Carcinoma
Carcinoma (especially squamous cell carcinoma [SCCA] in the head and neck) is a malignancy originating in the cells that comprise the skin, or that line the respiratory and digestive tracts. SCCA may also be called “epidermoid carcinoma.”
Types of SCCA
SCCA may have subvariants such as spindle cell, verrucous, and papillary forms. The “angriness is described as a degree of differentiation: mildly-, moderately-, or poorly-differentiated.
See also: cancer, carcinoma in situ, and verrucous carcinoma.
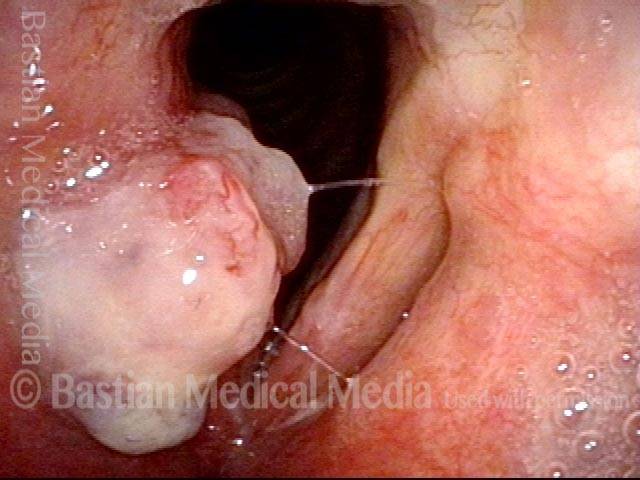
Papillary Squamous Cell Cancer
As in this case, there is sometimes a debate in the mind of the pathologist peering through the microscope, between papillary and verrucous squamous cell carcinoma. The latter (verrucous) form tends to have a pushing margin at the interface with normal tissue, the mitotic rate is low, and there is a cauliflower-like, keratotic surface with clear demarcation between the tumor and normal tissues.
