 Studio della deglutizione videoendoscopica (SDVS, VESS)
Studio della deglutizione videoendoscopica (SDVS, VESS)
Metodo per valutare la capacità di deglutizione di una persona mediante un esame fisico documentato tramite video, guardando dall’interno della gola. Chiamata anche valutazione endoscopica a fibre ottiche della deglutizione (FEES). Lo studio videoendoscopico della deglutizione (VESS in inglese) deve essere distinto dallo studio videofluoroscopico della deglutizione (VFSS), che è una valutazione basata sui raggi X.
 Come funziona un SDVS
Come funziona un SDVS
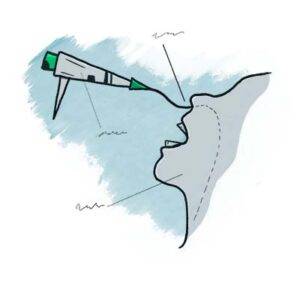
Per eseguire un VESS, un medico utilizza un nasolaringoscopio a fibra ottica o con chip distale. Il medico inizia esaminando la struttura e la funzione del palato, della lingua, della faringe e della laringe del paziente, compresa la sensibilità, se lo si desidera. Successivamente, per valutare le capacità e i limiti di deglutizione del paziente, il medico posiziona la punta del nasolaringoscopio appena sotto il rinofaringe e, guardando verso la gola, chiede al paziente di deglutire una serie di sostanze colorate con una gamma di consistenze (ad esempio, blu -acqua macchiata, salsa di mele macchiata di blu e cracker color arancione).
Mentre il paziente ingerisce queste sostanze, il medico osserva se rimangono o riappaiono tracce significative nello spazio sopra, intorno o all’interno della laringe, anziché scomparire nell’ingresso dell’esofago. Se