Injection Laryngoplasty
Injection laryngoplasty is a procedure during which the vocal cord is injected (filled) with an implant material. The most common reason for this is a paralyzed vocal cord, but it might also be used for severe vocal cord bowing unresponsive to voice building. There are also other diagnoses such as atrophy or tissue loss. In each of these diagnoses, the patient is motivated by a weak, air-wasting (breathy or diplophonic) voice quality that is highly limiting to his or her ability to communicate.
Materials available for injection are: a temporary gel (various brands); a semi-permanent calcium hydroxyapatite paste; micronized human collagen (Cymetra™); the patient’s own fat, usually harvested from around the umbilicus; or in an earlier era, Teflon™ paste.
The particular material used usually depends upon whether temporary or more permanent voice strengthening is needed.
Two-Fold Purpose of Injection Laryngoplasty
First, to fatten the cord and shift its static position toward the midline so that the other (mobile) vocal cord can “reach it.” The second reason is to fortify the tissue so that the deficient cord is less flaccid and can “stand up” to the air pressure below and passing between the two cords when they are positioned together to create voice.
3 Injection Methods
- With the help of extensive topical anestheisa, in an “office” videoendoscopy room, using a curved cannula inserted through the mouth, over the back of the tongue, and down into the cord through its upper surface.
- In an “office” videoendoscopy room, injecting through the anterior neck while viewing the vocal cords video-endoscopically on a monitor screen.
- In an outpatient operating room and during brief general anesthesia, viewing through a laryngoscope placed through the mouth to visualize the vocal cords, and injecting in a straight line through the upper surface of the vocal cord(s).
Which Method Should I Use?
It depends on surgeon and patient preference, as well as the circumstance. For example, a medically-fragile patient might be best done under topical anesthesia in an “enhanced office” setting. A person having more permanent material injected, and certainly if it is to be bilateral, may need exquisite symmetry of injection more suitably done under brief general anesthesia.
Photo Examples
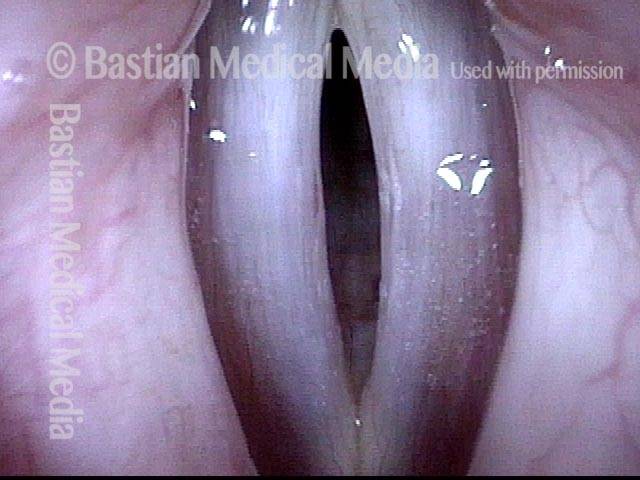
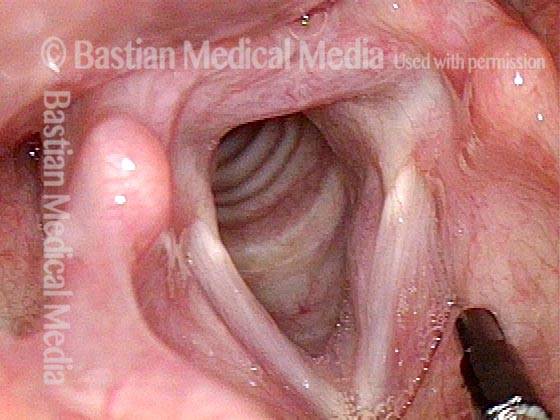
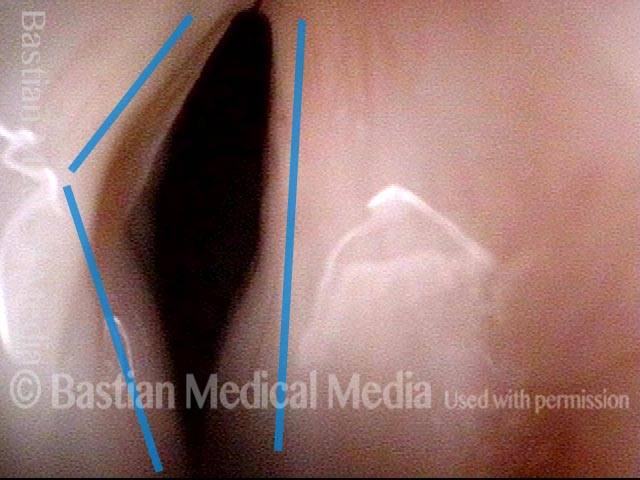
Vocal cord paralysis (1 of 7)
Vocal cord paralysis (1 of 7)
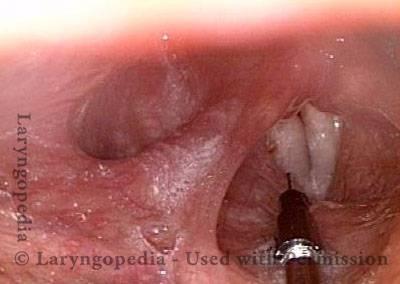
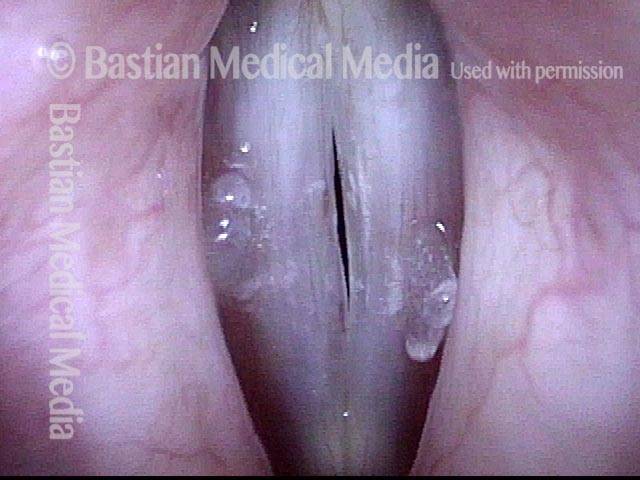
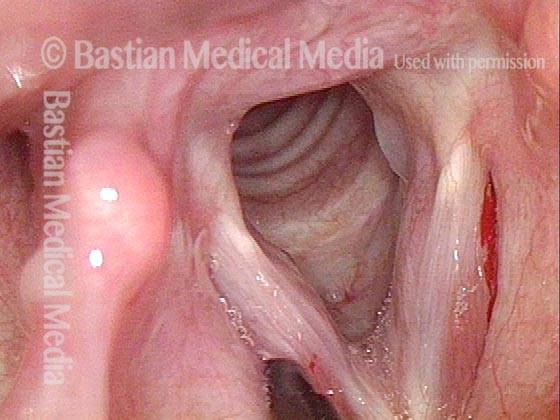
