The pharynx (loosely “throat”) has a “foodway” function to convey food and liquid from the mouth to the esophagus. It also serves as part of the “airway,” also from mouth into the larynx and trachea. These foodway/airway functions are kept separate so food and liquid do not enter the airway towards the lungs. At the moment of swallowing, vocal cords clamp firmly together and epiglottis drops over the entrance of the larynx to divert food and liquid into the esophagus. During each swallow, lasting perhaps a second, breathing is briefly suspended. Once the food/liquid has gone by, the larynx re-opens and breathing resumes.
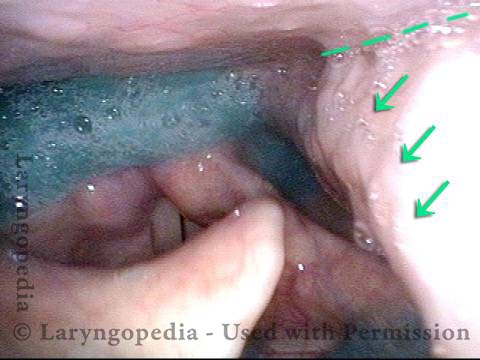
A thin sheet of muscle surrounds the pharynx, and squeezes to narrow the pharynx and help to propel swallowed material. That contraction lasts for approximately one second, each time the person swallows. The muscle is innervated bilaterally by the pharyngeal branch of the vagus nerve and so one side or both sides can be paralyzed by tumor, fracture at the base of the skull, viral injury, etc.
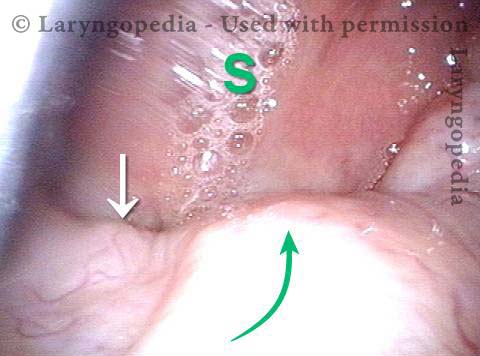
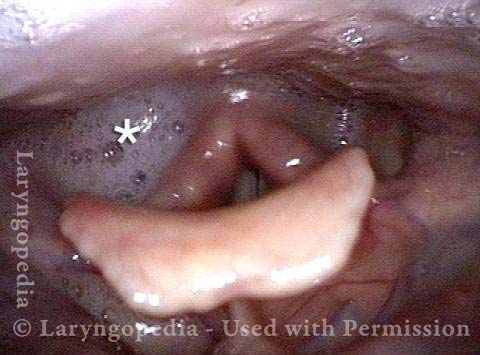
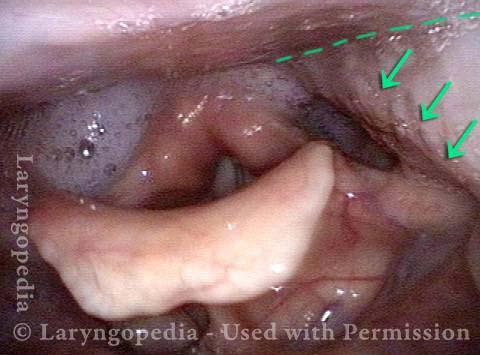
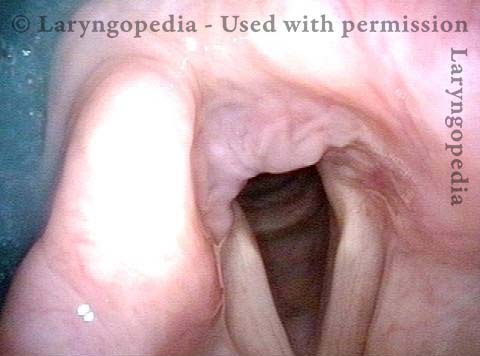
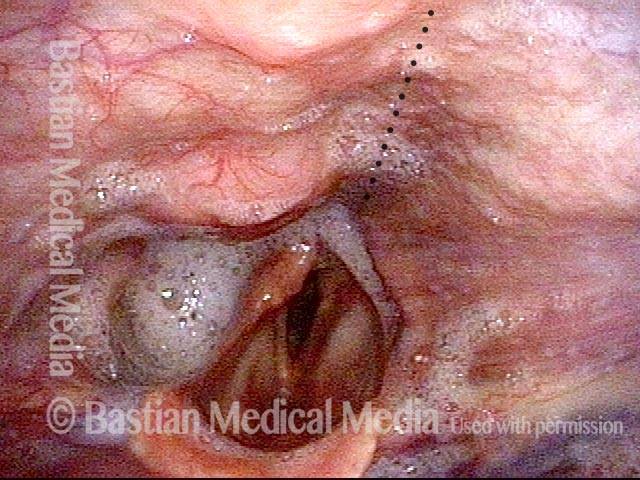
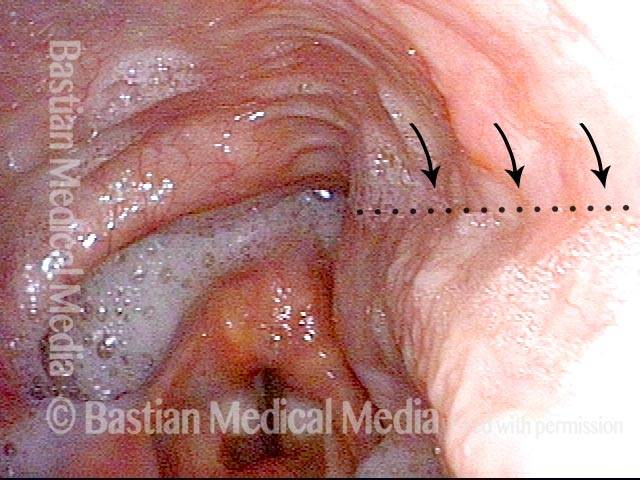
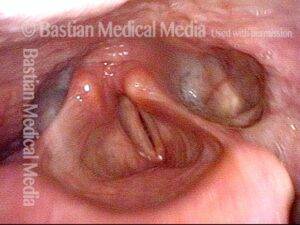
This diagnosis is often overlooked, because clinicians may not be clear on how to make the diagnosis. The best way is to obtain a clear panoramic view of the laryngopharynx as seen in the photo series below, and ask the patient to produce a very high pitch. This maneuver “recruits” contraction of the pharynx outside of the act of swallowing and allows the examiner to see clearly the difference in the contraction of the two sides. The paralyzed side is pulled to the non-paralyzed side, again as seen below.
Some with unilateral pharynx paralysis can compensate and continue to swallow (with limitations). Others are completely unable to surmount the impediment of this kind of paralysis.
High Vagus Nerve Injury
The vagus (10th cranial) nerve originates from the medulla (part of the brainstem), exits from the base of the skull through the jugular foramen, and among other things, supplies branches to the musculature of palate, pharynx, and larynx. Location of vagus nerve injury is sometimes evident by palate and pharynx findings. But these findings are sometimes overlooked as in this case, especially if palate and pharynx are weak but not completely paralyzed.
Case study: This 50-something woman developed a weak voice and moderate difficulty swallowing upon awakening 5 months prior to this visit. Fortunately, her symptoms of weak voice and difficulty swallowing were not devastating, and are improving. But up to this examination, there has been no diagnosis. This examination reveals a “lesion” of her right vagus nerve and it has to be at the base of the skull because palate, pharynx, and larynx muscles are all weak. Voice is functional but lacks the ability to project and has a “soft-edged” quality. A sophisticated listener can also hear mild hypernasality. The examination below prompts a scan with special attention to base of skull to be sure there is no mass lesion there.