rimangono tracce significative o se del materiale si riversa nell’apertura della laringe o nella trachea, il paziente può soffrire di presbifagia. Se inizialmente scompaiono tracce significative ma poi riemergono verso l’alto dall’ingresso esofageo, il paziente può avere una disfunzione cricofaringea, con o senza diverticolo di Zenker.
 Benefici dello studio della deglutizione videoendoscopica
Benefici dello studio della deglutizione videoendoscopica
This method has particular value for patients who are bedfast and cannot travel to the radiology suite, or for patients whose swallowing function is rapidly evolving (improving, usually), such as those recovering from a mild stroke. For clinicians experienced with this technique, VESS can also often be used with new patients complaining of dysphagia during the initial consultation as a robust and—depending on patient history—potentially stand-alone method of diagnosis and management.
Sometimes, the VESS findings, along with a patient history of solid food lodgment at the level of the cricoid cartilage or cricopharyngeus muscle, will indicate when VFSS should also be obtained to assess for possible cricopharyngeal dysfunction. Even in this latter circumstance, when VFSS is called upon to confirm a suspected diagnosis, VESS will have already oriented the examiner to the nature and severity of the problem. In most follow-up circumstances other than after cricopharyngeal myotomy, VESS is generally more efficient and inexpensive than VFSS.
