Dysphagia
Dysphagia is the abnormal swallowing, or inability to swallow. It can result from such diverse causes as surgery on the larynx or neck, stroke, the aging process, tumor, injury to the neck, or radiation, among other things.
Treatment for Dysphagia (Swallowing Therapy)
This therapy is typically provided by a speech-language pathologist (and, more informally and adjunctively, by other healthcare professionals). General areas of teaching might include:
- Choosing wisely which food types and consistencies to eat (See Diet Modification below);
- Swallowing maneuvers such as tucking the chin, double swallow, effortful swallow, head turning, and supraglottic swallow;
- Direct exercises for the tongue, pharynx, palate, and larynx.
Diet Modification
These are suggested dietary changes, particularly regarding food consistencies, directed at improving a patient’s ability to swallow and at avoiding aspiration.
For example, an individual who is struggling with aspiration might be advised to avoid thin liquids and use thicker or carbonated liquids instead. Or this individual might be advised to avoid composite foods, since his or her swallowing deficiency could make it harder to “stay organized” with several consistencies in the mouth at once.
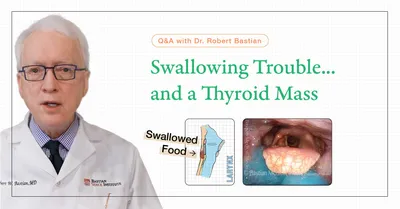
Q&A: Swallowing Trouble...and a Thyroid Mass
Question: My mother has been having difficulty swallowing. She has a benign thyroid growth that was found, and a doctor in her retirement community (she lives far away from me) wants to do surgery in 2 weeks. We’re feeling uncomfortable…
Answer:
I’m sorry to hear about your mother’s difficulty. While a diagnosis from afar is not possible, here are some thoughts that may help frame the situation more clearly.
It’s important to distinguish between two possibilities:
- The thyroid growth is causing the swallowing problem;
- The swallowing problem is unrelated, and the thyroid issue is simply a coincidental finding.
Thyroid Abnormalities and Swallowing
Thyroid enlargement is common, especially in older women, and many nodules or goiters are benign and do not require surgery unless they are:
- Causing clear symptoms (e.g., pressure, breathing difficulty)
- Suspicious for malignancy
- Growing rapidly
When the thyroid does cause swallowing difficulty, it is usually because of:
- Large size, especially if substernal (growing downward into the chest)
- Compression of the cervical esophagus, leading to difficulty swallowing, especially with solids and pills
But Swallowing Trouble Has Many Causes
If her swallowing issue led to imaging that incidentally found a thyroid mass, it’s possible the two problems are unrelated. For example:
- Antegrade Cricopharyngeus dysfunction (A-CPD)
- Presbyphagia (age-related swallow weakening)
- Other neuromuscular or esophageal issues
In such cases, removing the thyroid would not improve swallowing—and could delay correct diagnosis and treatment.
How to Distinguish?
A videoendoscopic swallow study (VESS) will certainly show if the patient has presbyphagia. And if swallowed material is well organized in pyriform sinuses, this would strongly suggest an outlet obstruction. But the most helpful test to clarify the thyroid question is a videofluoroscopic swallow study (VFSS, also known as a modified barium swallow or “cookie swallow”). It shows:
- How material moves through the mouth and throat
- Whether there is obstruction at the level of the cricopharyngeus muscle (upper esophageal sphincter)
- Whether aspiration or pooling is occurring
- If the esophagus is narrowed by external compression (like a thyroid mass)
Based on the findings:
- If it’s A-CPD, thyroidectomy won’t help—but cricopharyngeal myotomy or Botox injection could.
- If it’s presbyphagia, swallowing therapy, varying head position, and careful choice of food consistencies may be best—not surgery.
- If the thyroid is clearly compressing the esophagus, then thyroid surgery might be appropriate.
Bottom Line
Before proceeding with thyroid surgery to “fix” swallowing trouble, it’s essential to confirm causality. Ask the current medical team whether a modified barium swallow (videofluoroscopic swallow study) has been done—or if not, whether they will consider doing one.
