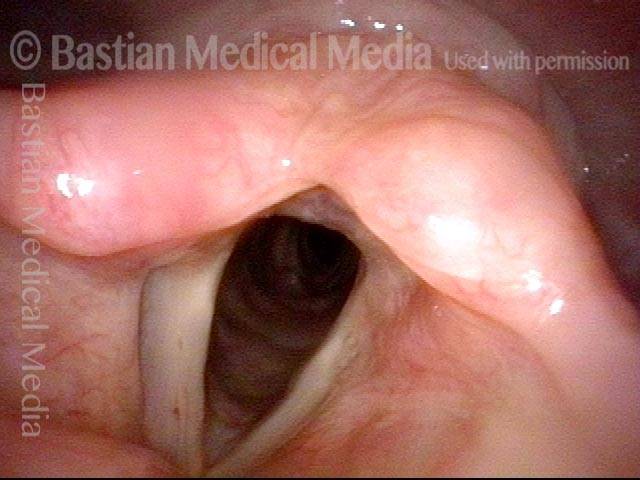
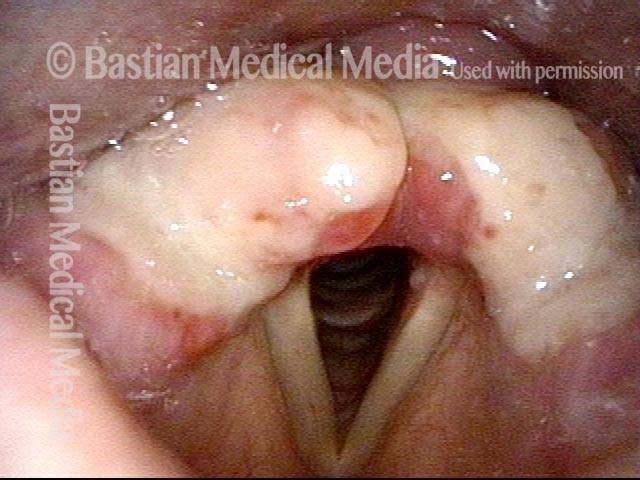
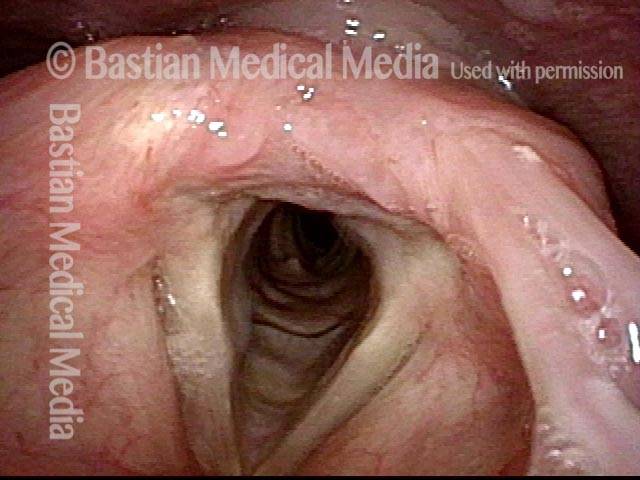
Redundant supraglottic mucosa is an excess of mucosa overlying one or more structures in the larynx above the vocal cords. Mucosa in this area should “fit” snugly, like leggings, but in the case of redundant supraglottic mucosa, the fit becomes more like baggy pants.