The prognosis for treatment is very good as this is a relatively “lazy” variant of SCCA. Papillary SCCA has features more like garden variety SCCA: the tumor is more infiltrating at the interface with normal tissue and a there is usually a higher mitotic rate. The reader will note strong visual similarity between verrucous SCCA and papillary SCCA, however.
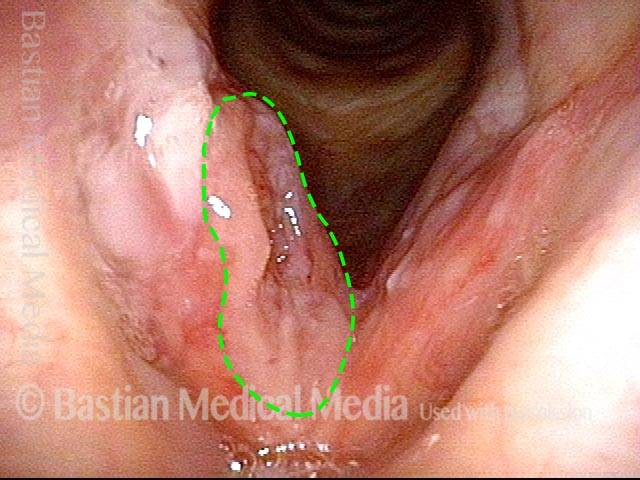
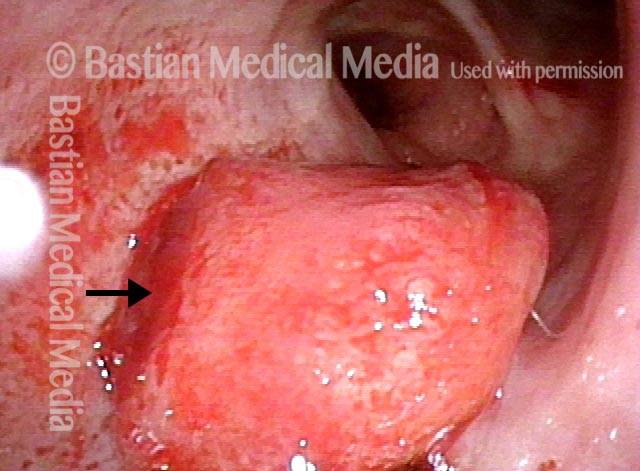
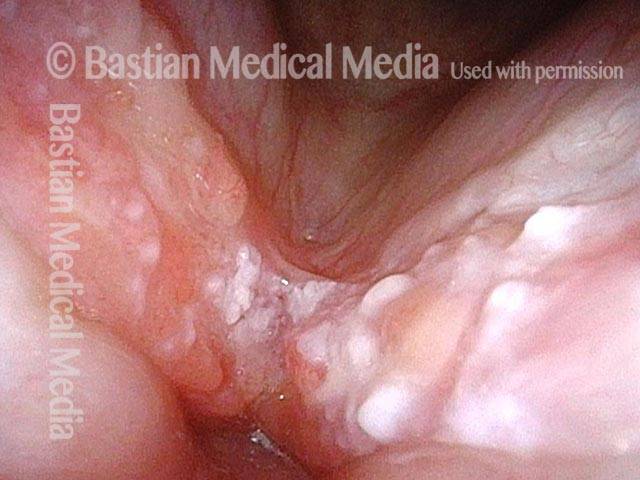
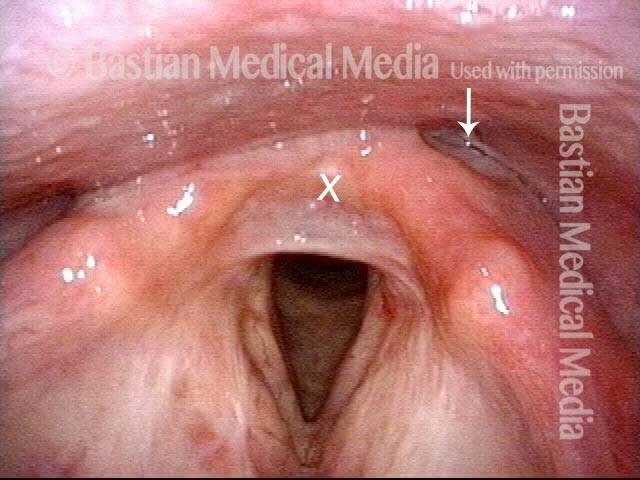
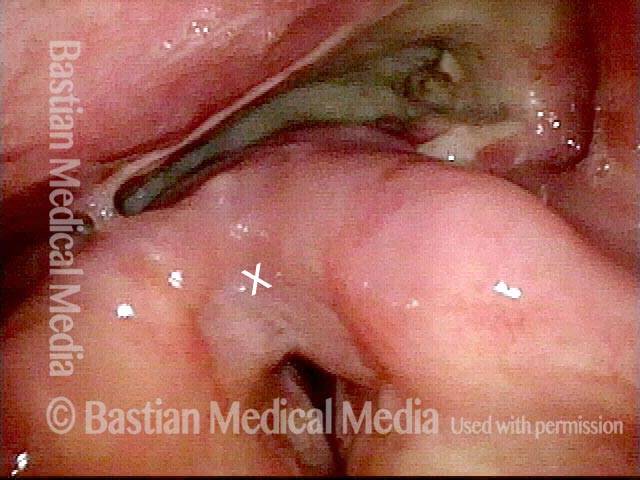
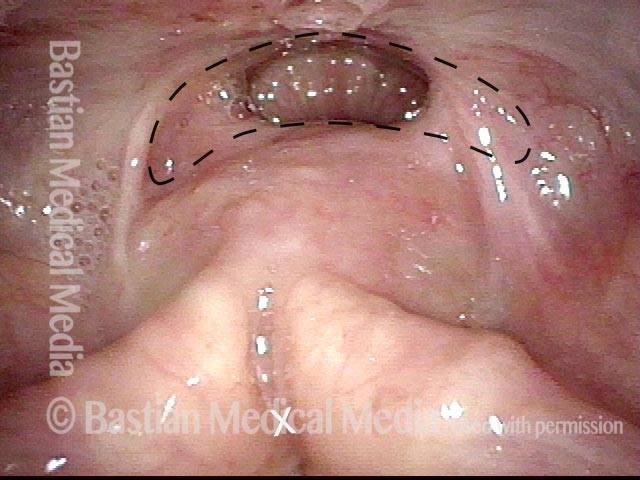
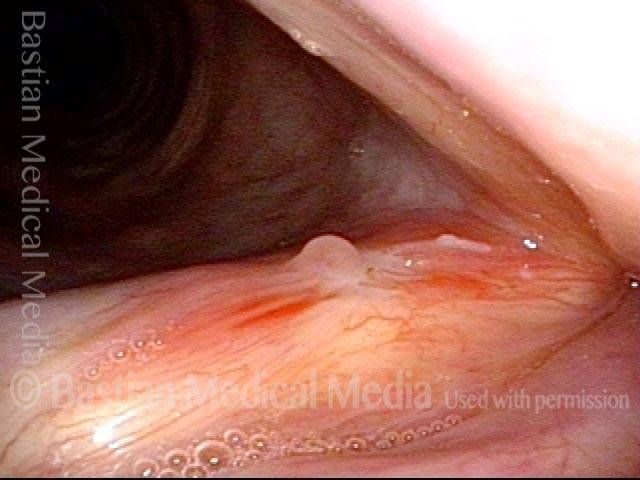
Bulky White Lesion (1 of 17)
Bulky White Lesion (1 of 17)
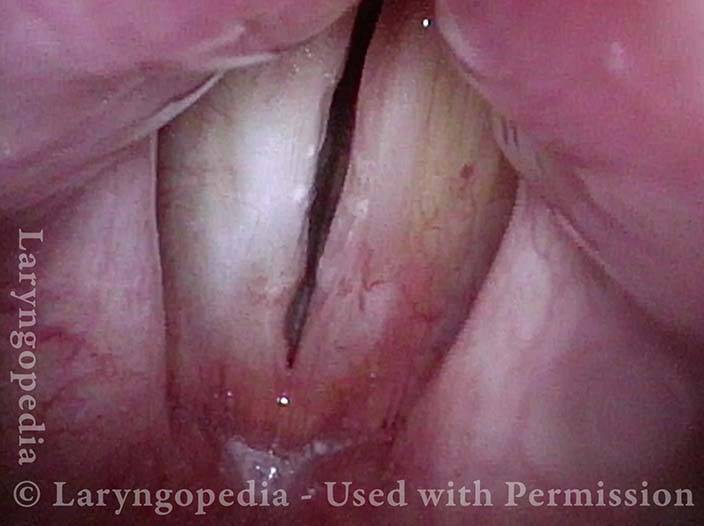
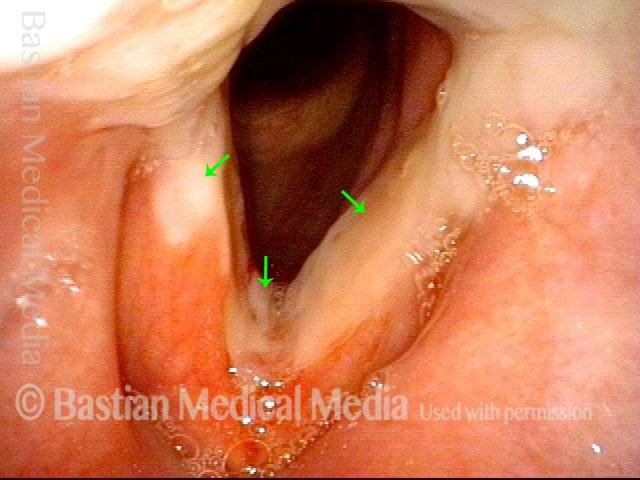
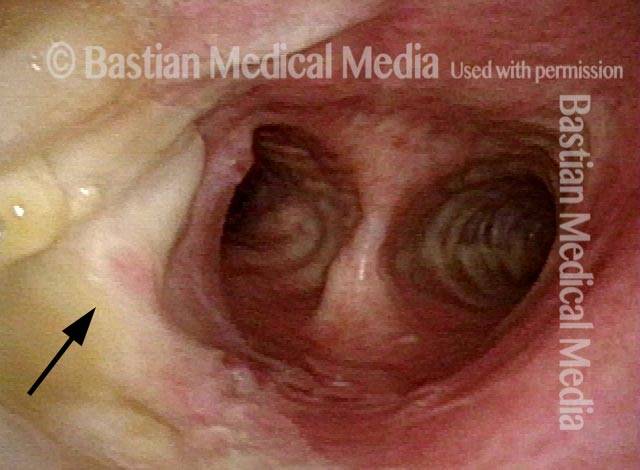
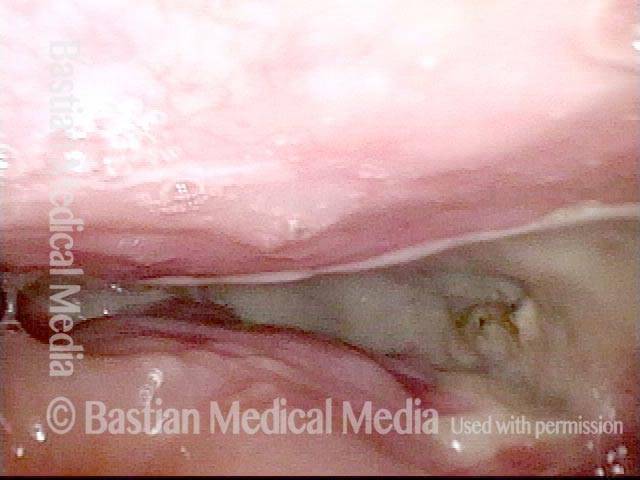
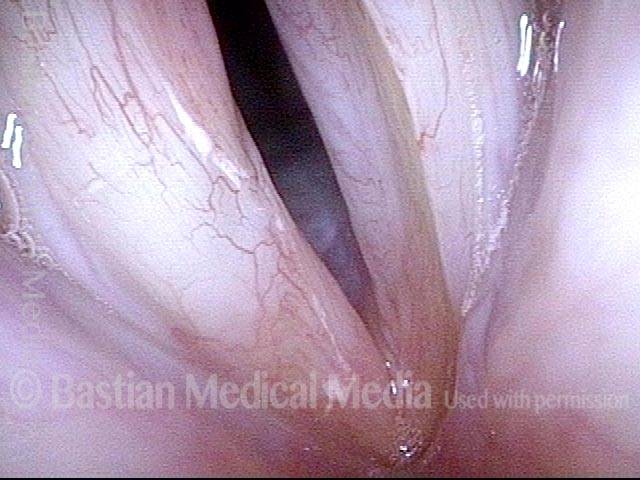
