Babies Who Cannot Burp, and Still Cannot as Adults.
The Big Picture
Babies who cannot burp are in terrible misery. So are their parents. While the child struggles with daily colic, spitting up, sometimes projectile vomiting, and gassiness, the parents must deal with hours of crying each evening and much medical attention may have provided no answers.
The explanation for why some babies can’t burp may be found in the story of adults who had this kind of trouble in their infancy – trouble that has continued into adulthood.
Adults with a lifelong inability to burp were recently diagnosed with retrograde cricopharyngeus dysfunction, or R- CPD. This condition was successfully treated for the first time on record in November of 2016. The first publication of both the comprehensive syndromic criteria for diagnosis and the treatment with Botox was by Bastian and Smithson in March of 2019, in a review of their first 51 cases of a much larger subsequent caseload.
Bastian and colleagues have also published additional articles about R-CPD, on: the use of cricopharyngeus myotomy for recurrent cases; an alternate EMG-guided technique for injection; and longer term results.
As Background, Here Are the Primary Symptoms in Adults, Some of Whom had Trouble as Infants
Summarized from a caseload of nearly 600 patients treated, R-CPD’s debilitating adulthood syndrome typically consists of all–or at least some–of the following:
- Inability to burp. This could be recognized in childhood, teenage years, etc. Victims routinely say they do not remember being able to burp, except for the rare occasion.
- Easily audible and therefore socially awkward gurgling noises like croaking frogs, creaking floorboards, etc. made worse after eating or drinking.
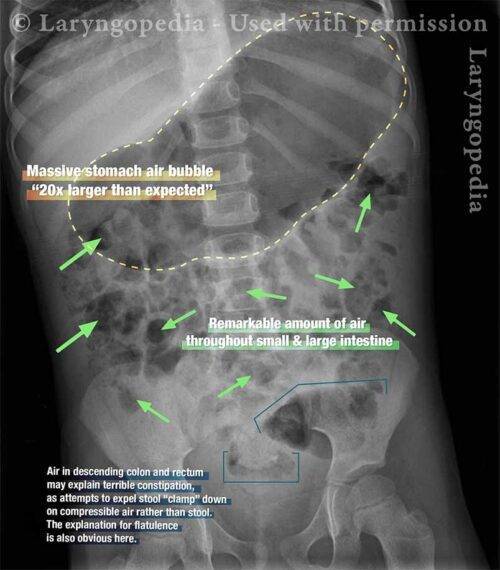
- Abdominal bloating (and often chest and even low-neck pressure).
- Flatulence that can be excessive or even extreme after meals, later in the day and into the night.
Other Common but Less Universal Symptoms
Can include painful hiccups, nausea after eating, a feeling of being so full it is almost hard to breathe when bloating is bad, and hypersalivation.
What is the linkage between this large adult caseload and babies and children who cannot burp?
A percentage of these adult patients know by family lore that they were unable to burp as infants. Parents who accompany them to their initial visit to BVI tell me that they (the parents) couldn’t burp them as infants. They also recount that this was in turn associated with extraordinary stress on the part of both baby and parents.
One mother said to me, “I couldn’t get him to burp conventionally, and he screamed in pain. Someone even told me to roll him on the floor, but he still wouldn’t burp.”
Another said, “He burped for the first two weeks of life, and then stop burping. At that point, he became incredibly gassy.”
Several parents have used words such as: “If she/he had been our first child, he/she would have been our only child.”
Others recount numerous trips to pediatricians searching in vain for a solution to the colic, projectile vomiting, ceaseless crying, and so forth.
One of the most extreme stories came from a father accompanying his teenage daughter. He told me that he and his wife had become concerned when their daughter was a baby because 20 to 30 minutes after every feeding, she would throw up what looked like everything they had just fed her. Fearing she would starve, they began measuring what they fed her and then standing by with a bowl to try to catch what she threw up to measure and compare.
Some describe a kind of failure to thrive and poor weight gain. One set of parents mentioned that even in toddlerhood, they had to chase the little one around to get him to the table to eat. And once there, he often refused the food they offered, due to the GI distress that inevitably followed.
 Children with R-CPD Need Champions
Children with R-CPD Need Champions
This four-year-old is an example of the many young children who fulfill the criteria for a diagnosis of R-CPD, but who cannot find a doctor to help. Her parents also say the following: “She was impossible to burp as an infant. She only eats small amounts, stopping due to discomfort, and is falling behind developmental markers (especially weight). Her abdomen blows up like a balloon each day. She requires daily laxative use, and passes a long stream of flatulence before moving her bowels.”