SDVS valuta l’attrezzatura, le secrezioni e quindi la capacità di deglutizione
Part Ia: Palate elevates normally (1 of 7)
Part Ia: Palate elevates normally (1 of 7)
Part Ib: phonation (2 of 7)
Part Ib: phonation (2 of 7)
Part Ic: High pitch elicited (3 of 7)
Part Ic: High pitch elicited (3 of 7)
Part IIa: applesauce (4 of 7)
Part IIa: applesauce (4 of 7)
Part IIb: cracker (5 of 7)
Part IIb: cracker (5 of 7)
Part IIb: continued (6 of 7)
Part IIb: continued (6 of 7)
Part IIc: water (7 of 7)
Part IIc: water (7 of 7)
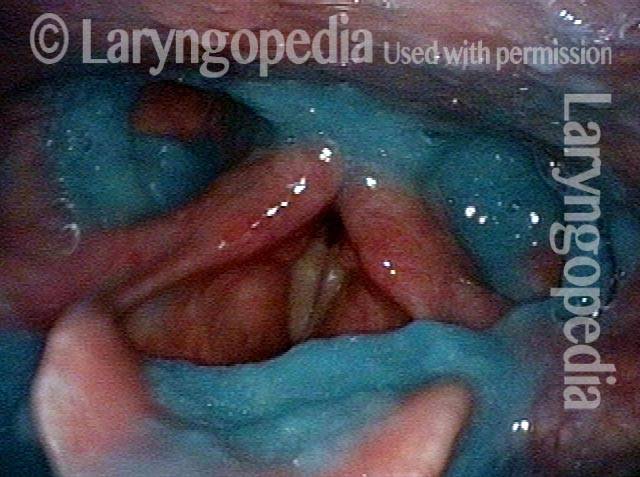
Disfagia/Riflesso ritardato della deglutizione
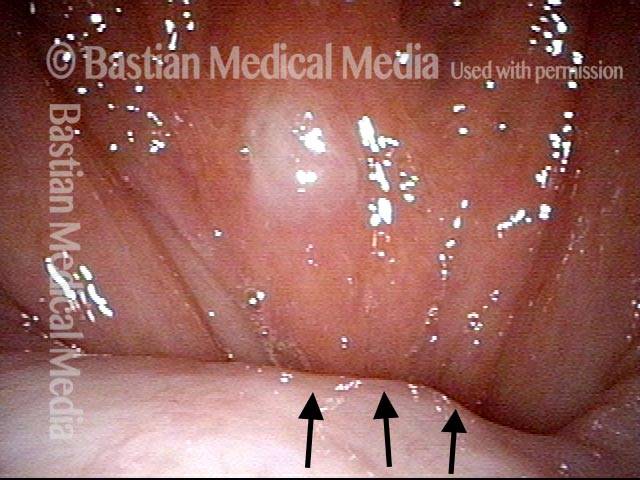
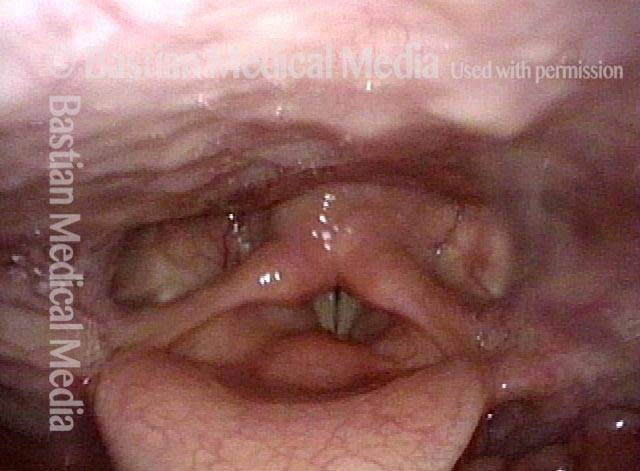
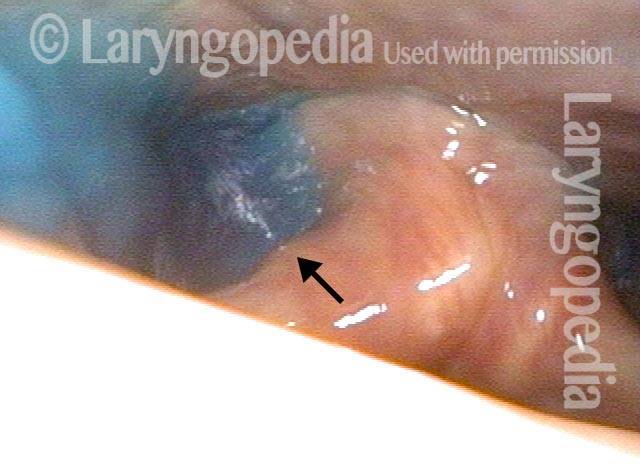
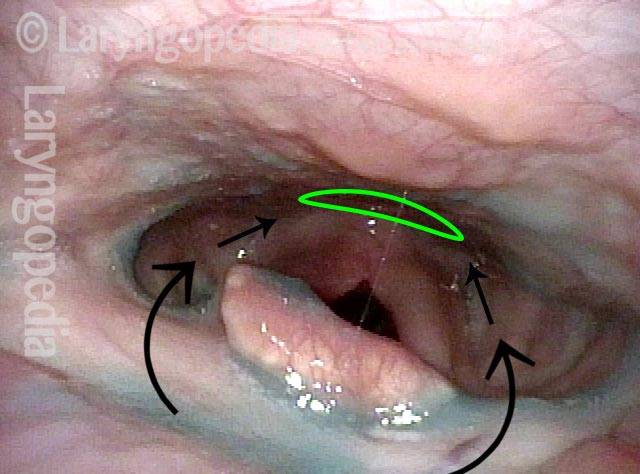
Laryngopharynx (1 of 3)
Laryngopharynx (1 of 3)
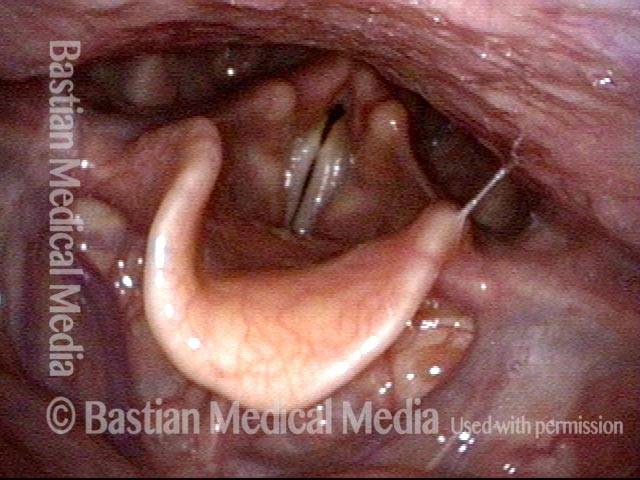
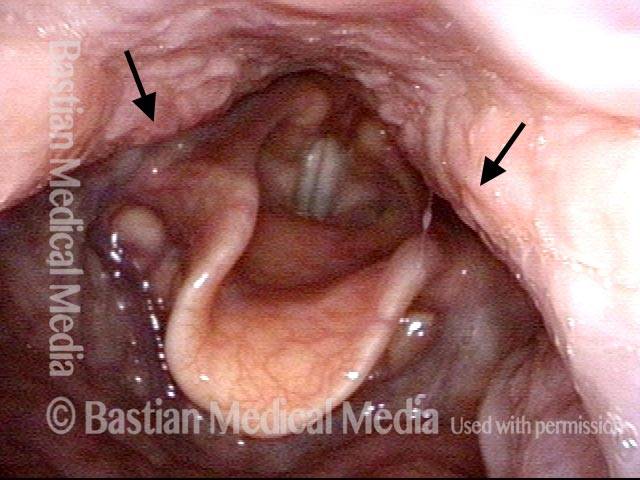
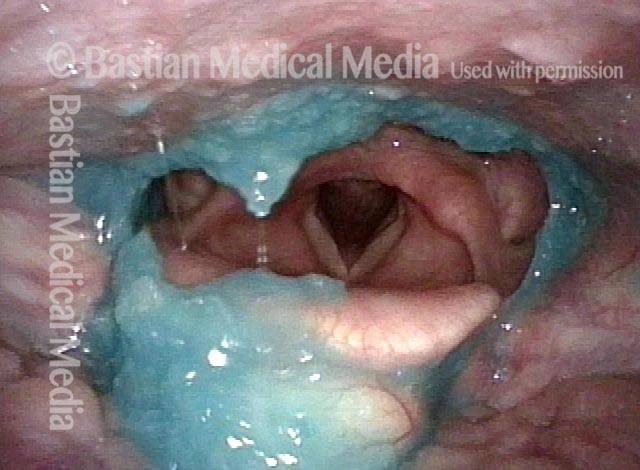
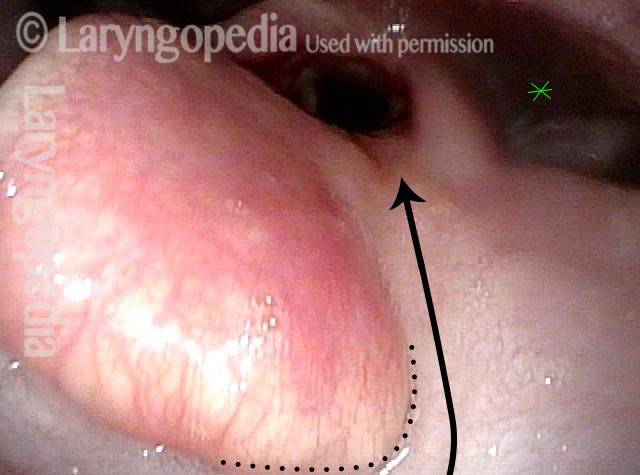
Dysphagia / Delayed swallow reflex (2 of 3)
Dysphagia / Delayed swallow reflex (2 of 3)
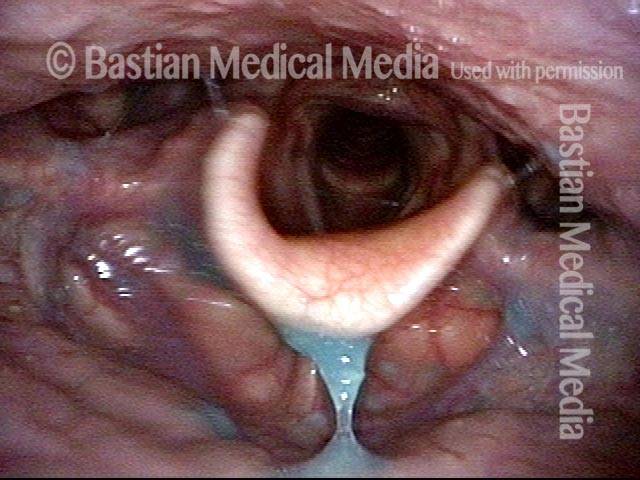
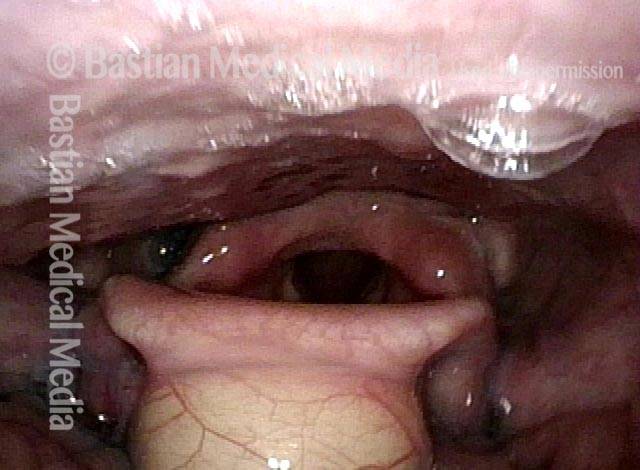
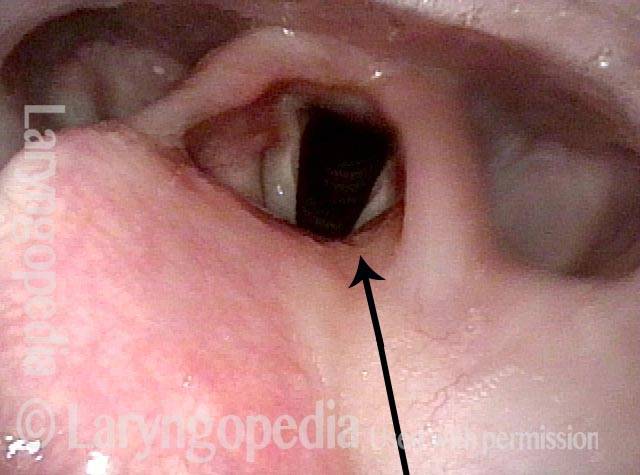
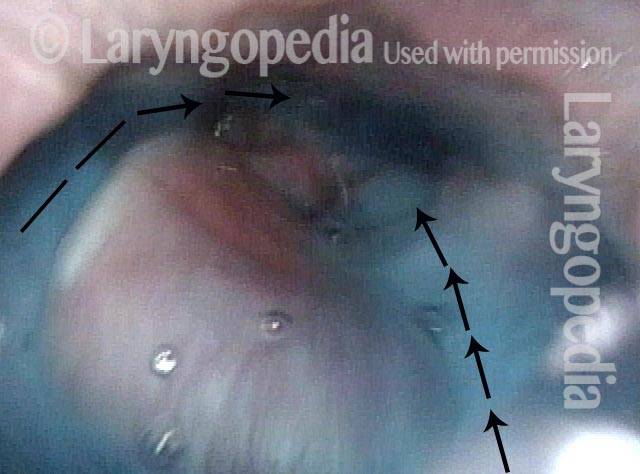
Hypopharyngeal pooling (3 of 3)
Hypopharyngeal pooling (3 of 3)
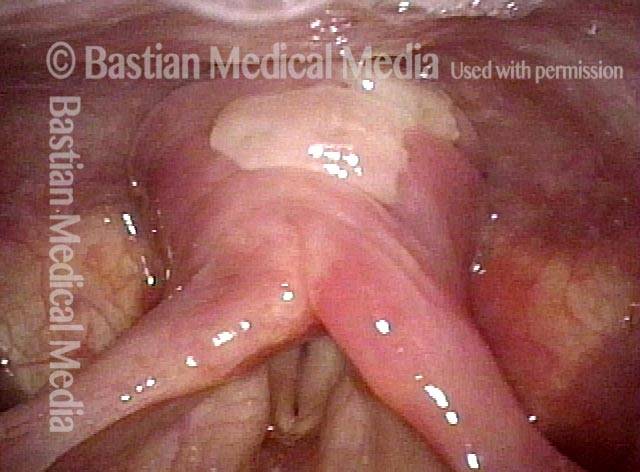
Il muscolo cricofaringeo visto durante la deglutizione
