Laryngitis
Laryngitis is an infection or inflammation of the larynx. The cause can be viral, bacterial, or fungal (candida). Or it can result from acid reflux, cancer radiation therapy, surgery (as temporary post-operative inflammation), or an auto-immune disorder.
Chronic Bacterial Laryngitis
Chronic bacterial laryngitis is a laryngologic problem looking for a more definitive solution. Seen in persons who have undergone radiotherapy or who have an immune defect. The laryngitis can often be improved with antibiotics, but often recurs when antibiotics are discontinued. Sometimes chronic antibiotic administration is needed. Or, laryngeal irrigations.
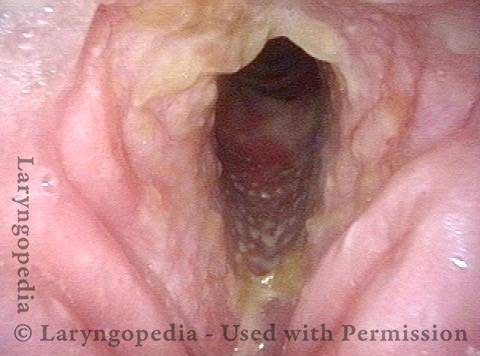
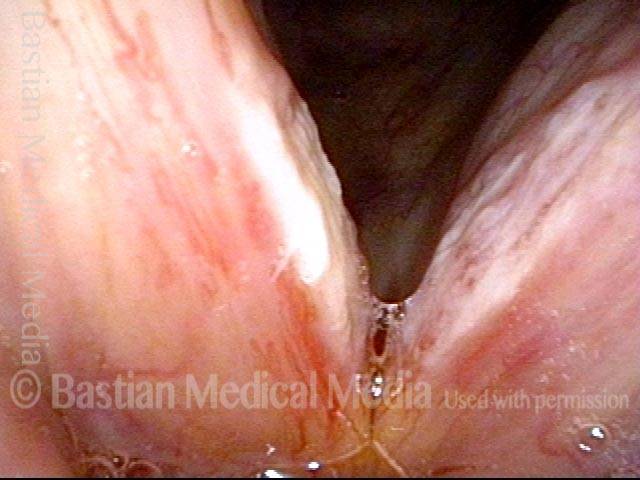
