Glottic stenosis refers to scarring in the larynx at the level of the vocal cords (glottis). It usually narrows the space available between the cords for inflow of air to the lungs while breathing. Or it can cause divots in the posterior vocal cords. Examples of possible causes:
-
Congenital Web
A baby can be born with vocal cords fused together due to a developmental defect.
-
Endotracheal (breathing) tube injury
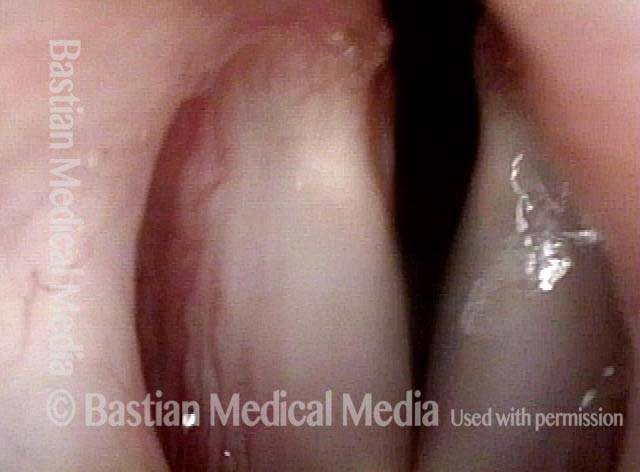
Breathing tubes go through the mouth, down into the larynx, between the vocal cords and into the upper trachea. If a person requires ventilation due to critical illness and the breathing tube sits between the vocal cords for several weeks, then raw surfaces can be created. A scar between the raw surfaces on opposite cords can bind the vocal cords together with insufficient remaining space for easy breathing. Or there can be scarring (ankylosis) of the cricoarytenoid joints.
-
Radiation for Larynx Cancer
When larynx cancer is radiated for cure, occasionally the radiation burns are deep enough to create scarring between the cords, or to progressively fibrose (stiffen) the cricoarytenoid joints. Other causes are gunshot wounds, or swallowed plumber’s lye injury (usually young children).
-
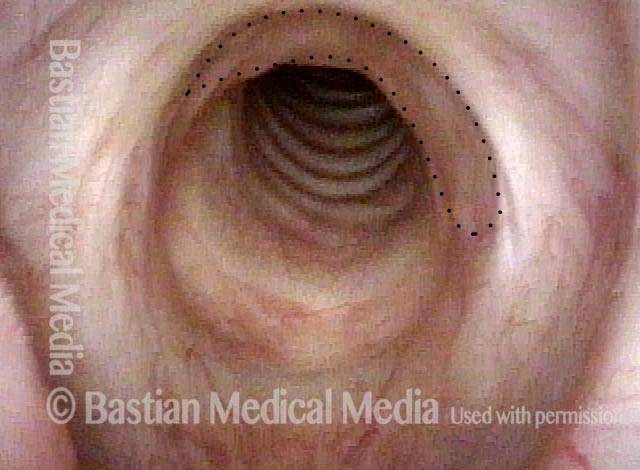
The Effect of Glottic Stenosis
Persons with glottic stenosis describe exercise intolerance and/ or noisy inspiratory breathing (causing involuntary inspiratory phonation or stridor) if the scarring is only the posterior vocal cords. Or if there is scarring of the anterior 2/3 of the cords, voice will also be affected.
Treatment
Treatment options include microsurgical release of scar tissue, with or without steroid injection and topical anti-scarring agents, and occasionally an open reconstruction with grafting.