This person struggles to swallow due to a combination of prior tongue cancer surgery decades ago, and longterm radiation effects. Solid foods are the most problematic, and so this sequence shows an attempt to swallow water stained with blue food coloring.
Swallowing crescent (1 of 5)
Swallowing crescent (1 of 5)
Swallowing water (2 of 5)
Swallowing water (2 of 5)
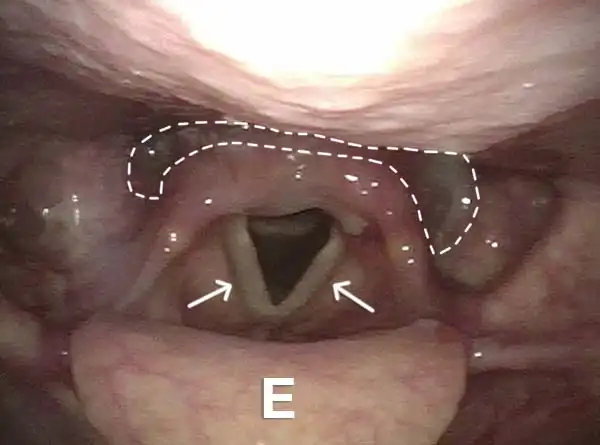
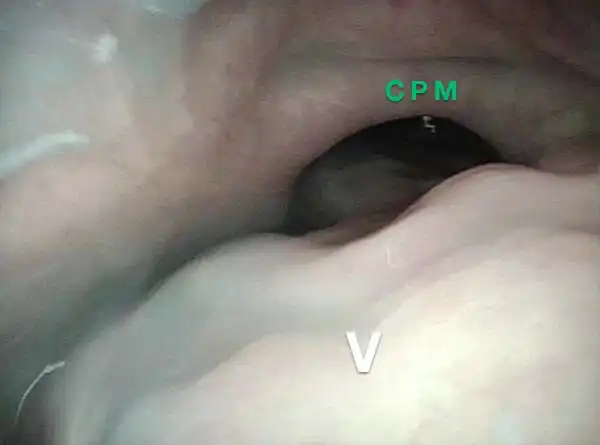
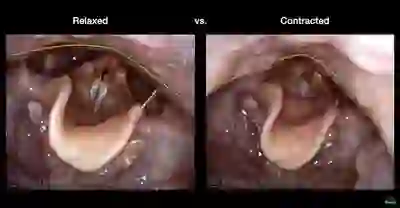
Cricopharyngeus muscle (3 of 5)
Cricopharyngeus muscle (3 of 5)
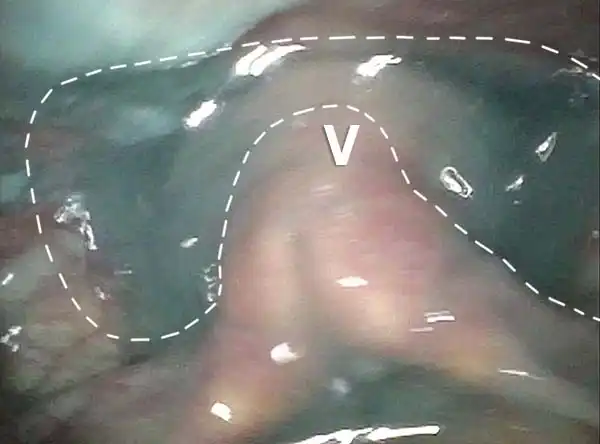
Relaxed CPM (4 of 5)
Relaxed CPM (4 of 5)
Partially open esophagus due to A-CPD (5 of 5)
Partially open esophagus due to A-CPD (5 of 5)
Diverticolo di Zenker
Zenker’s diverticulum (1 of 3)
Zenker’s diverticulum (1 of 3)
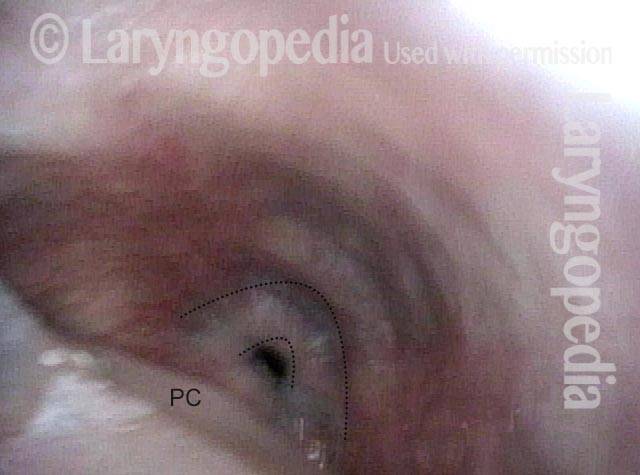
Postcricoid area (2 of 3)
Postcricoid area (2 of 3)
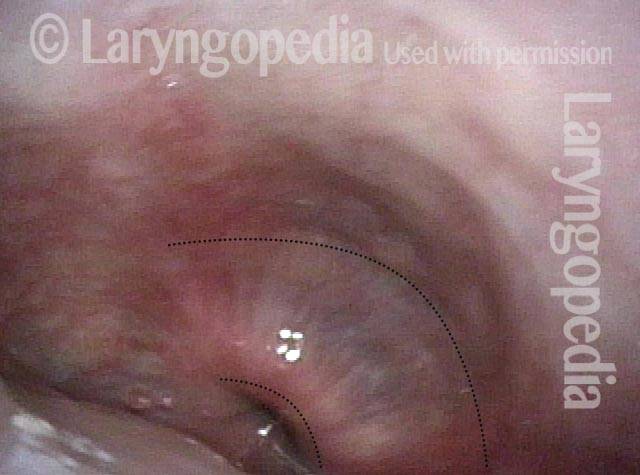
Hypopharynx (3 of 3)
Hypopharynx (3 of 3)
Reflusso nell’ipofaringe, caratteristico della disfunzione cricofaringea
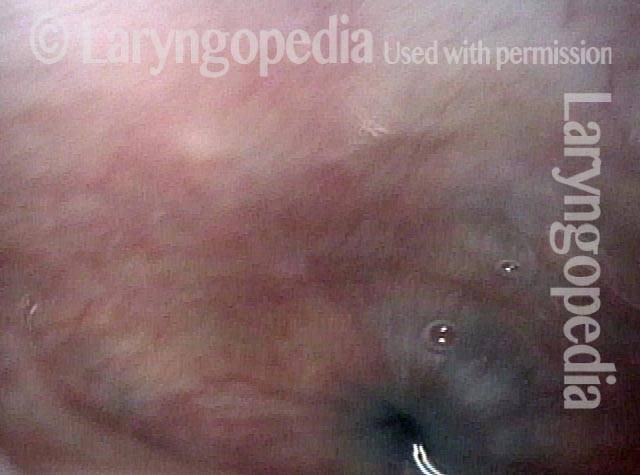
Reflux into hypopharynx (1 of 3)
Reflux into hypopharynx (1 of 3)
Water flows into the swallowing crescent (2 of 3)
Water flows into the swallowing crescent (2 of 3)
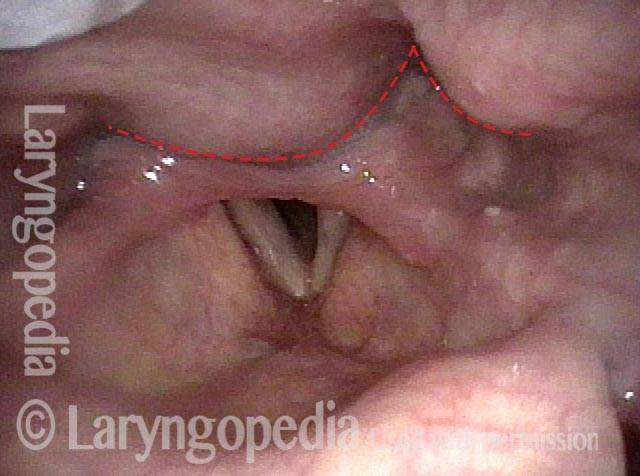
Larynx opens up (3 of 3)
Larynx opens up (3 of 3)
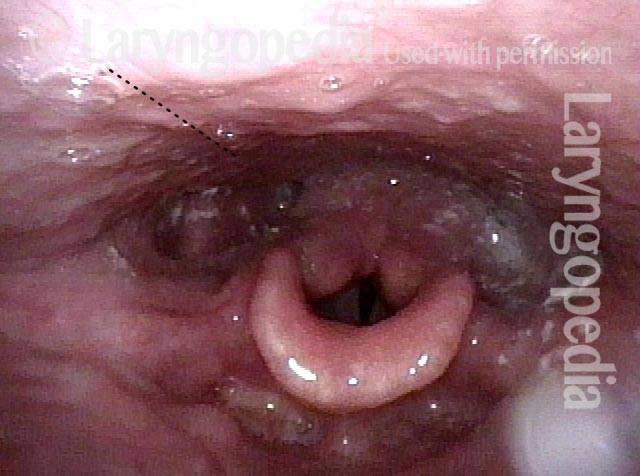
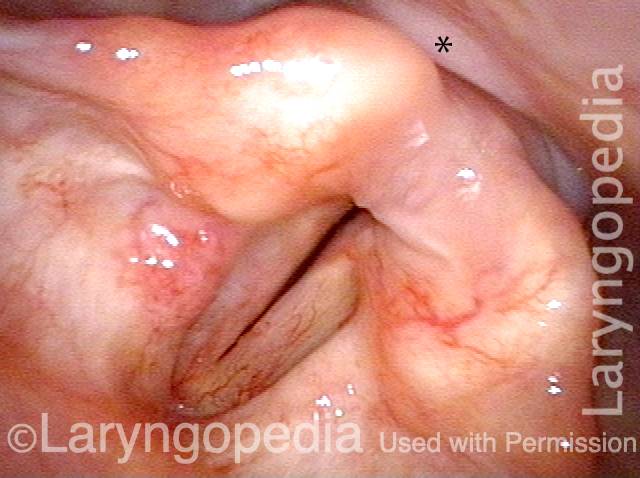
Le cisti vallecolari non disturbano la deglutizione, tranne quando lo fanno
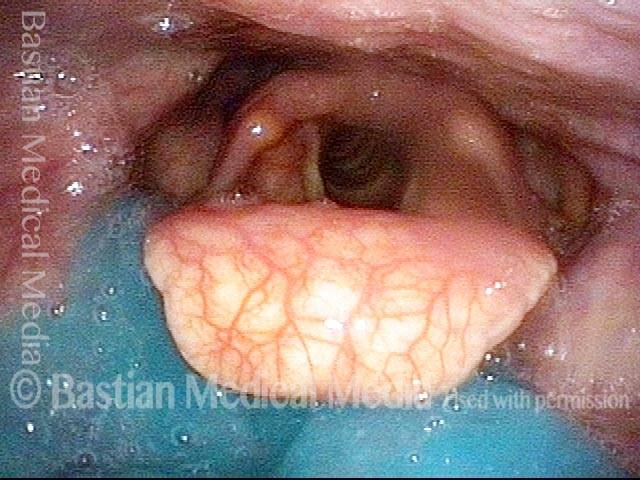