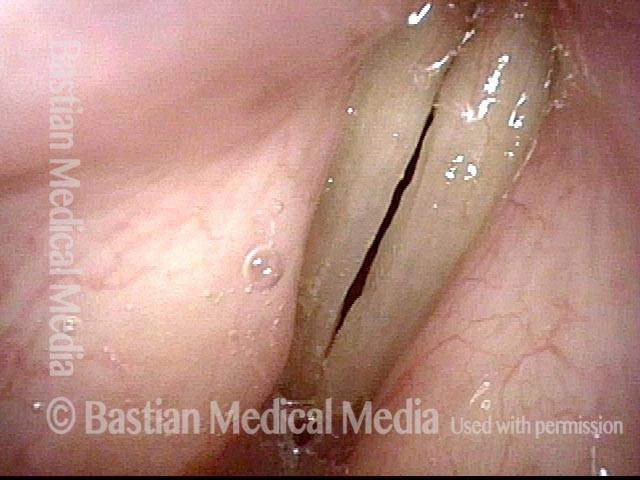
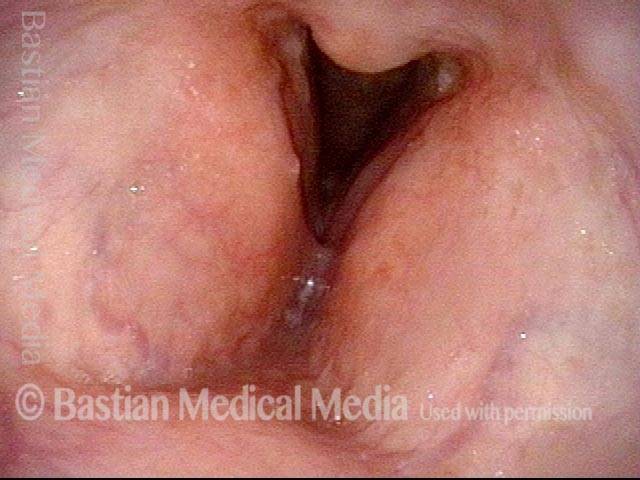
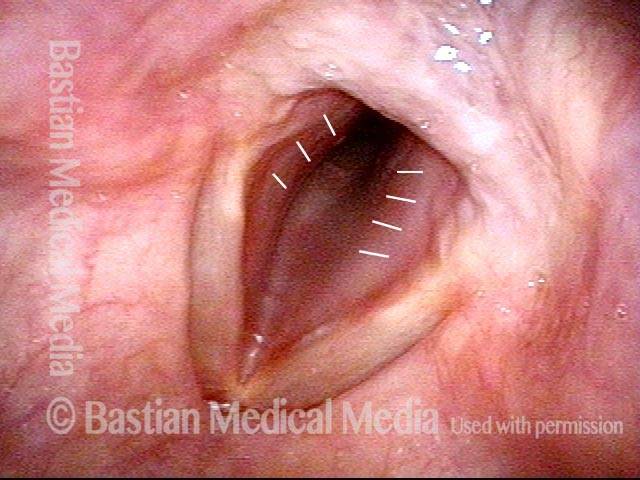
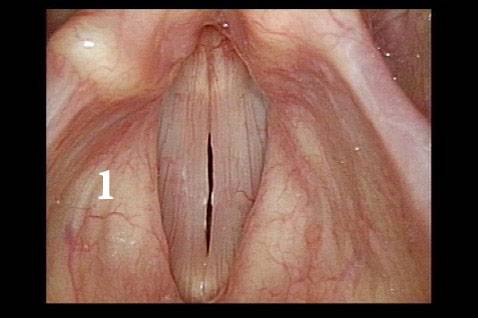
Bacterial infection? (1 of 5)
Bacterial infection? (1 of 5)
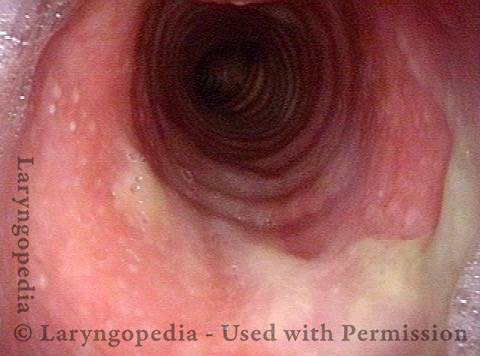
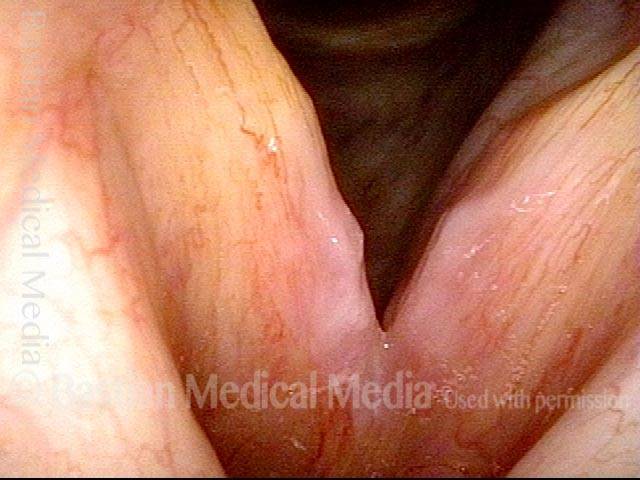
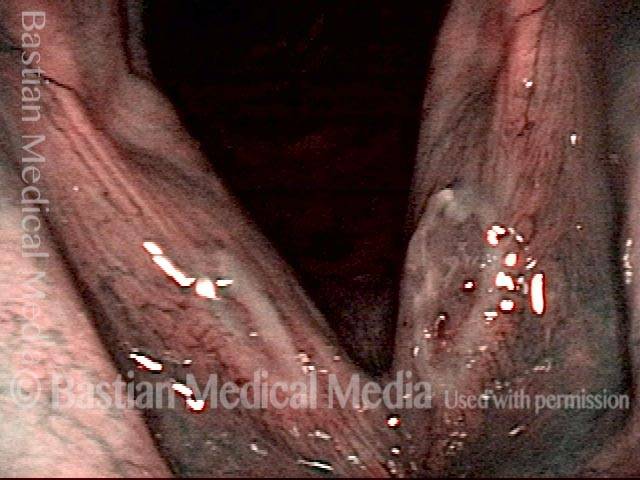
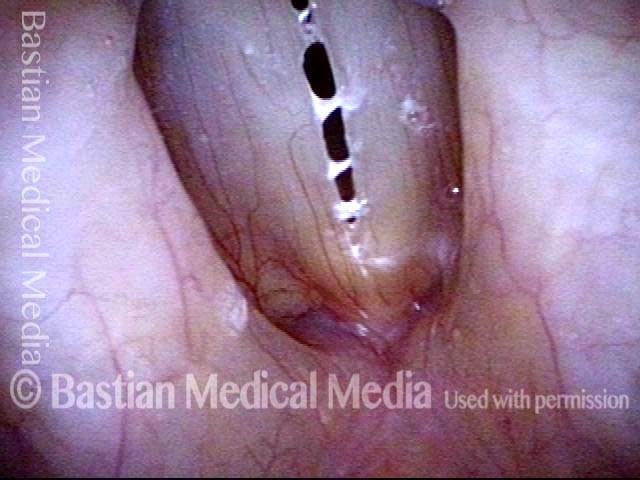
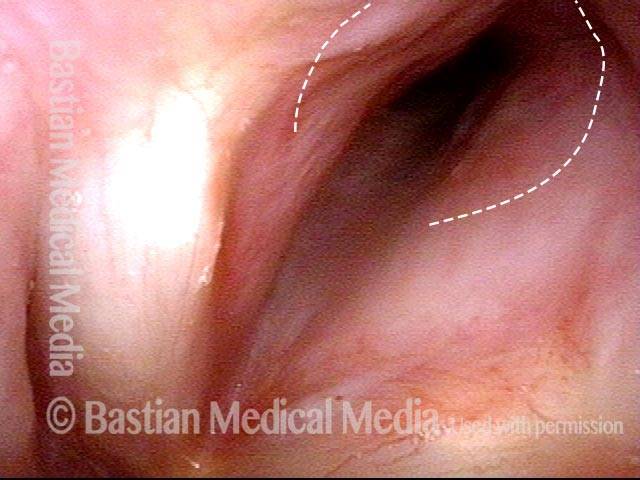
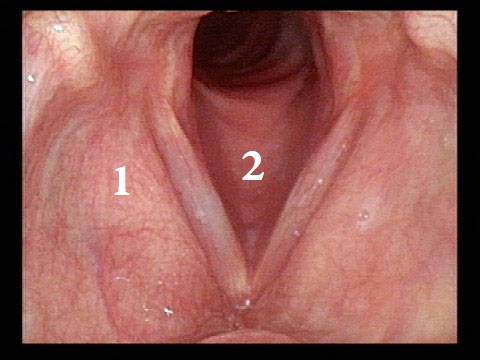
Yellow mucus (2 of 5)
Yellow mucus (2 of 5)
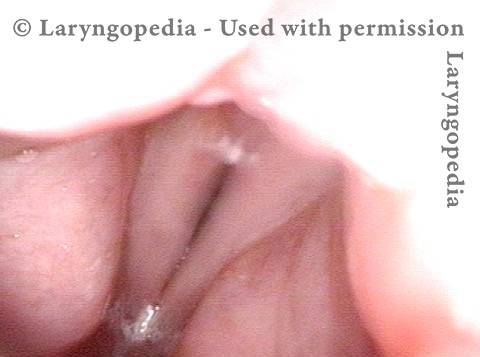
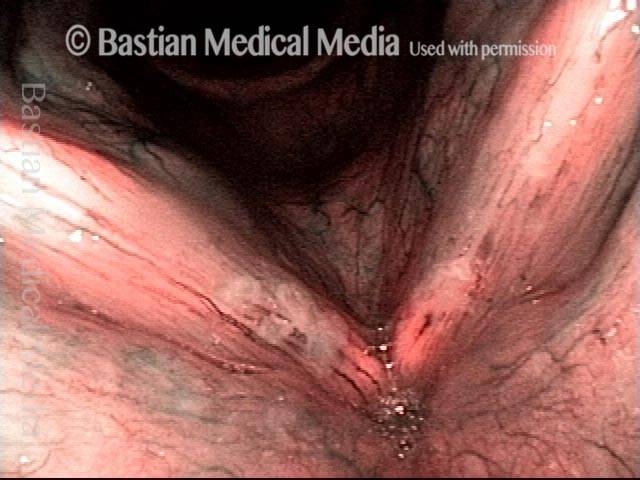
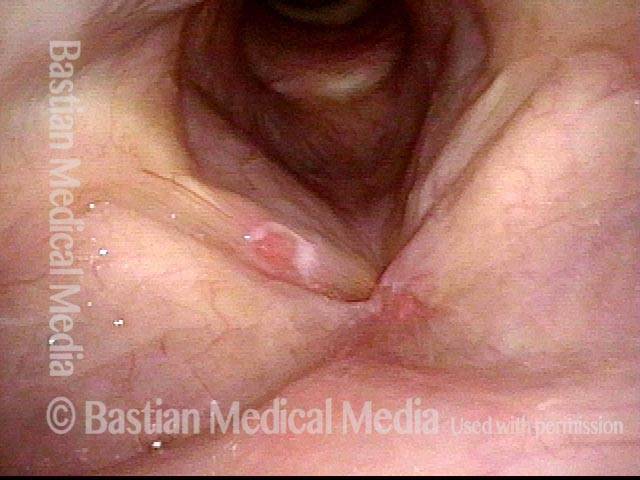
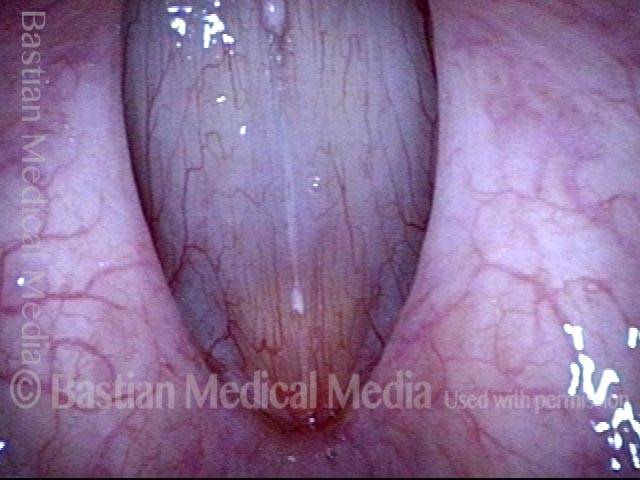
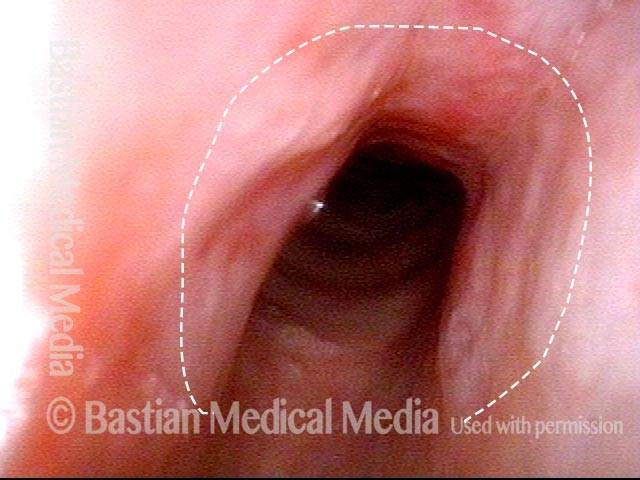
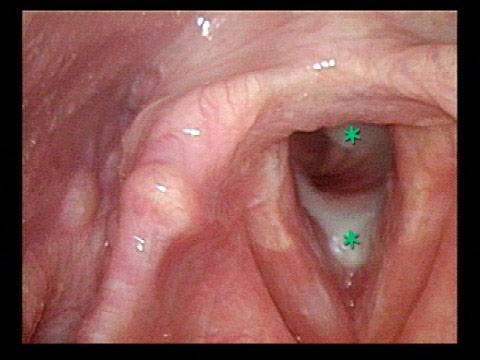
Improvement (3 of 5)