A short video called “Swallowing Trouble 101” may also help in understanding the landscape of potential causes.
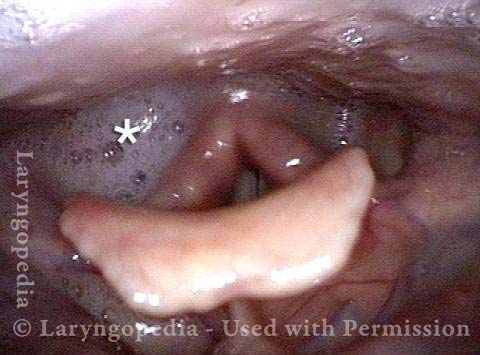
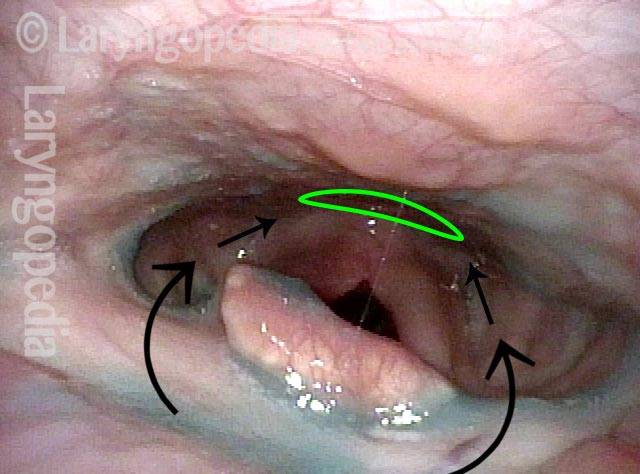
Dysphagia / Delayed Swallow Reflex
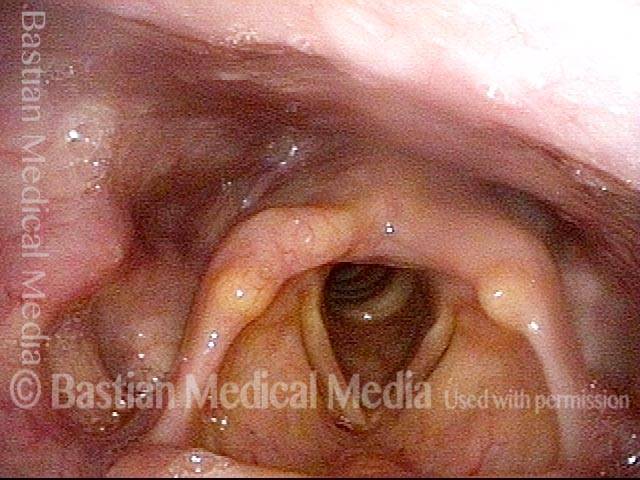
Laryngopharynx (1 of 3)
Laryngopharynx (1 of 3)
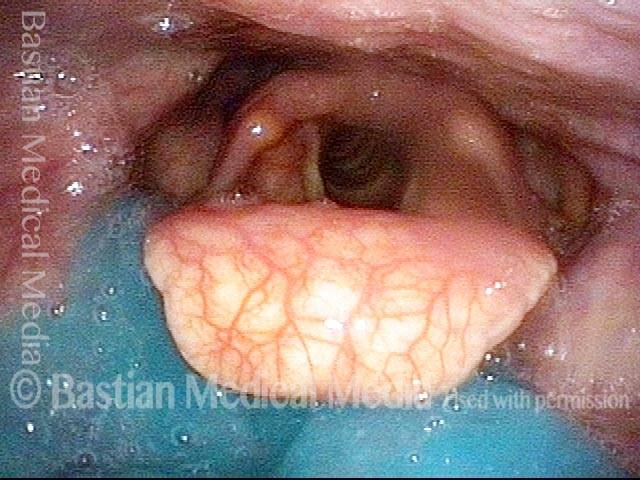
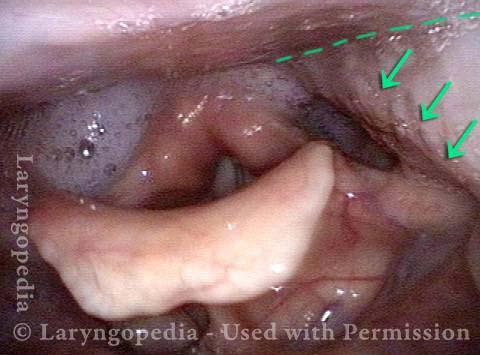
Dysphagia / Delayed swallow reflex (2 of 3)
Dysphagia / Delayed swallow reflex (2 of 3)
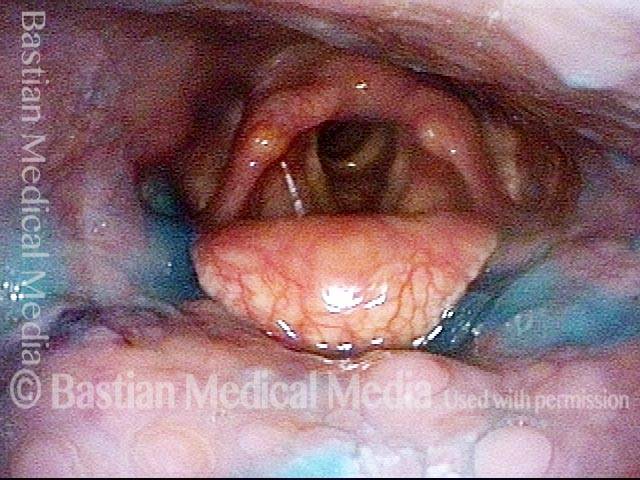
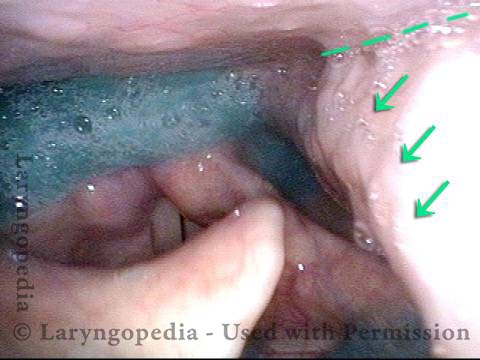
Hypopharyngeal pooling (3 of 3)
Hypopharyngeal pooling (3 of 3)
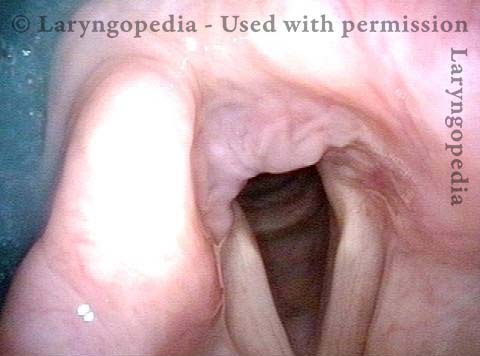
High Vagus Nerve Injury
The vagus (10th cranial) nerve originates from the medulla (part of the brainstem), exits from the base of the skull through the jugular foramen, and among other things, supplies branches to the musculature of palate, pharynx, and larynx. Location of vagus nerve injury is sometimes evident by palate and pharynx findings. But these findings are sometimes overlooked as in this case, especially if palate and pharynx are weak but not completely paralyzed.
Case study: This 50-something woman developed a weak voice and moderate difficulty swallowing upon awakening 5 months prior to this visit. Fortunately, her symptoms of weak voice and difficulty swallowing were not devastating, and are improving. But up to this examination, there has been no diagnosis.
This examination reveals a “lesion” of her right vagus nerve and it has to be at the base of the skull because palate, pharynx, and larynx muscles are all weak. Voice is functional but lacks the ability to project and has a “soft-edged” quality. A sophisticated listener can also hear mild hypernasality. The examination below prompts a scan with special attention to base of skull to be sure there is no mass lesion there.
