cords into the subglottic airway, a small white oval is seen (arrow). This is the upper surface of the white plastic tracheotomy tube.
Closer view (3 of 4)
A closer view, again through the vocal cords.
Closer view (3 of 4)
A closer view, again through the vocal cords.
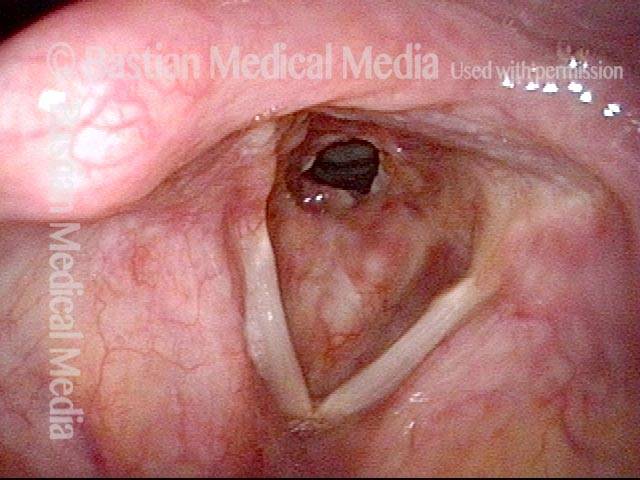
Space between subglottis and trachea (4 of 4)
At yet closer range. The size of this pinhole between subglottis and trachea below cannot measure more than 3 mm. Crico-tracheal resection and re-anastomosis (planned for soon after this examination) is the best option to work towards decannulation.
Space between subglottis and trachea (4 of 4)
At yet closer range. The size of this pinhole between subglottis and trachea below cannot measure more than 3 mm. Crico-tracheal resection and re-anastomosis (planned for soon after this examination) is the best option to work towards decannulation.
Subglottic Stenosis, Due to Wegener’s Granulomatosis
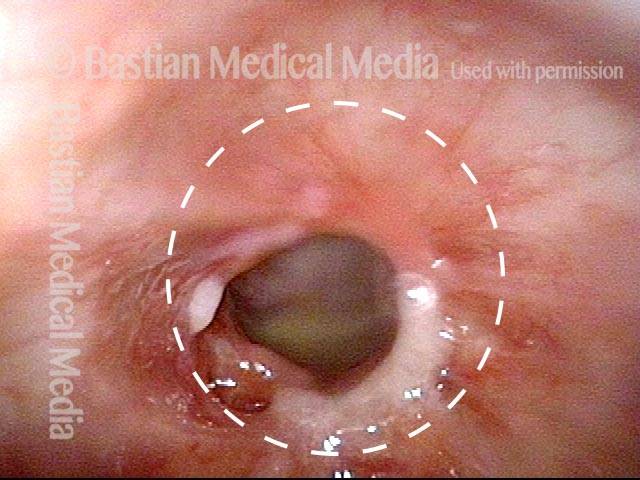
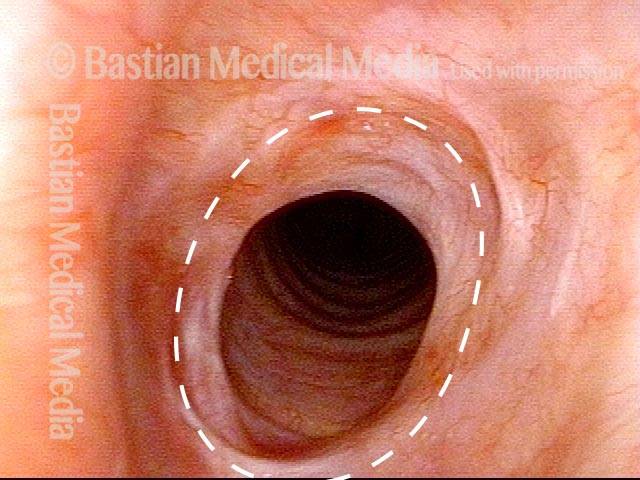
Subglottic stenosis, due to Wegener's (1 of 2)
This person has Wegener’s granulomatosis, confirmed by anti-neutrophil cytoplasmic antibodies (ANCA) testing. Here, looking from above the vocal cords, one can see an estimated 50% narrowing of the subglottic and high tracheal passageway.