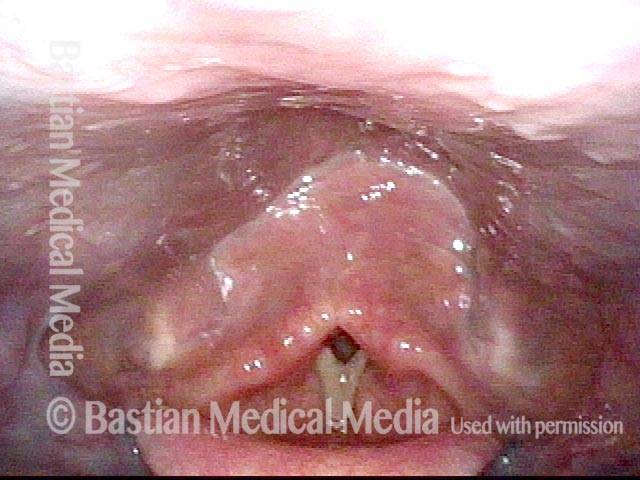
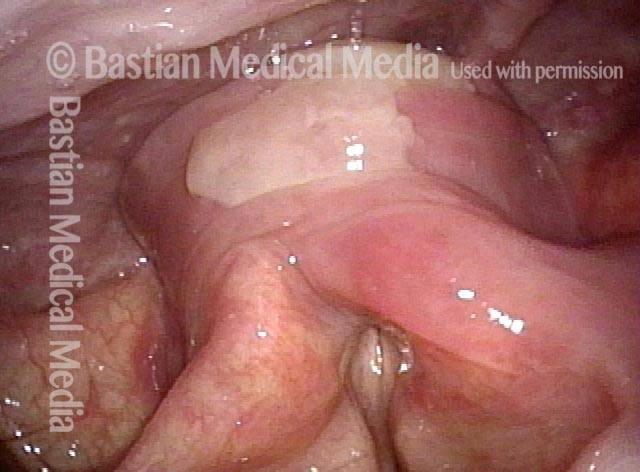
Vallecular cyst (1 of 4)
Vallecular cyst (1 of 4)
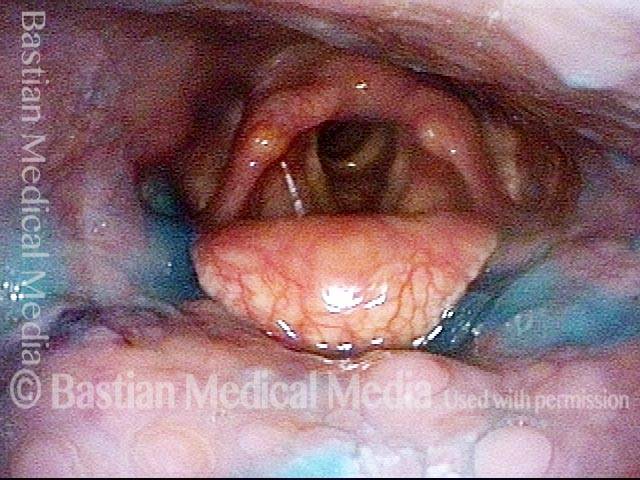
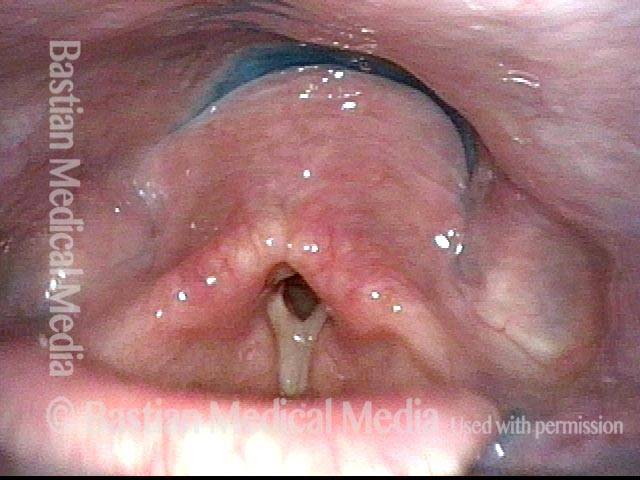
Evaluation of function (2 of 4)
Evaluation of function (2 of 4)
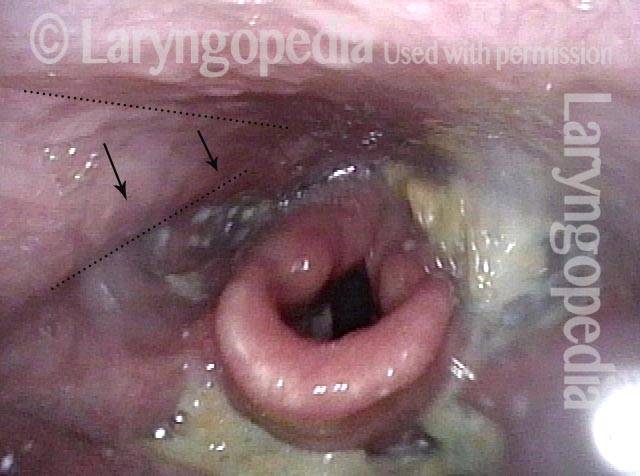
Applesauce residue (3 of 4)
Applesauce residue (3 of 4)
Water wash (4 of 4)
Water wash (4 of 4)
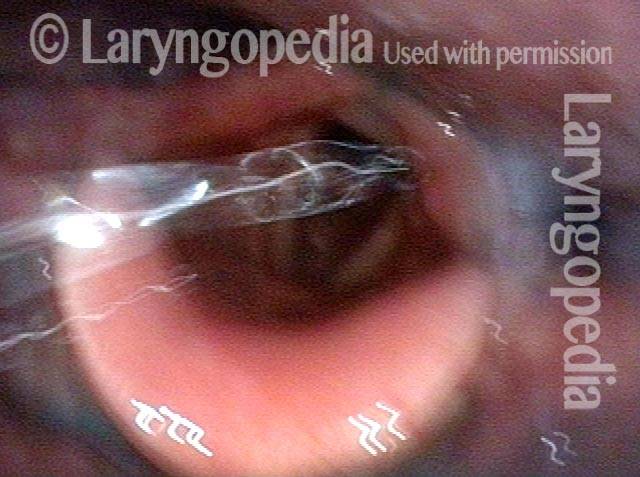
Alloggiamento della pillola a causa di difficoltà di deglutizione
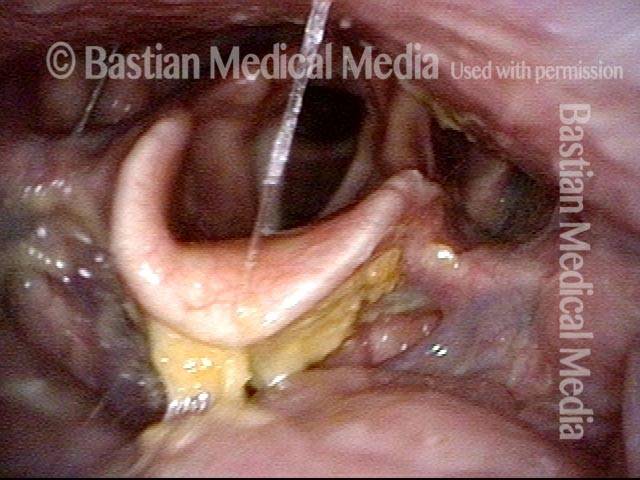
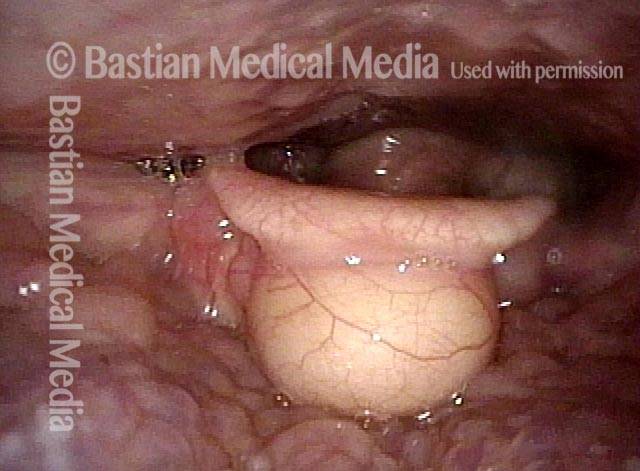
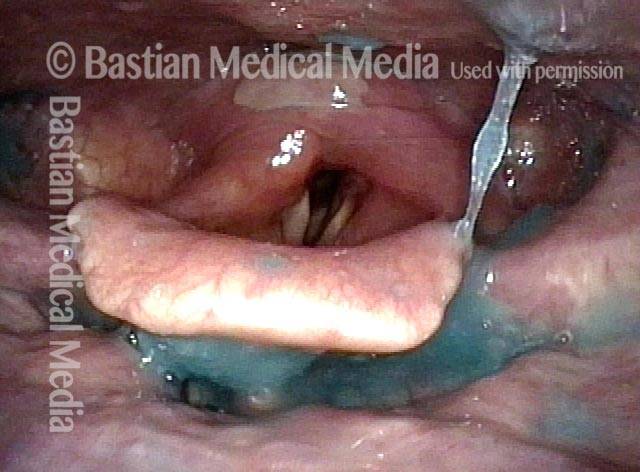
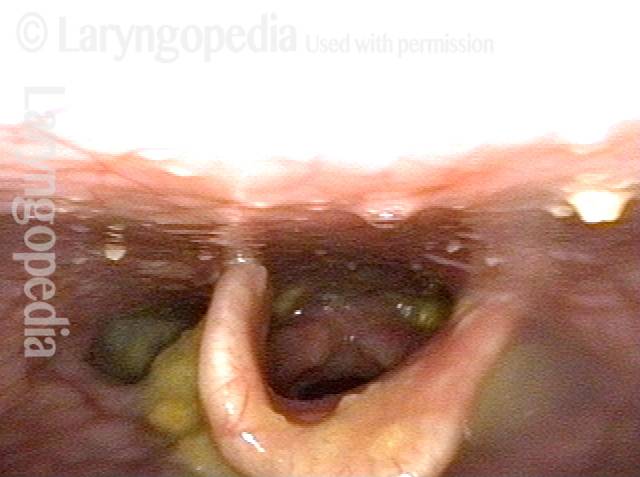
Lodged pill (1 of 4)
Lodged pill (1 of 4)
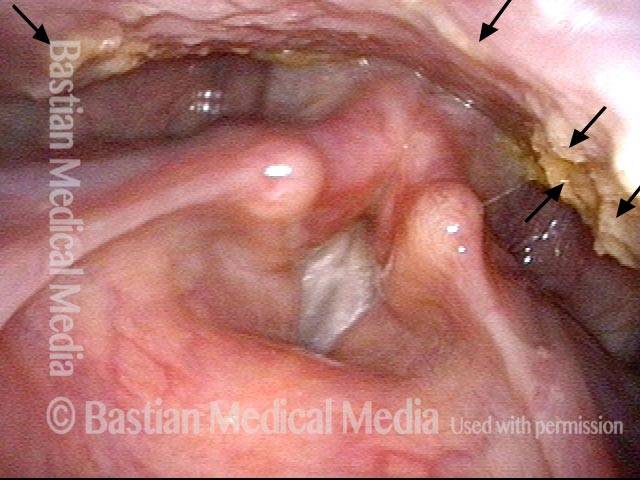
Trumpet maneuver (2 of 4)
Trumpet maneuver (2 of 4)
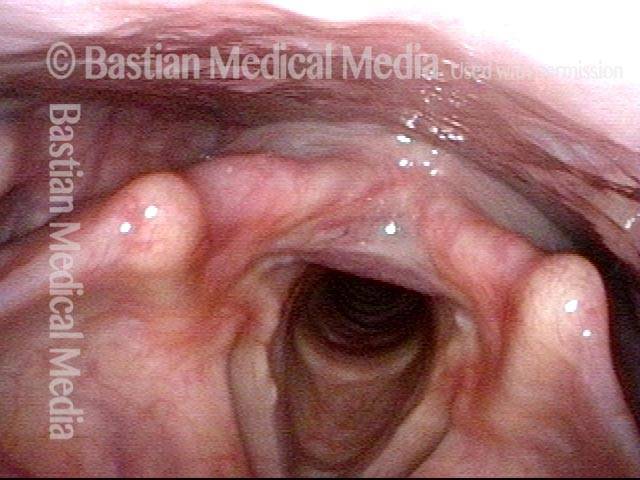
VESS (3 of 4)
VESS (3 of 4)
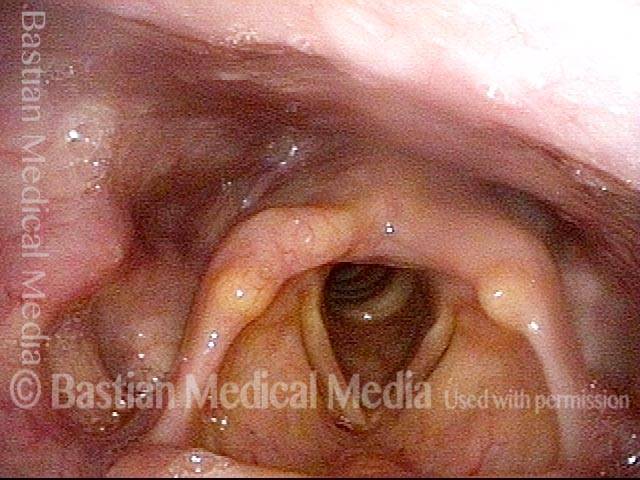
Incomplete relaxation of CPD (4 of 4)
Incomplete relaxation of CPD (4 of 4)
Riflesso ritardato della deglutizione: confronta la salsa di mele blu e l’acqua blu
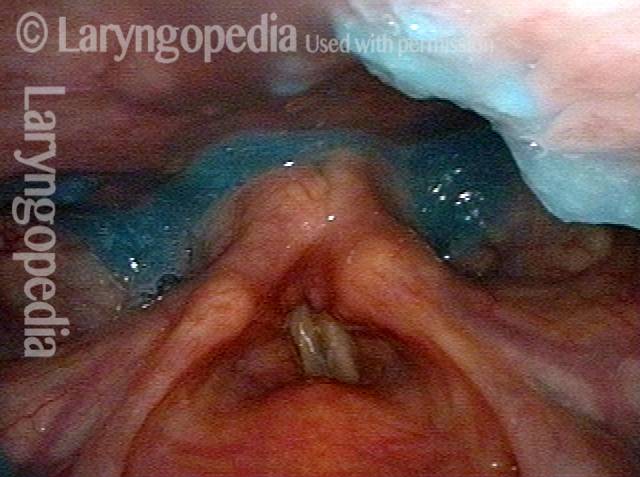
VESS (1 of 4)
VESS (1 of 4)
Delayed swallow reflex (2 of 4)
Delayed swallow reflex (2 of 4)
Blue-stained water (3 of 4)
Blue-stained water (3 of 4)
No residue (4 of 4)
No residue (4 of 4)
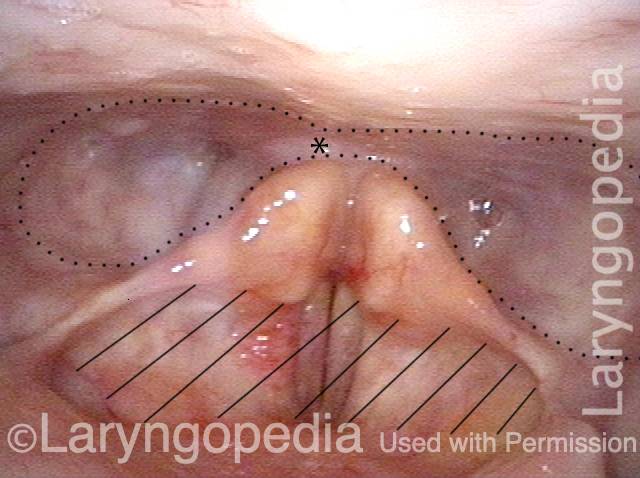
Scarring Diverts Swallowed Materials Directly into the Larynx
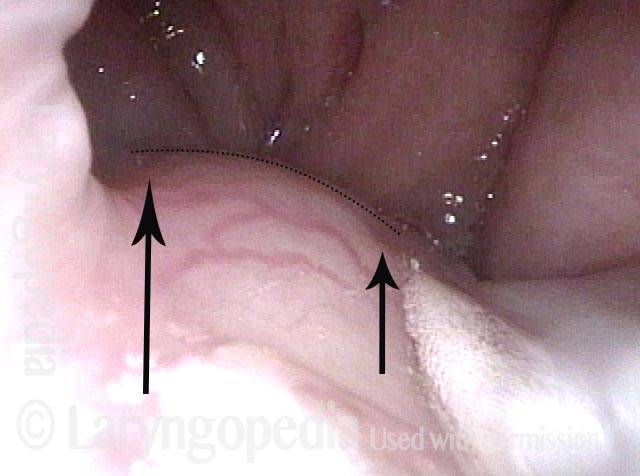