Nasopharynx (1 of 7)
Nasopharynx (1 of 7)
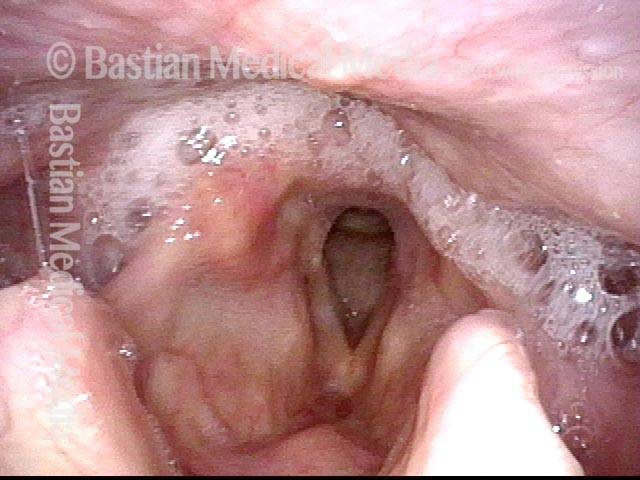
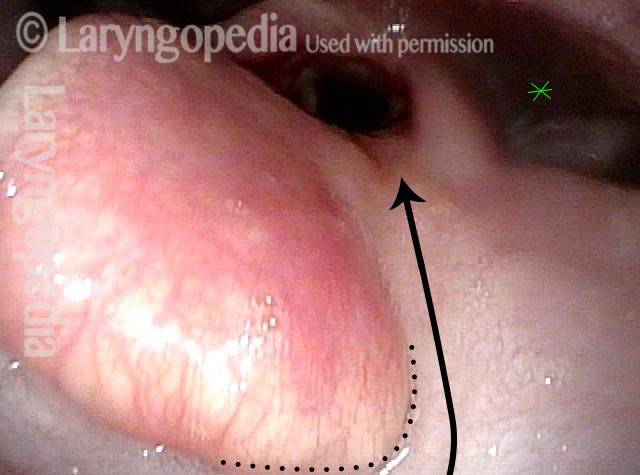
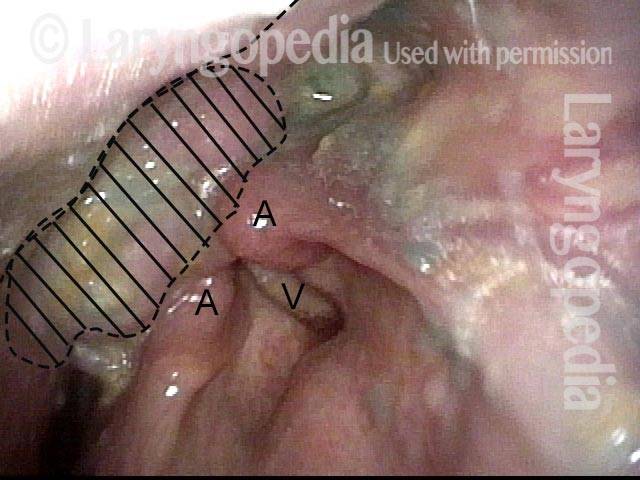
Saliva pooling in right pyriform sinus (2 of 7)
Saliva pooling in right pyriform sinus (2 of 7)
Pharynx contracts (3 of 7)
Pharynx contracts (3 of 7)
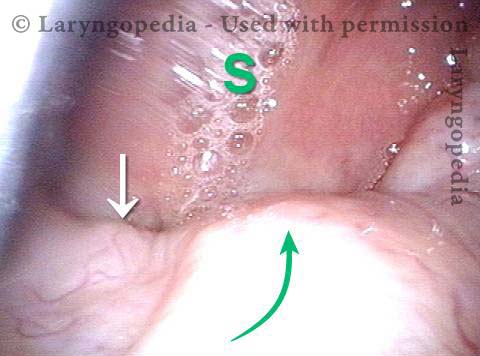
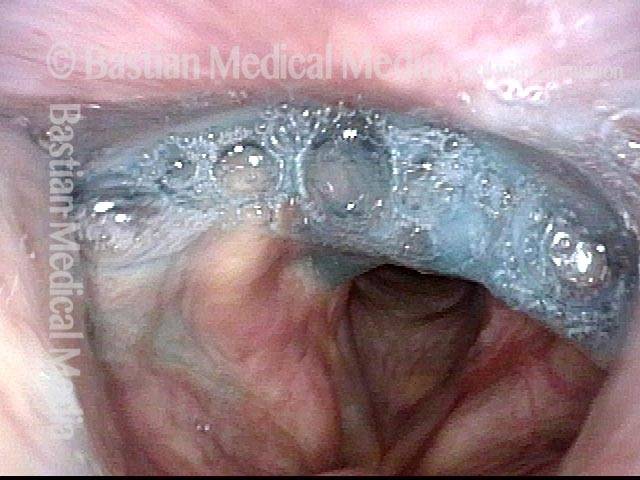
Swallowing blue applesauce (4 of 7)
Swallowing blue applesauce (4 of 7)
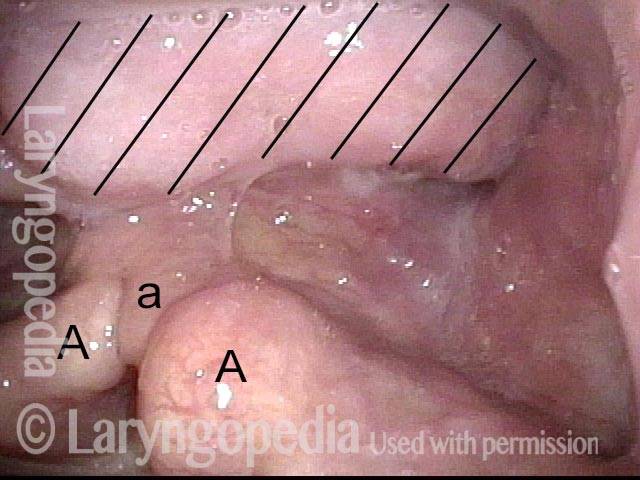
Unilateral pharynx contraction (5 of 7)
Unilateral pharynx contraction (5 of 7)
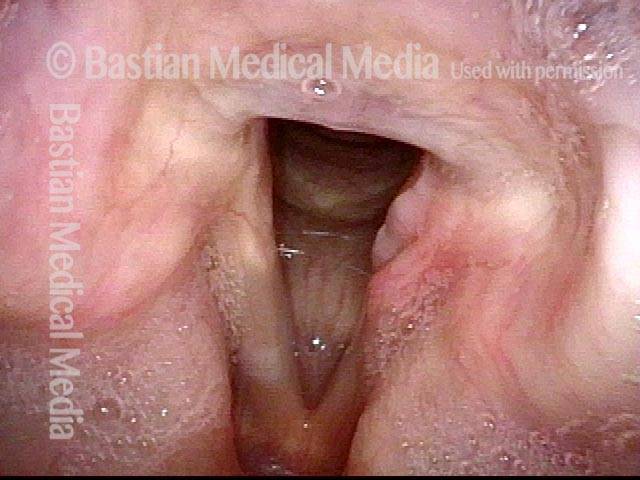
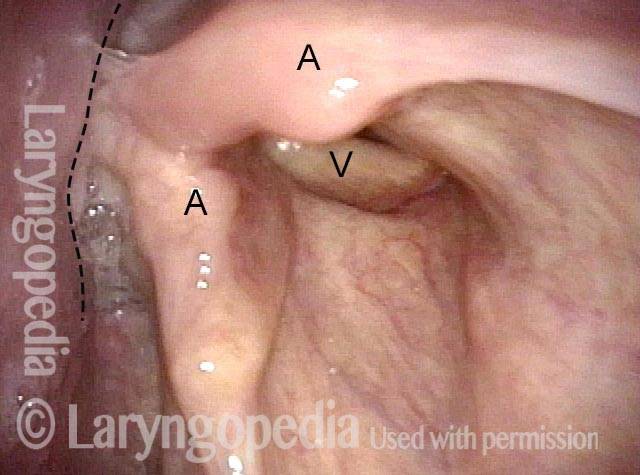
Right vocal cord paresis (6 of 7)
Right vocal cord paresis (6 of 7)
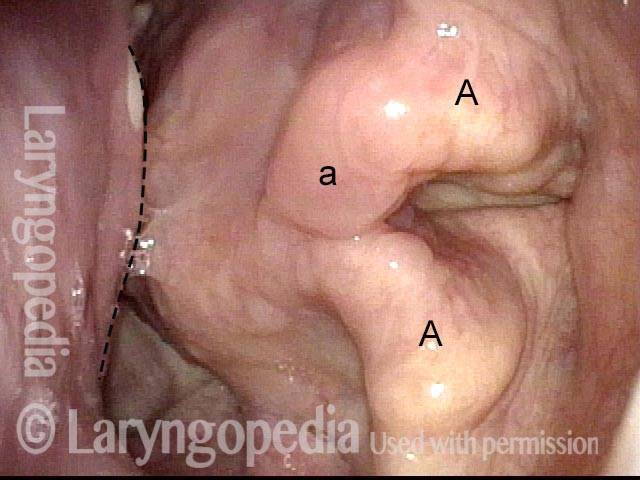
Vocal cord is paretic, not paralyzed (7 of 7)
Vocal cord is paretic, not paralyzed (7 of 7)
