What Hospital Staff Need to Know About You As a Laryngectomy Patient (Especially if Contemplating Surgery)
Introduction
Anesthesiologists, respiratory therapists, and nurses may know the following information if you are in a large hospital. If you are in a small hospital, day surgery center, walk-in urgent care facility, etc., the clinical staff may be unfamiliar with the following information.
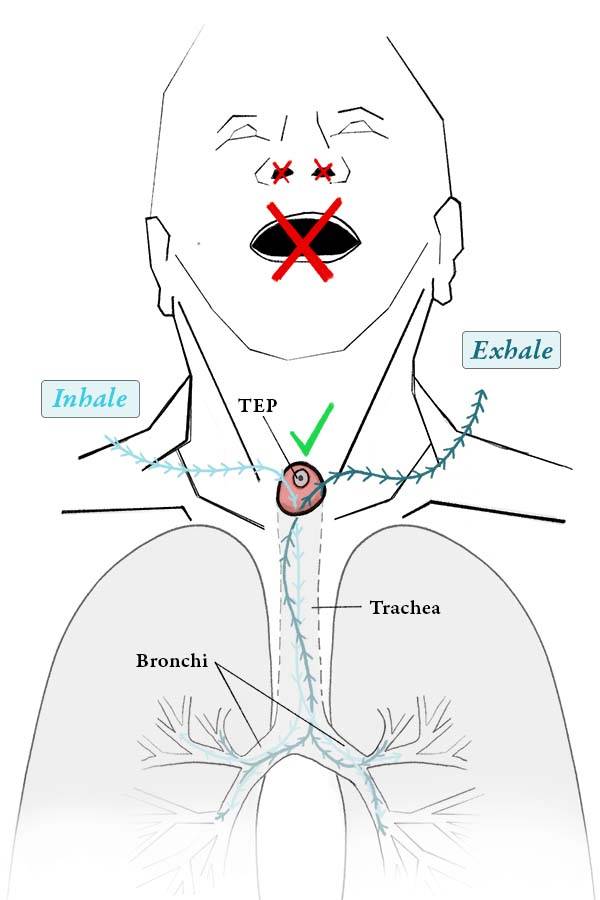
Understanding your new anatomy
Managing your airway is very straightforward as the entrance to the airway is immediately accessible at the base of the neck. See Figure 1. You cannot get to the airway through the nose or mouth. In other words, you are an obligatory neck breather. Hence, all interventions having to do with airway—whether that is intubation, suctioning, administration of medication such as for bronchospasm, or administration of oxygen—must all be done through the stoma at the base of the neck. A facemask for the purpose of administering oxygen, inhaled medication, or humidity will not work.
Mechanical ventilation for TEP patients
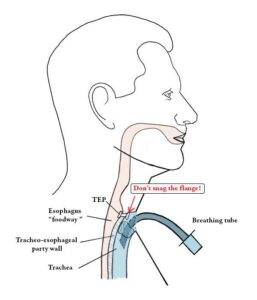
If you need to be ventilated mechanically (such as during surgery or in an ICU), the only two methods are to insert a small breathing tube (but only a few centimeters!). See Figure 2. Or, on a short-term basis, a pediatric facemask will usually make a nice seal over the stoma, such as during induction of anesthesia.
Patients with Tracheo-esophageal Voice
If you use tracheo-esophageal voice (and not an “electrolarynx”), you will see within the stoma a small circular plastic device. This is called the tracheoesophageal prosthesis (TEP) and is utilized for tracheoesophageal prosthetic voice. Upon induction of anesthesia, the endotracheal tube should pass this plastic device without any difficulty. Just take extra precaution not to catch the edge of the prosthesis (flange) with the breathing tube. See Figure 2.
Post-anesthesia care
At the conclusion of anesthesia, after the endotracheal tube is withdrawn, it is critical to verify visually that the prosthetic device remains in site, and that its position has not changed (other than rotation) as compared with the beginning of the case. See Figure 1.
What to do if your TEP is dislodged?
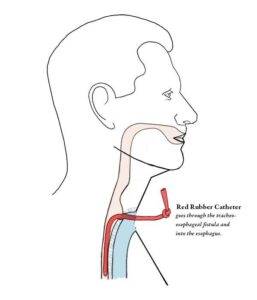
If, for any reason, the tracheoesophageal prosthesis is dislodged (no longer seen at the conclusion of the procedure), there must be an effort to locate it, including searching bedclothes and if necessary, taking of a chest x-ray if it is not found otherwise. Furthermore, this situation requires semi-urgent attention from an otolaryngologist or speech pathologist familiar with tracheoesophageal puncture voice.
There is no threat to your life, but a red rubber catheter should be inserted into the TEP site and into the esophagus beyond as a “placeholder,” until a new tracheoesophageal voice prosthesis can be placed. See Figure 3. Otherwise, the passage can close rapidly, necessitating a surgical procedure to recreate it, and of course you would be unable to swallow liquids without their entering your trachea.
Share this article