Subglottic stenosis, due to Wegener's (1 of 2)
This person has Wegener’s granulomatosis, confirmed by anti-neutrophil cytoplasmic antibodies (ANCA) testing. Here, looking from above the vocal cords, one can see an estimated 50% narrowing of the subglottic and high tracheal passageway.
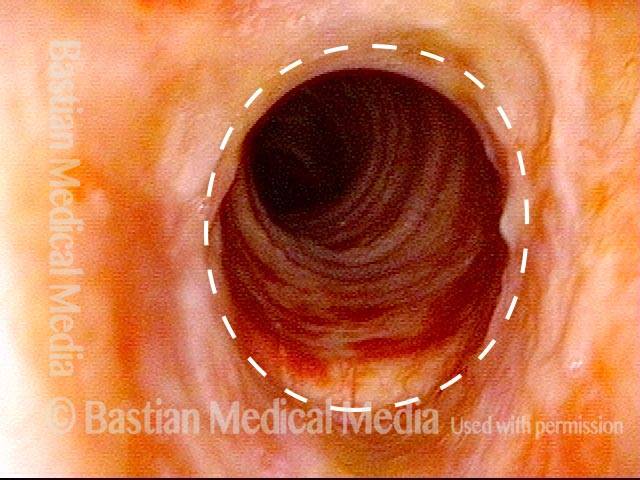
Subglottic stenosis, due to Wegener's (2 of 2)
Viewed from within the subglottis, one can see more clearly the inflammatory nature of this stenosis. A dotted oval estimates what the normal caliber or width of this airway would be. This patient has been managed with systemic medication, but also occasional dilation, steroid injection, and Mitomycin C application.
Subglottic stenosis, due to Wegener's (2 of 2)
Viewed from within the subglottis, one can see more clearly the inflammatory nature of this stenosis. A dotted oval estimates what the normal caliber or width of this airway would be. This patient has been managed with systemic medication, but also occasional dilation, steroid injection, and Mitomycin C application.
Airway Stenosis Caused By Wegener’s Granulomatosis, Before and After Dilations
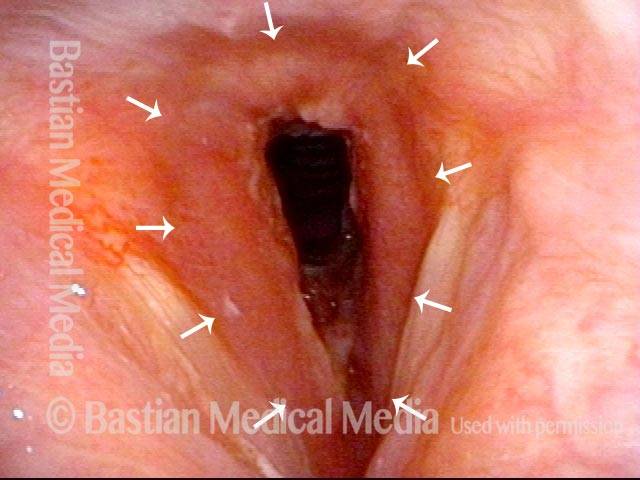
Airway stenosis (1 of 5)
Marked inflammatory narrowing in the immediate subglottis. Within the ring of arrows is the inflamed, reddened tissue, which is narrowing the airway into the shape of a slit. This man needs to be active for his work, but notices shortness of breath and noisy breathing with exertion.
Airway stenosis (1 of 5)
Marked inflammatory narrowing in the immediate subglottis. Within the ring of arrows is the inflamed, reddened tissue, which is narrowing the airway into the shape of a slit. This man needs to be active for his work, but notices shortness of breath and noisy breathing with exertion.