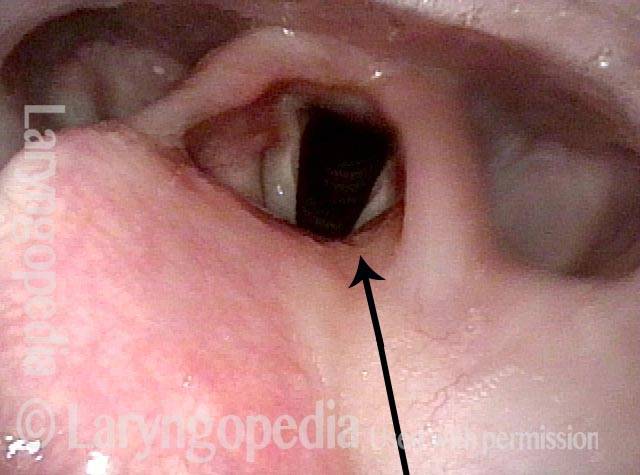
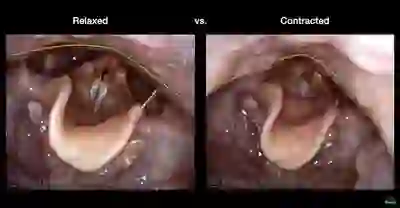
Cricopharyngeal Dysfunction, Before & After Myotomy
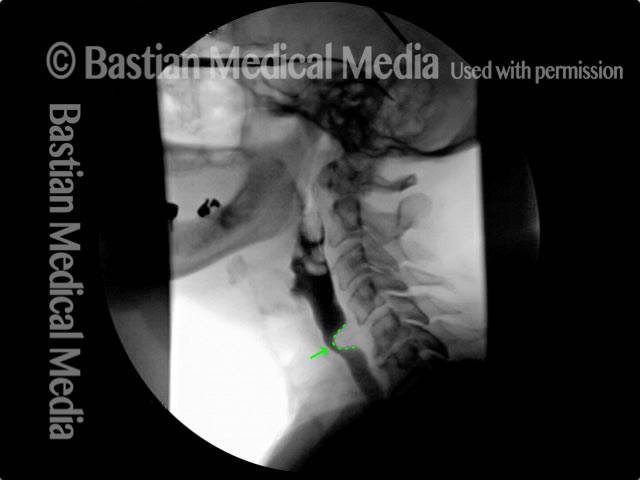
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (2 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (2 of 2)
Example 2
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: before myotomy (1 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (1 of 2)
Cricopharyngeal dysfunction: after myotomy, resolved (1 of 2)
Dysphagia, Due to Tongue Weakness
Dysphagia, due to tongue weakness (1 of 4)
Dysphagia, due to tongue weakness (1 of 4)
Dysphagia, due to tongue weakness (2 of 4)
Dysphagia, due to tongue weakness (2 of 4)
Dysphagia, due to tongue weakness (3 of 4)
Dysphagia, due to tongue weakness (3 of 4)
Dysphagia, due to tongue weakness (4 of 4)
Dysphagia, due to tongue weakness (4 of 4)