Normal Vocal Cord Movement (2 of 17)
Normal Vocal Cord Movement (2 of 17)
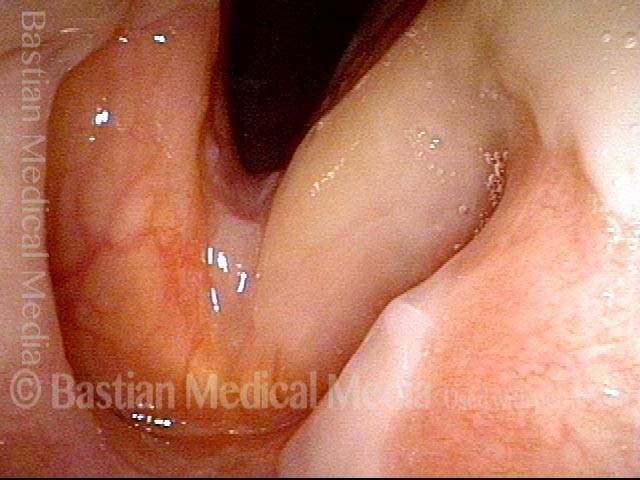
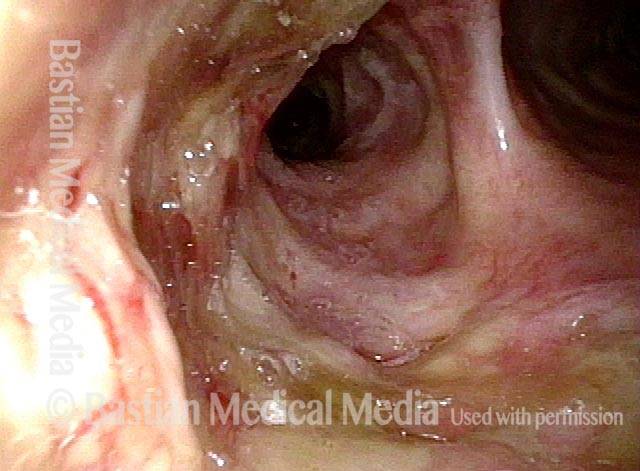
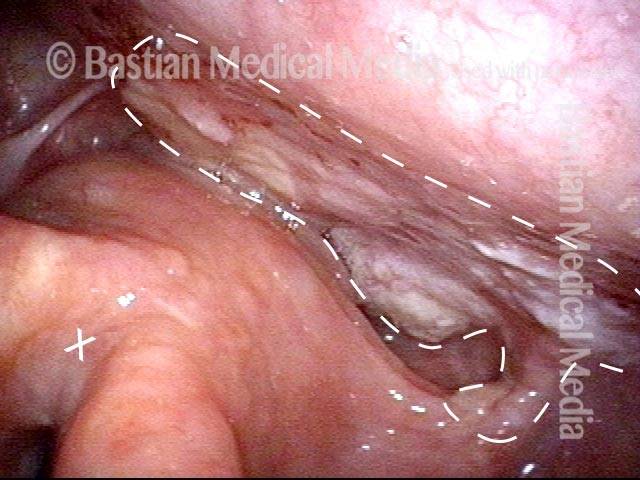
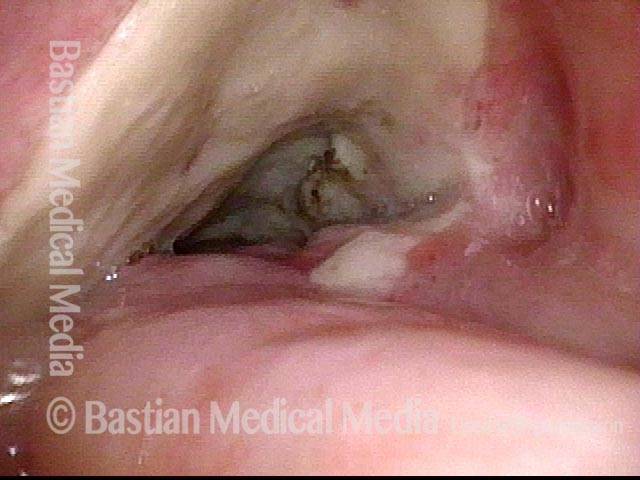
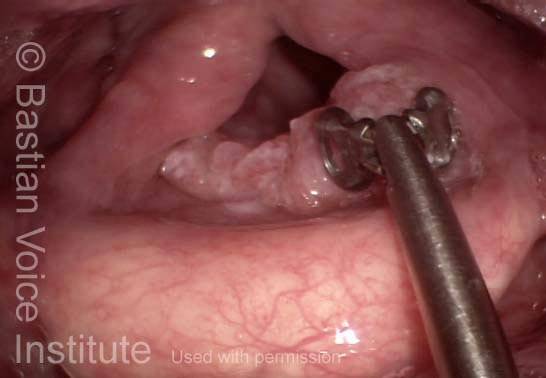
Initial View During Microlaryngoscopy (3 of 17)
Initial View During Microlaryngoscopy (3 of 17)
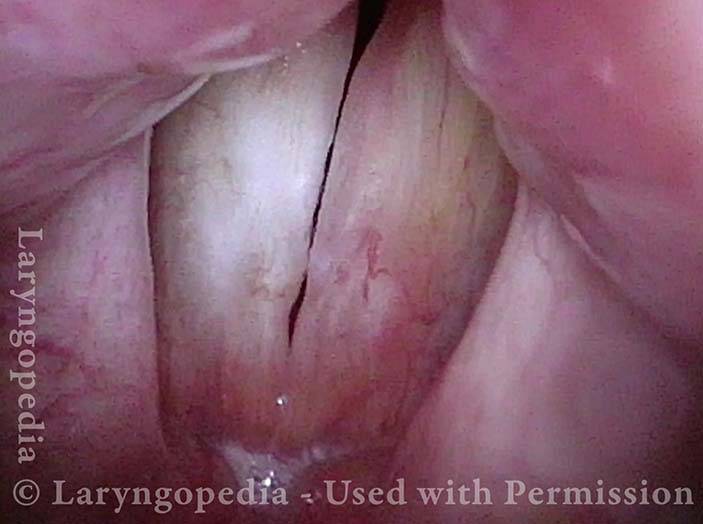
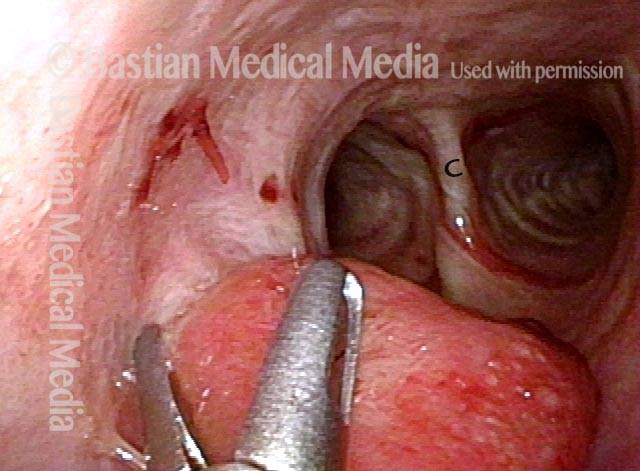
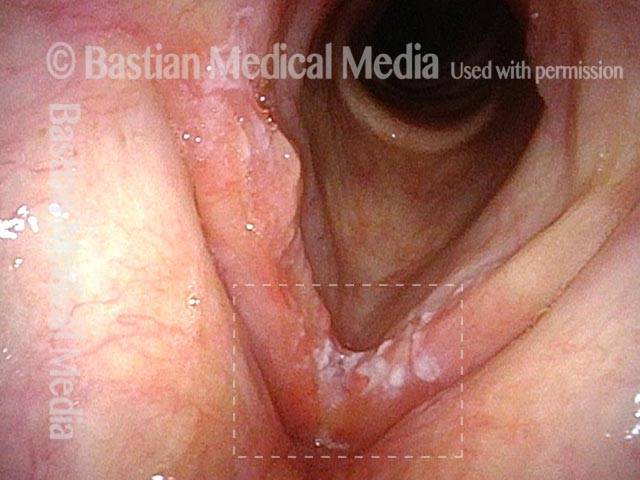
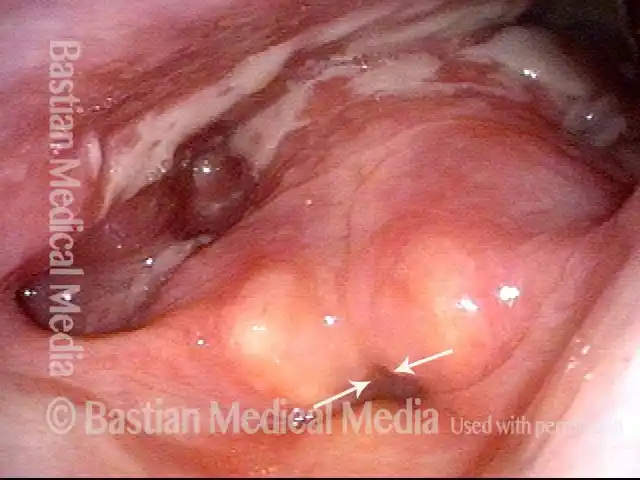
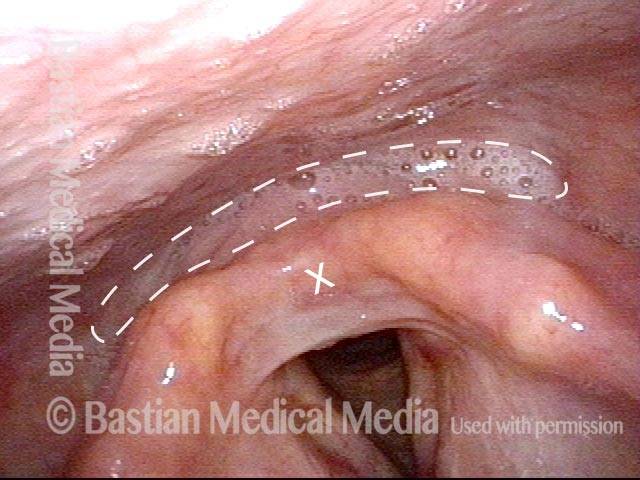
Clear Demarcation from Normal (4 of 17)
Clear Demarcation from Normal (4 of 17)
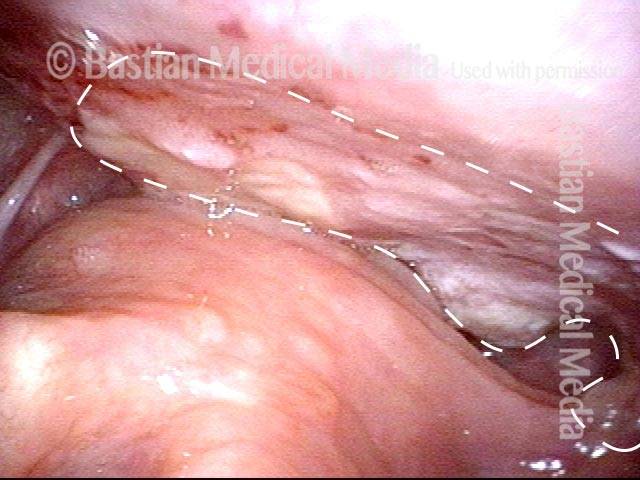
Narrow Margin (5 of 17)
Narrow Margin (5 of 17)
Added Excision (6 of 17)
Added Excision (6 of 17)
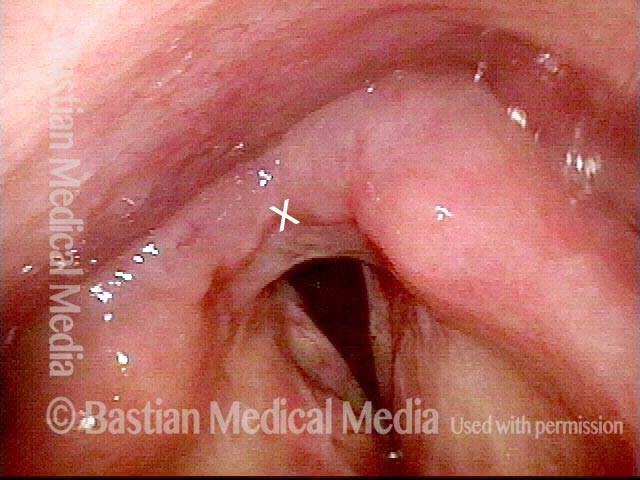
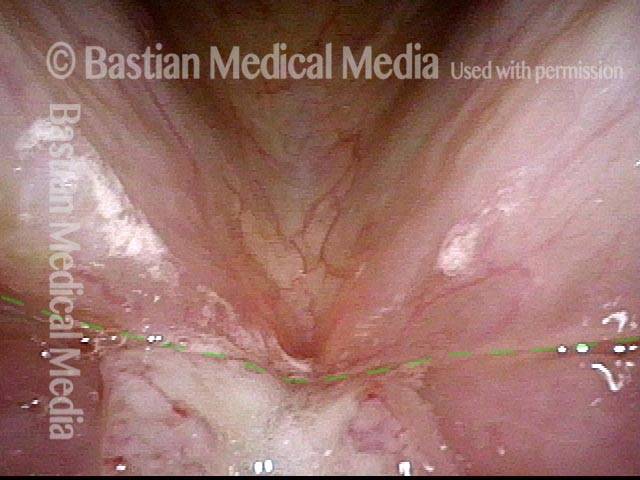
Excision Complete (7 of 17)
Excision Complete (7 of 17)