Voice gel injection (2 of 7)
Voice gel injection (2 of 7)
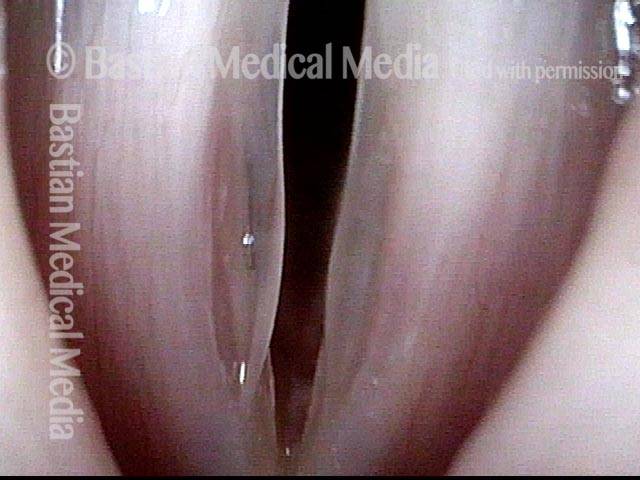
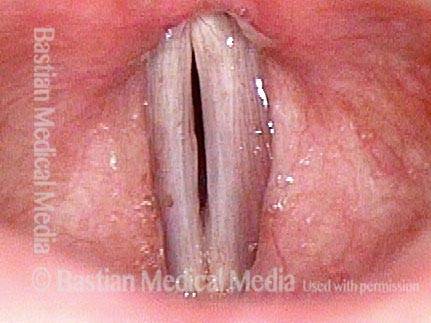
Success (3 of 7)
Success (3 of 7)
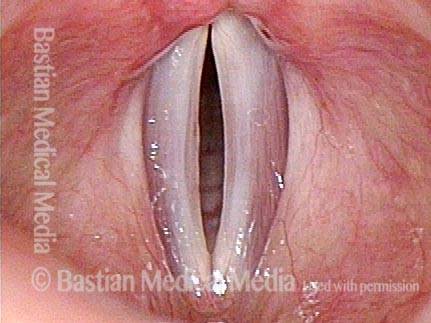
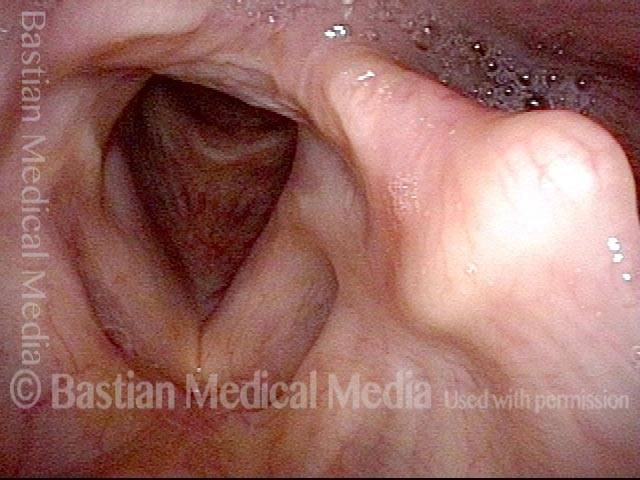
Plump right vocal cord (4 of 7)
Plump right vocal cord (4 of 7)
Posterior gap (5 of 7)
Posterior gap (5 of 7)
PCA Weakness (6 of 7)
PCA Weakness (6 of 7)
LCA muscle recovered (7 of 7)
LCA muscle recovered (7 of 7)
Example 2
Paresis, TA + LCA (1 of 5)
Paresis, TA + LCA (1 of 5)
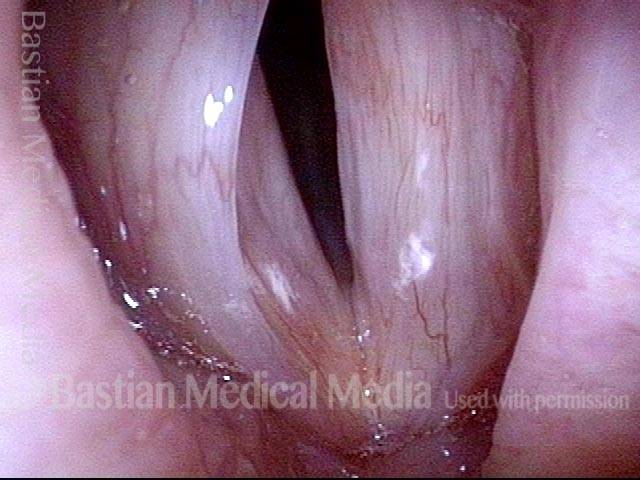
Paresis, TA + LCA (2 of 5)
Paresis, TA + LCA (2 of 5)
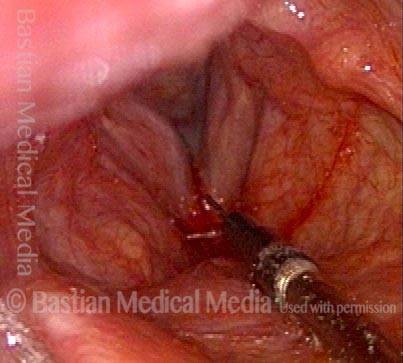
Voice gel injection (3 of 5)
Voice gel injection (3 of 5)
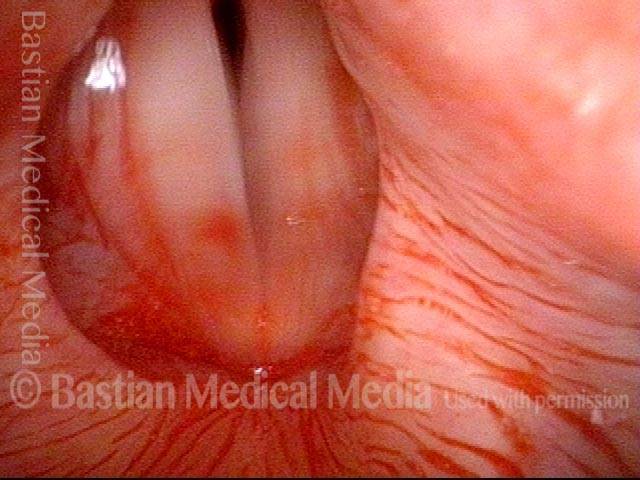
1 month after injection (4 of 5)
1 month after injection (4 of 5)
Phonation 1 month after injection (5 of 5)
Phonation 1 month after injection (5 of 5)
Injection Laryngoplasty with Temporary Gel
Laryngoplasty (1 of 4)
Laryngoplasty (1 of 4)
Reason for air-wasting (2 of 4)
Reason for air-wasting (2 of 4)
Voice gel injected into vocal cord (3 of 4)
Voice gel injected into vocal cord (3 of 4)
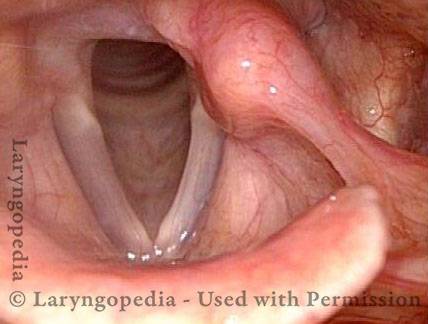
Vocal cords close completely (4 of 4)
Vocal cords close completely (4 of 4)
Congenital Glottic Sulcus & Bowing, before and after Injection