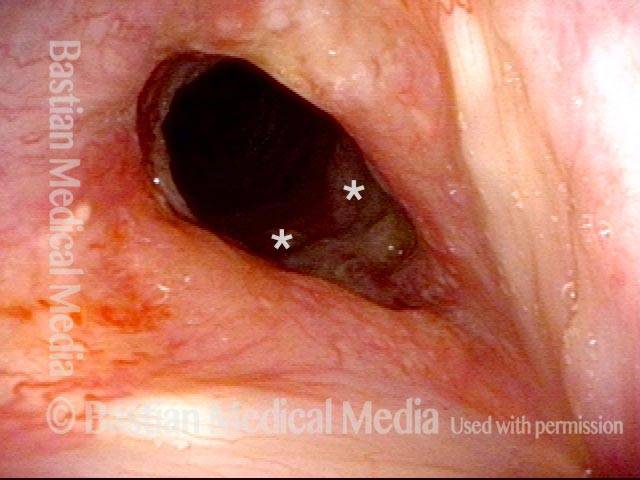
Airway stenosis, after dilation (2 of 5)
Nine days after a dilation procedure, with local steroid injection and painting with Mitomycin C. The airway has widened, so that it is more oval-shaped and less slit-like. Compare with photo 1. Although a degree of stenosis remains, symptoms have subsided dramatically. For reference, asterisks mark the same points in the subglottis in this photo and the next photo.
Airway stenosis, after dilation (2 of 5)
Nine days after a dilation procedure, with local steroid injection and painting with Mitomycin C. The airway has widened, so that it is more oval-shaped and less slit-like. Compare with photo 1. Although a degree of stenosis remains, symptoms have subsided dramatically. For reference, asterisks mark the same points in the subglottis in this photo and the next photo.
Airway stenosis, after dilation (3 of 5)
Same exam, looking beyond the immediate subglottis. There is an inflammatory response that involves several centimeters of the upper trachea. Inflammatory areas often “trap” mucus, as seen here.
Airway stenosis, after dilation (3 of 5)
Same exam, looking beyond the immediate subglottis. There is an inflammatory response that involves several centimeters of the upper trachea. Inflammatory areas often “trap” mucus, as seen here.
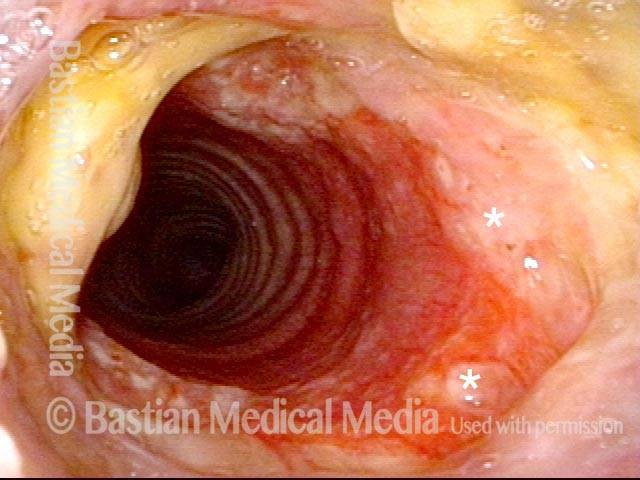
Airway stenosis, before another dilation (4 of 5)
Now five months after the dilation procedure mentioned in photos 2 and 3. The patient has been receiving systemic treatment with methotrexate and prednisone. General appearance of the inflammation has decreased. In spite of this, as expected, the stenosis has persisted (dotted oval shows the estimated caliber or width of a normal airway) and symptoms have gradually increased. Thus, another dilation was scheduled for the next day.
Airway stenosis, before another dilation (4 of 5)
Now five months after the dilation procedure mentioned in photos 2 and 3. The patient has been receiving systemic treatment with methotrexate and prednisone. General appearance of the inflammation has decreased. In spite of this, as expected, the stenosis has persisted (dotted oval shows the estimated caliber or width of a normal airway) and symptoms have gradually increased. Thus, another dilation was scheduled for the next day.
Airway stenosis, after another dilation (5 of 5)
A week after photo 4, following the most recent dilation. There is expected immediate postoperative inflammation and an increase in the airway’s caliber or width by an estimated 30% (dotted oval again shows the estimated caliber or width of a normal airway; compare with photo 4). Symptoms are again abolished.
Airway stenosis, after another dilation (5 of 5)
A week after photo 4, following the most recent dilation. There is expected immediate postoperative inflammation and an increase in the airway’s caliber or width by an estimated 30% (dotted oval again shows the estimated caliber or width of a normal airway; compare with photo 4). Symptoms are again abolished.
Tagged Anatomy & Physiology, Education