Post tonsillectomy (1 of 4)
Post tonsillectomy (1 of 4)
Closer view (2 of 4)
Closer view (2 of 4)
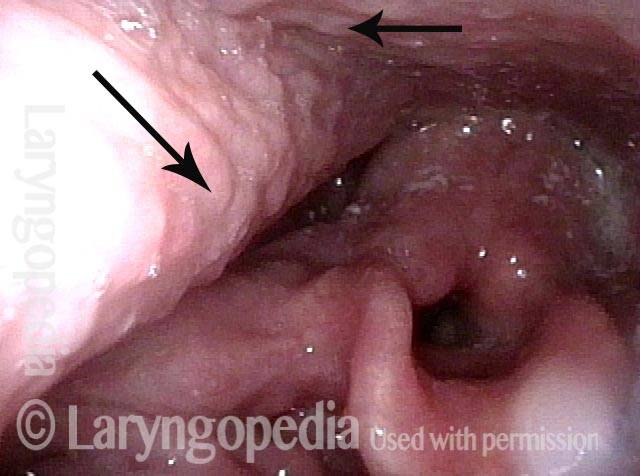
The “chute” (3 of 4)
The “chute” (3 of 4)
Abnormal diversion (4 of 4)
Abnormal diversion (4 of 4)
Frattura della base cranica e lesione del nervo vago: notare la contrazione della faringe e l’impatto sulla deglutizione
Palate branch of the vagus nerve (1 of 4)
Palate branch of the vagus nerve (1 of 4)
Pharynx branch of the vagus nerve (2 of 4)
Pharynx branch of the vagus nerve (2 of 4)
Damage to left vagal nerve function (3 of 4)
Damage to left vagal nerve function (3 of 4)
Residue during swallowing test (4 of 4)
Residue during swallowing test (4 of 4)
SDVS in 6 foto
Assessing the patient’s swallowing (1 of 6)
Assessing the patient’s swallowing (1 of 6)
Observing the pharynx (2 of 6)
Observing the pharynx (2 of 6)
Patient secretions (3 of 6)
Patient secretions (3 of 6)
Pooling of swallowed pureed food (4 of 6)
Pooling of swallowed pureed food (4 of 6)
Swallowing solids (5 of 6)
Swallowing solids (5 of 6)
Residue after foods (6 of 6)
Residue after foods (6 of 6)
Risultati SVDS dopo la radioterapia
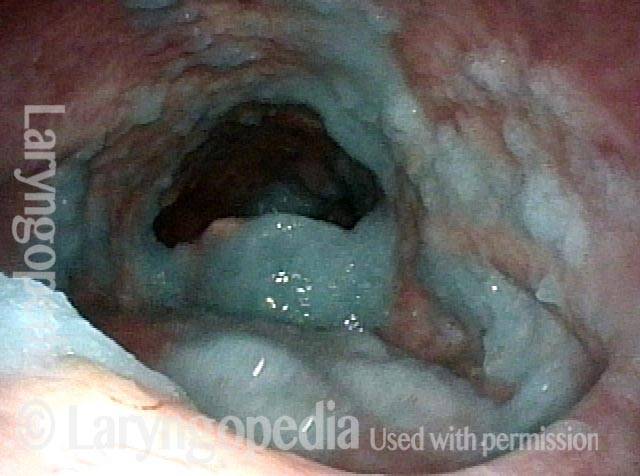
Narrowed pharyngeal wall (1 of 7)
Narrowed pharyngeal wall (1 of 7)
Swallowing applesauce (2 of 7)
Swallowing applesauce (2 of 7)
After sipping water (3 of 7)
After sipping water (3 of 7)
Gravity aiding in swallowing (4 of 7)
Gravity aiding in swallowing (4 of 7)
Lifting larynx (5 of 7)