Glottic sulcus (1 of 10)
Glottic sulcus (1 of 10)
Glottic sulcus (2 of 10)
Glottic sulcus (2 of 10)
Glottic sulcus (3 of 10)
Glottic sulcus (3 of 10)
Glottic sulcus (4 of 10)
Glottic sulcus (4 of 10)
Sulcus with bowing, just prior to injection (5 of 10)
Sulcus with bowing, just prior to injection (5 of 10)
Sulcus with bowing, just prior to injection (6 of 10)
Sulcus with bowing, just prior to injection (6 of 10)
Voice gel injection (7 of 10)
Voice gel injection (7 of 10)
Voice gel injection (8 of 10)
Voice gel injection (8 of 10)
After the injection (9 of 10)
After the injection (9 of 10)
After the injection (10 of 10)
After the injection (10 of 10)
Paresis, TA + LCA, before and after Injection of Voice Gel
Normally functioning PCA muscle (1 of 8)
Normally functioning PCA muscle (1 of 8)
Paresis, TA + LCA (2 of 8)
Paresis, TA + LCA (2 of 8)
Paresis, TA + LCA (3 of 8)
Paresis, TA + LCA (3 of 8)
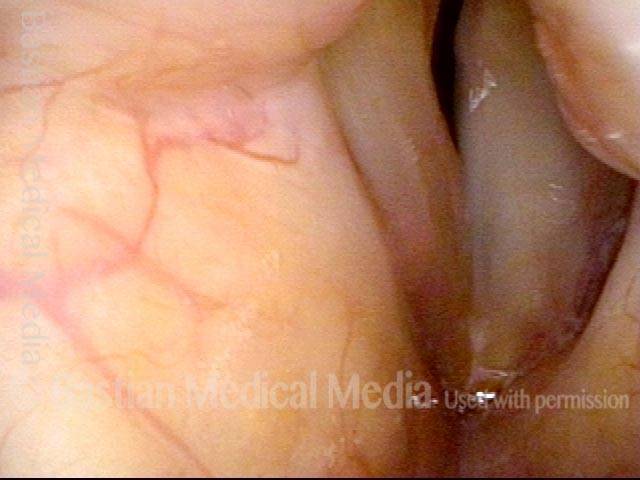
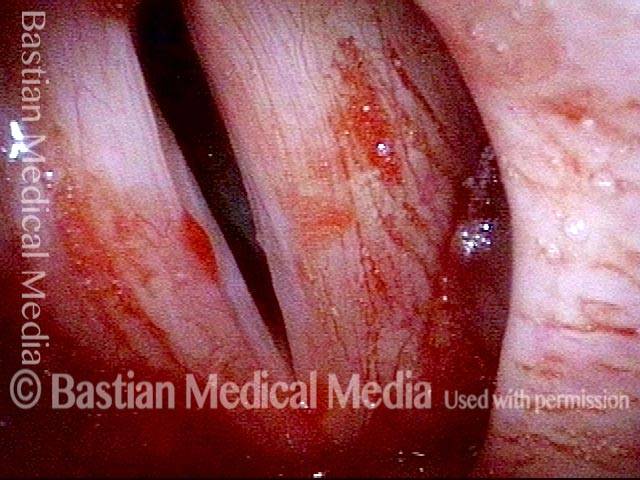
Lateral buckling (4 of 8)
Lateral buckling (4 of 8)
Voice gel injection (5 of 8)
Voice gel injection (5 of 8)
After voice gel injection (6 of 8)
After voice gel injection (6 of 8)
After injection (7 of 8)
After injection (7 of 8)
Strobe light after injection (8 of 8)
Strobe light after injection (8 of 8)
Share this article