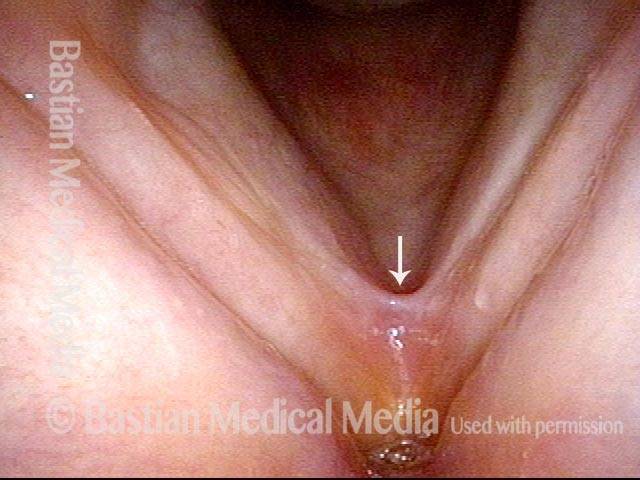
At One Week, Voice Better (8 of 17)
At One Week, Voice Better (8 of 17)
Voice Already Better (9 of 17)
Voice Already Better (9 of 17)
Small recurrence (10 of 17)
Small recurrence (10 of 17)
Vocal Cord Microsurgery (11 of 17)
Vocal Cord Microsurgery (11 of 17)
Excision in progress (12 of 17)
Excision in progress (12 of 17)
Post-surgical divot (13 of 17)
Post-surgical divot (13 of 17)
Voice is still good (14 of 17)
Voice is still good (14 of 17)
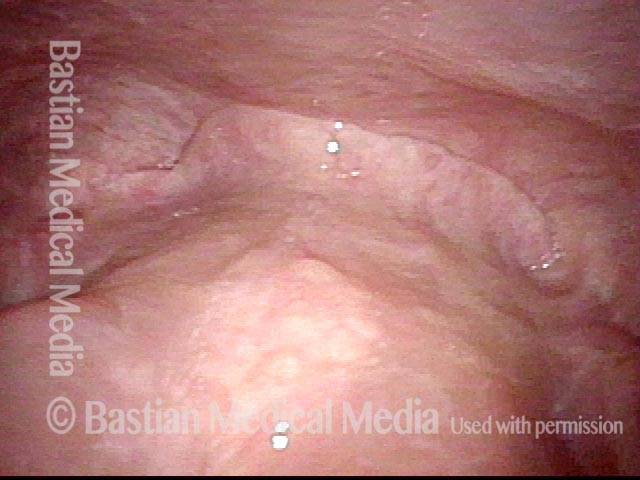
No recurrence 7 years later (15 of 17)
No recurrence 7 years later (15 of 17)
Strobe light view (16 of 17)
Strobe light view (16 of 17)
Good match (17 of 17)
Good match (17 of 17)
Radiation Mucositis
Prior to start of radiation (1 of 4)
Prior to start of radiation (1 of 4)
Radiation mucositis, 1 week after radiation (2 of 4)
Radiation mucositis, 1 week after radiation (2 of 4)