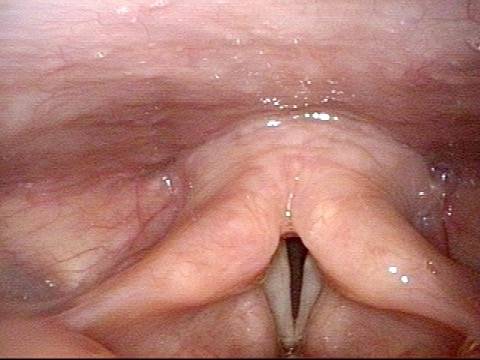
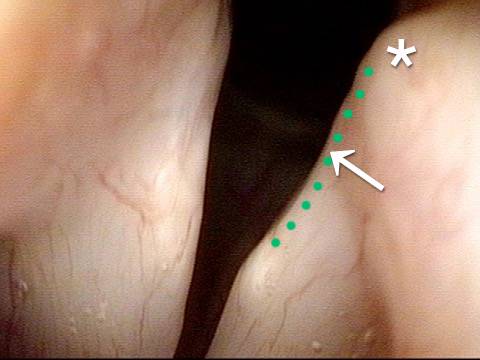
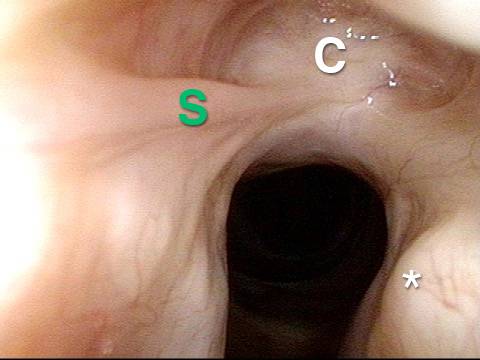
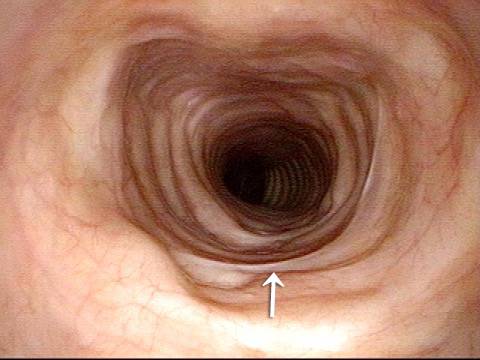
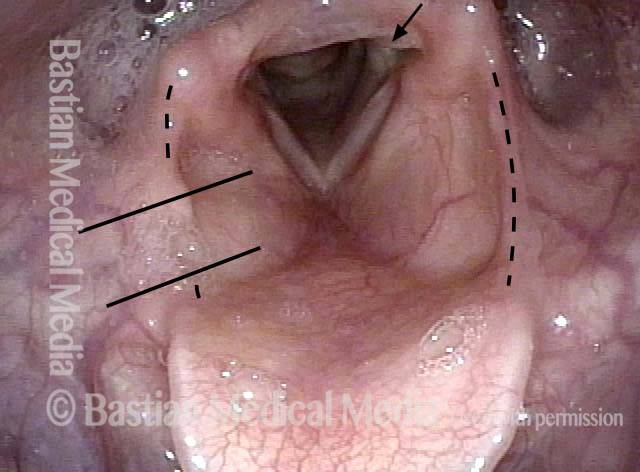
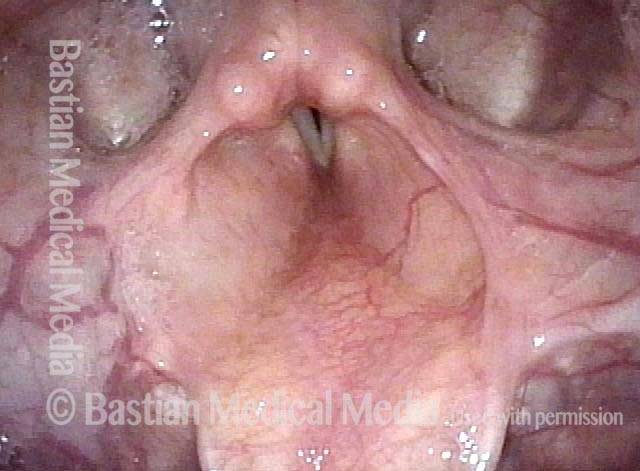
Breathing Tube Injury, not Vocal Cord Paralysis
This middle-aged woman was injured severely in an auto accident as a teenager. Recovery involved a long stay in ICU, and ventilation via a breathing (endotracheal) tube for a few weeks prior to tracheotomy. Fifteen years earlier, a posterior commissuroplasty was done by me on the left side. Severely short of breath before that procedure, she said the improvement was such that she was able to do most activities of daily living remarkably well for many years. While still much better than prior to the posterior commissuroplasty, she has felt a little more limited in the past few years and wants now another similar airway-widening procedure. Speaking voice can easily pass for normal, though she thinks it is occasionally a little rough.