This child precociously describes what is clearly throat nausea, and speaks of trouble breathing and too much “throat water.” When she has hiccups (once a week or so), they hurt a lot.
For her age, this child has undergone significant testing and dietary manipulations, even medications, without any significant benefit. The friction and delay in the medical system of this family’s large city is so great, and the child’s (and her parents’) distress so intense that they are traveling hundreds of miles for the care of a physician who will treat expeditiously based upon the syndrome alone.
What Causes the Disorder in Adults and Possibly in Children too?
R-CPD is caused by a dysfunction of the upper esophageal sphincter, found at the level of mid-neck. The sphincter is comprised primarily of the cricopharyngeus muscle. It acts like a circular “gate” or “muscular purse-string” between the lower throat and upper esophagus. (There are 4 other sphincters in the GI tract, ending with the anus.)
Simplistically, think of the upper esophageal sphincter – cricopharyngeus muscle – being contracted/closed almost 24/7 and even during sleep. It relaxes very briefly, perhaps for 1 second, each time we swallow saliva, liquid, or solid food, clamping down on the “tail” of each bolus that passes through it and remaining contracted until the next swallow.
This same sphincter must also relax briefly to belch or to vomit. In persons with R-CPD, swallowing function (requiring antegrade sphincter relaxation) is normal. But opening for burping and often vomiting (requiring retrograde relaxation) is impossible or extremely difficult.
The result is severe daily misery caused by the combination of symptoms described above in bold.
For adults, injection of Botox into the upper esophageal sphincter can magically resolve this misery. And in about 80% of adults, a single injection of Botox into the sphincter can resolve or dramatically diminish symptoms permanently. Those who recur after Botox injection may achieve permanent relief after a second injection, and a small fraction who recur a second or third time after good relief may go on to cricopharyngeus myotomy.
Did all Adults with R-CPD have Difficulty Burping as Babies and Children?
No. Only a subset seems to have had such trouble that early in life. In my most recent 77 patients (the latest additions to a Bastian Voice Institute caseload nearing 1,400), here’s the breakdown:
- 18 were told they could not burp as infants (24%) and that it was a problem at some level
- 24 definitely could burp as infants (32%)
- 12 could burp as infants but had a history of colic, spitting up, vomiting, etc. (16%)
- 22 had no information (28%)
Of course, it is possible that some of these adults who could burp as babies, but had GI distress, were burping incompletely. And some who could not burp as babies may not have had the dramatic GI distress described in some of my anecdotes above. In other words, they may have been on the mild end of the spectrum. And it is possible that some babies who couldn’t burp grew up to become adults who could…
Still, it appears that there are a small number of babies in the world even today who, together with their parents, suffer profoundly in infancy and beyond, and so far, have been unable to find an explanation or relief.
What might be done for this group of babies/children with no other explanation for their misery (after profuse medical evaluations) than potential R-CPD? Could a subset of babies who can’t burp—the ones with extreme manifestations, failure to thrive, and whose parents who are “on the ledge”—be helped by a Botox injection too?
The very thought is obviously off-putting. But hold this thought alongside the absolute misery and anguish in the child, and of the sleep deprived parents due to their crying baby.
Consider also, that some of these babies continue to suffer well into adulthood. In fact, given a 7-point scale to indicate their view of the overall severity of their symptoms, the most common response in our large adult population by far is “6” and many choose “7.” Hence, treatment of the baby could possibly serve as “training wheels” for burping and avoid all those early years of misery and even misery extending decades into adulthood…
What Is the Solution?
I believe that somewhere, a courageous physician will partner with courageous (and desperate) parents to offer this treatment to a toddler or pre-schooler on the extremely severe end of the R-CPD continuum. It will require input from one or more pediatricians who have exhausted other ideas and diagnoses. They will need to see both the diagnostic and potential therapeutic potential of Botox administration. And there will need to be a precise plan about how to follow and monitor afterwards.
And eventually, after gaining confidence from having helped this early group of young children, it is possible that this treatment will—on a highly selective basis—be offered to a small number of babies in extraordinary distress from R-CPD that presents in infancy.
My Baby Can’t Burp! This May Explain Why
Babies and older children with this condition are in misery, and so are their parents, with the stress of it all. The answer might be a dysfunction of the upper esophageal sphincter (Retrograde CricoPharyngeus Dysfunction, or R-CPD).
When such babies grow older, those with severe cases of R-CPD may refuse to eat, and may continue to complain of stomach distress.
In this video, Dr. Robert Bastian explains this “new” diagnosis that can cause all of these symptoms. Parents who are exhausted and depressed may find here a glimmer of hope.