Radiation mucositis, 4 weeks after radiation (3 of 4)
Radiation mucositis, 4 weeks after radiation (3 of 4)
Disappearing radiation mucositis, 10 weeks after radiation (4 of 4)
Disappearing radiation mucositis, 10 weeks after radiation (4 of 4)
Laser Surgery for Bilateral Vocal Cord Cancer
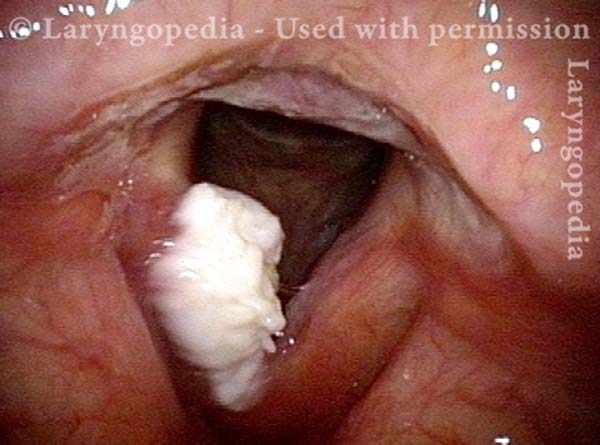
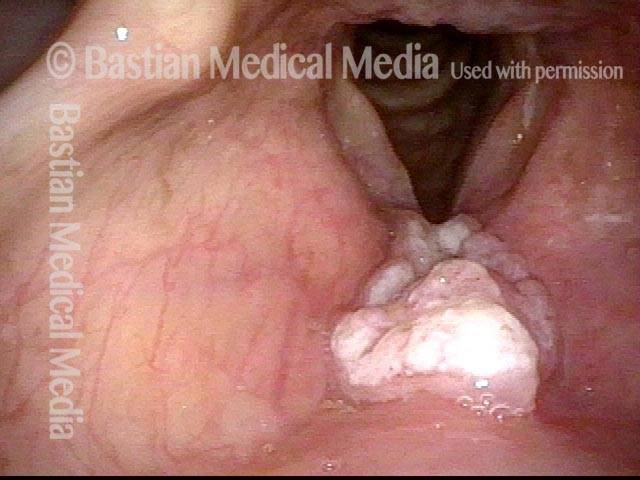
Squamous cell carcinoma (1 of 6)
Squamous cell carcinoma (1 of 6)
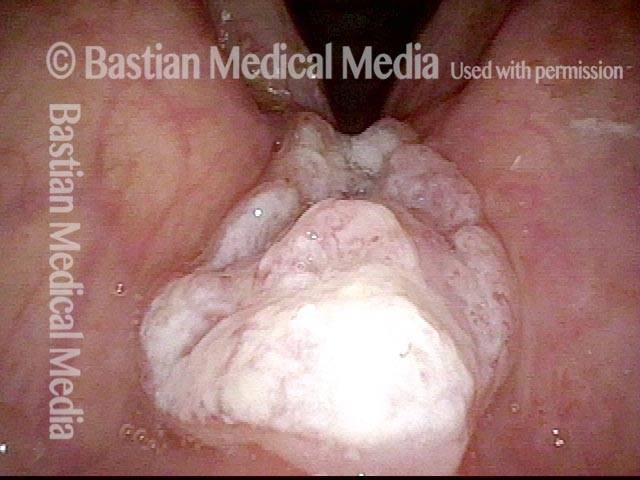
Tumor on the vocal cords (2 of 6)
Tumor on the vocal cords (2 of 6)
Granuloma delays voice recovery (3 of 6)
Granuloma delays voice recovery (3 of 6)
Closer view of granuloma (4 of 6)
Closer view of granuloma (4 of 6)
Granuloma is smaller (5 of 6)
Granuloma is smaller (5 of 6)
Granuloma doesn’t impede voice (6 of 6)
Granuloma doesn’t impede voice (6 of 6)
Tumor in Trachea
Biopsy (1 of 4)
Biopsy (1 of 4)
After biopsy (2 of 4)
After biopsy (2 of 4)
Tumor gone (3 of 4)