Lifting larynx (5 of 7)
A closer look (6 of 7)
A closer look (6 of 7)
Gravity aiding again in swallowing (7 of 7)
Gravity aiding again in swallowing (7 of 7)
Gli osteofiti cervicali non sembrano di per sé un grave ostacolo alla deglutizione
Protruding osteophytes (1 of 2)
Protruding osteophytes (1 of 2)
Rapid swallowing (2 of 2)
Rapid swallowing (2 of 2)
Aspirazione e fontana dell’aspirazione restituita dopo la tosse
Salivary pooling (1 of 5)
Salivary pooling (1 of 5)
After applesauce (2 of 5)
After applesauce (2 of 5)
After cheese cracker (3 of 5)
After cheese cracker (3 of 5)
After water (4 of 5)
After water (4 of 5)
Cough expels the water from airway (5 of 5)
Cough expels the water from airway (5 of 5)
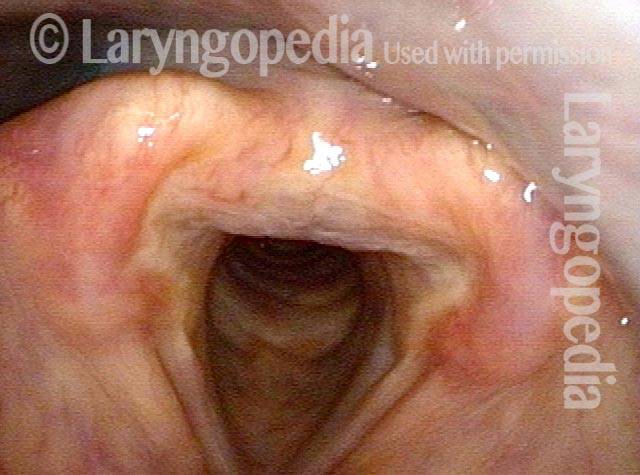
Tre viste dell’ingresso dell’esofago da lontano a da vicino
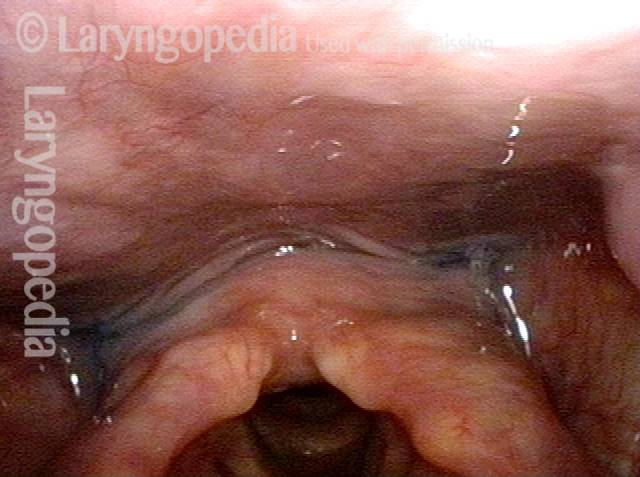
Swallowing Crescent (1 of 3)
Swallowing Crescent (1 of 3)
Closed esophagus (2 of 3)
Closed esophagus (2 of 3)
Open Esophagus (3 of 3)
Open Esophagus (3 of 3)
Condividi questo articolo
SDVS (Studio sulla deglutizione videoendoscopica)
Metodo per valutare la capacità di deglutizione di una persona mediante un esame fisico documentato tramite video, guardando dall’interno della gola. Chiamata anche valutazione endoscopica a fibre ottiche della deglutizione (FEES).
Rondine centenaria!
Lo studio videoendoscopico della deglutizione (VESS) è un metodo per valutare la capacità di deglutizione di una persona mediante un esame fisico documentato video, guardando dall’interno della gola. Questo video presenta l’esempio di un paziente di 100 anni sottoposto a VESS.