Improvement (3 of 5)
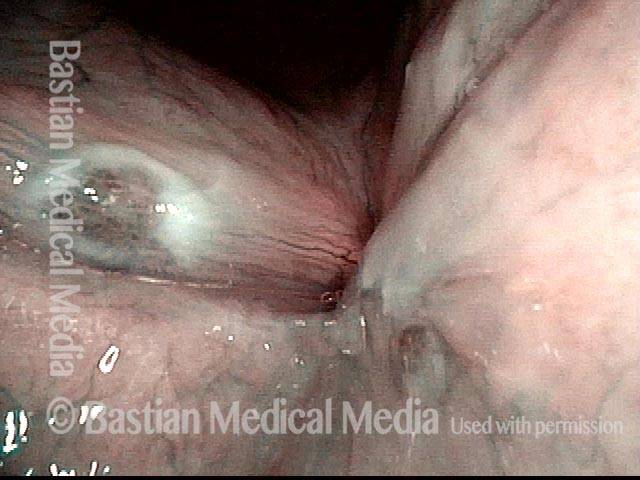
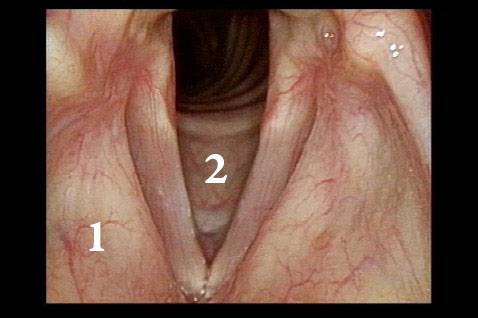
Improved voice (4 of 5)
Improved voice (4 of 5)
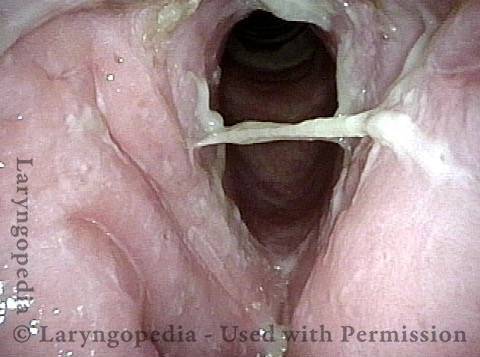
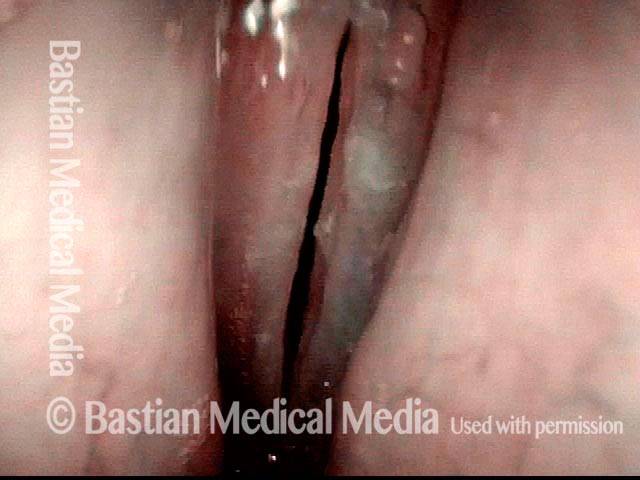
Infection returns (5 of 5)
Infection returns (5 of 5)
Candida laryngitis, before and after treatment
Candida laryngitis (1 of 4)
Candida laryngitis (1 of 4)
Candida laryngitis (2 of 4)
Candida laryngitis (2 of 4)
Candida laryngitis, 15 days after starting treatment (3 of 4)
Candida laryngitis, 15 days after starting treatment (3 of 4)
Candida laryngitis, several months later (4 of 4)
Candida laryngitis, several months later (4 of 4)
Example 2
Candida laryngitis (1 of 4)
Candida laryngitis (1 of 4)
Candida laryngitis (2 of 4)