Symptoms and Treatment
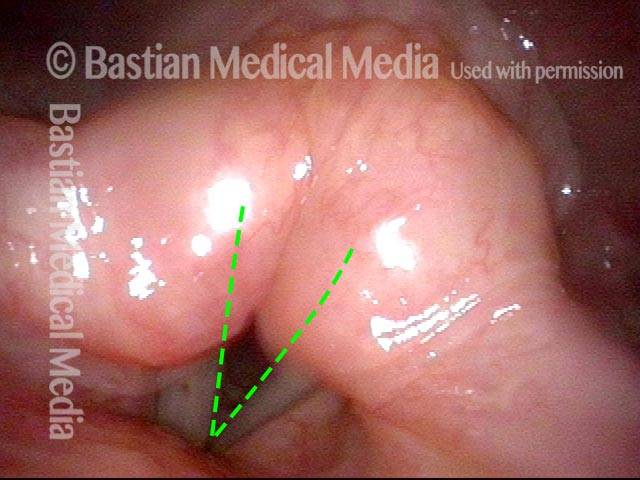
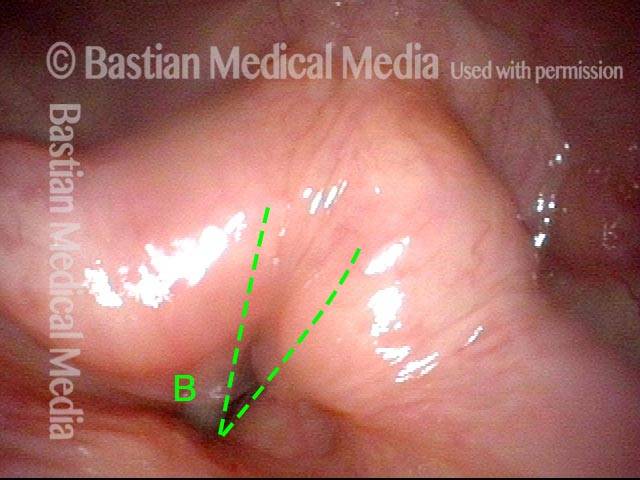
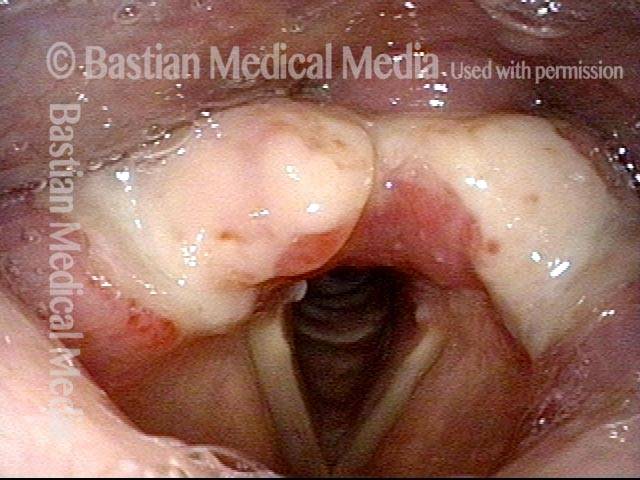
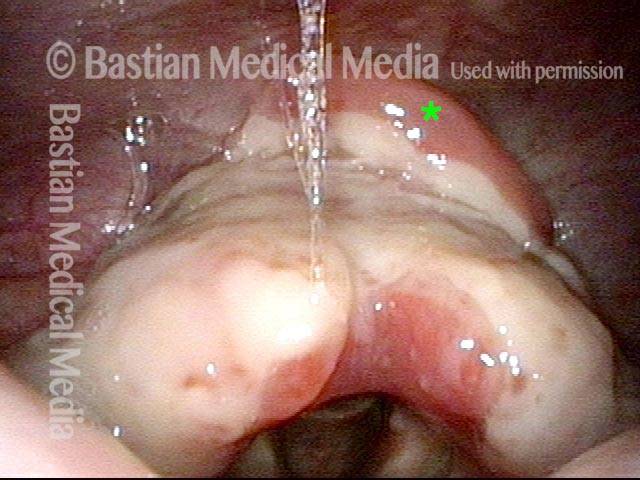
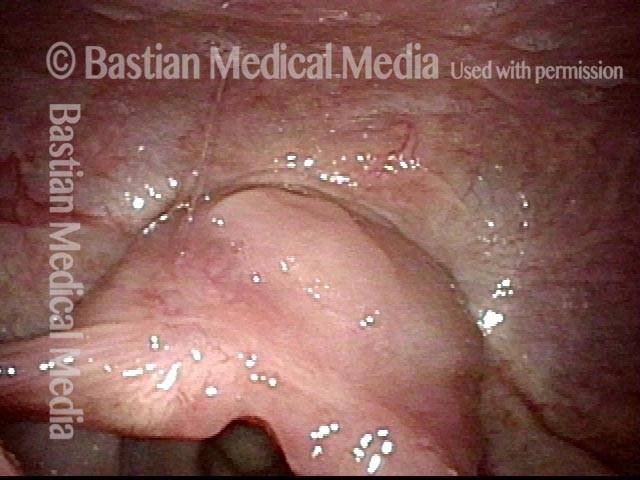
This redundant supraglottic mucosa most commonly develops on the apex and posterior surface of the arytenoid cartilage. Such mucosa sometimes draws inward during breathing and fills the laryngeal vestibule. In a severe case, inspiration can become noisy (stridor) or even effortful. When symptoms like these become troublesome, the excess mucosal tissue can be removed with endoscopic laser surgery.
Redundant Supraglottic Mucosa vs. Laryngomalacia
It is similar to the disorder laryngomalacia. In both disorders, supraglottic tissue is pulled into the laryngeal vestibule during breathing and can cause stridor. However, the causes of these symptoms are different. In the case of redundant supraglottic mucosa, the main problem is an excess of overlying mucosa, but in the case of laryngomalacia, the main problem is that the underlying structural tissue, such as that which comprises the aryepiglottic cord and epiglottic cartilage, is abnormally weak or soft.