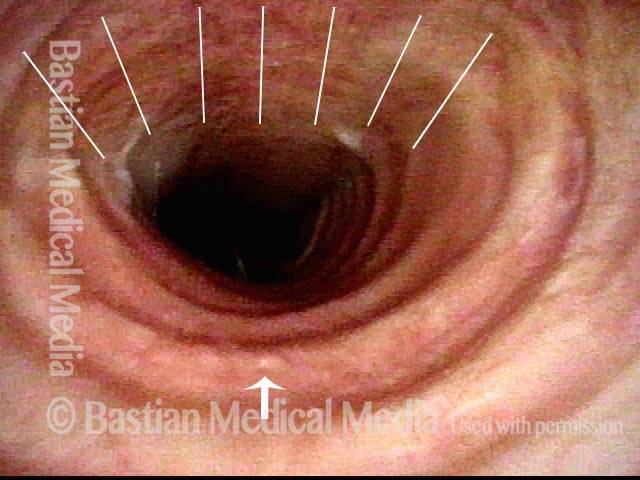
Tracheomalacia is the flaccidity of the trachea, due to injury or congenital defect, such that the tracheal passageway fails to stay open at its normal diameter, especially during inspiration. In adults, it is most commonly seen after a prolonged intubation in which the endotracheal tube balloon was (sometimes necessarily) over-inflated and, consequently, exerted too much pressure on the tracheal rings, damaging and thereby weakening them; infection can also exacerbate this weakening of the tracheal rings. Intubation is a less common cause of tracheomalacia now, however, since the advent years ago of high-volume, low-pressure endotracheal tube and tracheotomy tube cuffs. In neonates, tracheomalacia can be congenital or a sign of incomplete development of the trachea.
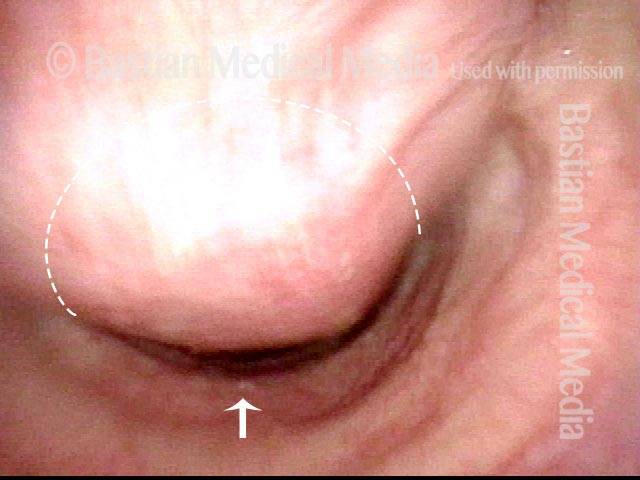
Tracheomalacia should be distinguished from nonorganic breathing disorder, tracheal, where the tracheal collapse which occurs is functional or volitional, and is sometimes used to amplify asthmatic wheezing, or to masquerade as asthma, in each case for secondary gain.