Difficoltà di deglutizione 101
Questo video offre una panoramica di come funziona la deglutizione, di come a volte può andare storto e dei possibili modi per trattare questi problemi.
Videoconsulto con il dottor Bastian
Qual è la differenza tra VESS e VFSS?
VESS è una metodologia completa, spesso autonoma, modellata in molti modi sullo studio della deglutizione videofluoroscopica (VFSS).
VFSS utilizza tre consistenze di materiale alimentare – liquido, purea e solido – mescolato con bario e somministrato sotto la supervisione di un logopedista nella sala radiografica di un ospedale.
Al contrario, VESS utilizza l’imaging videoendoscopico visivo del tratto di deglutizione. L’anatomia del paziente e l’esame neurologico (palato, faringe e laringe) vengono prima valutati in dettaglio utilizzando varie tecniche di elicitazione. Successivamente viene rilevata la presenza o l’assenza di saliva trattenuta.
Infine, al paziente vengono offerti, in una sequenza appropriata, acqua, budino e cracker, ciascuno colorato con colorante alimentare, per valutare la capacità di deglutizione. Quando vi sono dubbi sulla funzione esofagea, potrebbe essere necessario eseguire anche la VFSS.
Quando la VFSS è già stata eseguita o quando sono necessari studi di follow-up sulla deglutizione, la VESS viene generalmente utilizzata come alternativa alla VFSS.