Tumor gone (3 of 4)
Slow return (4 of 4)
Slow return (4 of 4)
Vocal Cord Cancer, before, during, and after Radiation
Vocal cord cancer (1 of 8)
Vocal cord cancer (1 of 8)
Vocal cord cancer (2 of 8)
Vocal cord cancer (2 of 8)
Vocal cord cancer, during radiation (3 of 8)
Vocal cord cancer, during radiation (3 of 8)
Vocal cord cancer, during radiation (4 of 8)
Vocal cord cancer, during radiation (4 of 8)
Vocal cord cancer, 2 months after radiation (5 of 8)
Vocal cord cancer, 2 months after radiation (5 of 8)
Vocal cord cancer, 4 months after radiation (6 of 8)
Vocal cord cancer, 4 months after radiation (6 of 8)
Vocal cord cancer, 6 months after radiation (7 of 8)
Vocal cord cancer, 6 months after radiation (7 of 8)
Vocal cord cancer, 6 months after radiation (8 of 8)
Vocal cord cancer, 6 months after radiation (8 of 8)
Hypopharyngeal Cancer, before and after Surgery
Hypopharyngeal cancer (1 of 10)
Hypopharyngeal cancer (1 of 10)
Hypopharyngeal cancer (2 of 10)
Hypopharyngeal cancer (2 of 10)
Hypopharyngeal cancer (3 of 10)
Hypopharyngeal cancer (3 of 10)
Hypopharyngeal cancer (4 of 10)
Hypopharyngeal cancer (4 of 10)
Hypopharyngeal cancer: 1 week after surgery (5 of 10)
Hypopharyngeal cancer: 1 week after surgery (5 of 10)
Hypopharyngeal cancer: 1 week after surgery (6 of 10)
Hypopharyngeal cancer: 1 week after surgery (6 of 10)
Hypopharyngeal cancer: 1 week after surgery (7 of 10)
Hypopharyngeal cancer: 1 week after surgery (7 of 10)
Hypopharyngeal cancer: 1 week after surgery (8 of 10)
Hypopharyngeal cancer: 1 week after surgery (8 of 10)
Hypopharyngeal cancer: several months after surgery (9 of 10)
Hypopharyngeal cancer: several months after surgery (9 of 10)
Hypopharyngeal cancer: several months after surgery (10 of 10)
Hypopharyngeal cancer: several months after surgery (10 of 10)
Supraglottic Cancer
Supraglottic cancer (1 of 4)
Supraglottic cancer (1 of 4)
Supraglottic cancer (2 of 4)
Supraglottic cancer (2 of 4)
Supraglottic cancer (3 of 4)
Supraglottic cancer (3 of 4)
Supraglottic cancer (4 of 4)
Supraglottic cancer (4 of 4)
Vocal Cord Cancer, before and after Surgery
Vocal cord cancer (1 of 4)
Vocal cord cancer (1 of 4)
Vocal cord cancer, 1 week after surgery (2 of 4)
Vocal cord cancer, 1 week after surgery (2 of 4)
Vocal cord cancer, 1 month after surgery (3 of 4)
Vocal cord cancer, 1 month after surgery (3 of 4)
Vocal cord cancer, after complete healing (4 of 4)
Vocal cord cancer, after complete healing (4 of 4)
Biopsy of Carcinoma
Biopsy, epiglottis (1 of 1)
Biopsy, epiglottis (1 of 1)
Glottic Cancer, Laser Removal
Glottic cancer, laser removal (1 of 3)
Glottic cancer, laser removal (1 of 3)
Glottic cancer, laser removal (2 of 3)
Glottic cancer, laser removal (2 of 3)
Glottic cancer, laser removal (3 of 3)
Glottic cancer, laser removal (3 of 3)
Share this article