Candida laryngitis (2 of 4)
Candida laryngitis, after treatment (3 of 4)
Candida laryngitis, after treatment (3 of 4)
Candida laryngitis, after treatment (4 of 4)
Candida laryngitis, after treatment (4 of 4)
Example 3
Candida laryngitis (1 of 3)
Candida laryngitis (1 of 3)
Candida laryngitis (2 of 3)
Candida laryngitis (2 of 3)
Candida laryngitis, after starting treatment (3 of 3)
Candida laryngitis, after starting treatment (3 of 3)
Gradual Healing of Ulcerative Laryngitis
Ulcerative laryngitis (1 of 4)
Ulcerative laryngitis (1 of 4)
Ulcerative laryngitis (2 of 4)
Ulcerative laryngitis (2 of 4)
1 month later: ulcerative laryngitis healing (3 of 4)
1 month later: ulcerative laryngitis healing (3 of 4)
3 months later: ulcerative laryngitis virtually all healed (4 of 4)
3 months later: ulcerative laryngitis virtually all healed (4 of 4)
Vocal Cord Ulcer
Vocal cord ulcer (1 of 2)
Vocal cord ulcer (1 of 2)
Vocal cord ulcer (2 of 2)
Vocal cord ulcer (2 of 2)
Laryngitis Sicca
Laryngitis sicca (1 of 2)
Laryngitis sicca (1 of 2)
Laryngitis sicca (2 of 2)
Laryngitis sicca (2 of 2)
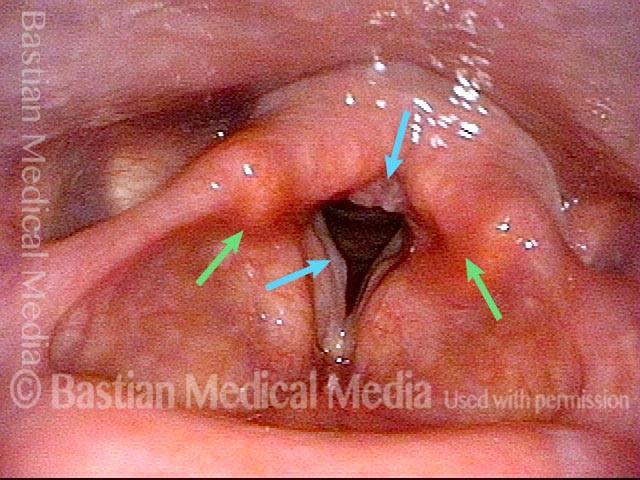
Pachyderma, Caused by Laryngitis Sicca
Heaped up Mucosa (1 of 3)
Heaped up Mucosa (1 of 3)
Pachyderma (2 of 3)
Pachyderma (2 of 3)
Stippled Vascular Markings (3 of 3)
Stippled Vascular Markings (3 of 3)
Acid Reflux
Phonation (1 of 2)
Phonation (1 of 2)
Acid reflux (2 of 2)
Acid reflux (2 of 2)
Example 2
Acid reflux (1 of 2)
Acid reflux (1 of 2)
Excessive mucus (2 of 2)
Excessive mucus (2 of 2)
Acid Reflux + Laryngitis
Acid reflux laryngitis (1 of 2)
Acid reflux laryngitis (1 of 2)
Acid reflux laryngitis (2 of 2)
Acid reflux laryngitis (2 of 2)
Croup, aka Laryngotracheitis
Croup, aka laryngotracheitis (1 of 4)
Croup, aka laryngotracheitis (1 of 4)
Croup, aka laryngotracheitis (2 of 4)
Croup, aka laryngotracheitis (2 of 4)
Croup, aka laryngotracheitis (3 of 4)
Croup, aka laryngotracheitis (3 of 4)
Croup, aka laryngotracheitis (4 of 4)
Croup, aka laryngotracheitis (4 of 4)
Acute Laryngitis “Redness”
Occasionally, the findings of acute laryngitis are not as “dramatic” as the voice change would suggest. There is not necessarily a lot of swelling, but instead, a diffuse pinkness or redness along with a change in secretions.