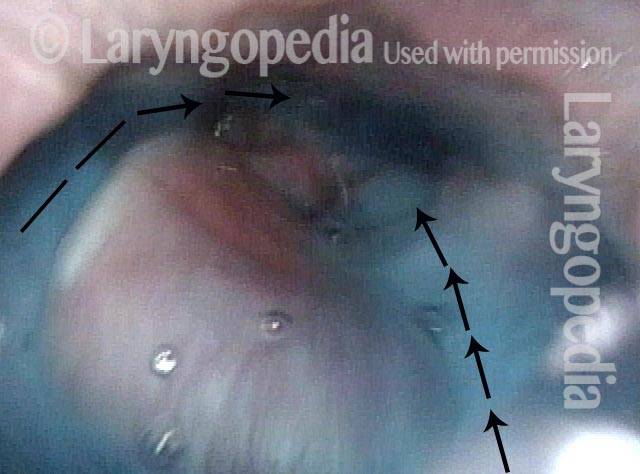
Scarring Diverts Swallowed Materials Directly Into the Larynx
Post tonsillectomy (1 of 4)
Post tonsillectomy (1 of 4)
Closer view (2 of 4)
Closer view (2 of 4)
The “chute” (3 of 4)
The “chute” (3 of 4)
Abnormal diversion (4 of 4)
Abnormal diversion (4 of 4)
Solid Food Dysphagia Due to An Unexplained Benign Mass
Benign mass (1 of 4)
Benign mass (1 of 4)
Closer view (2 of 4)
Closer view (2 of 4)
One week post-op (3 of 4)
One week post-op (3 of 4)
Trumpet maneuver post-op (4 of 4)
Trumpet maneuver post-op (4 of 4)
Share this article
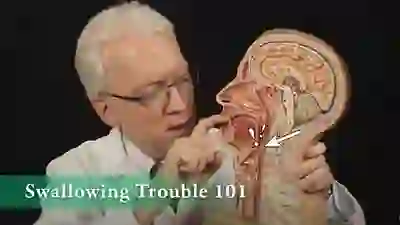
Swallowing Trouble 101
This video gives an overview of how swallowing works, how it can sometimes go wrong (presbyphagia or cricopharyngeal dysfunction), and possible ways to treat those problems (swallowing therapy or cricopharyngeal myotomy).
Videoendoscopic Swallowing Study
This video gives an example of a videoendoscopic swallowing study, which is a method of evaluating a person’s swallowing ability by means of a video-documented physical examination, looking from inside the throat.
Dysphagia vs. Dysphonia vs. Dyesethesia
Dysphagia is the medical term for difficulty swallowing. This may involve discomfort, the sensation of food sticking, or actual impairment of the swallowing process such as when food or liquid “goes down the wrong tube” (aspiration) and induces coughing.
Dysesthesia refers to an abnormal sensation—often unpleasant—such as burning, tingling, or prickling. It may be an exaggerated response to a normal stimulus, or it can occur in the absence of any stimulus at all.
Dysphasia refers to difficulty with language processing (not voice or articulation). There are two broad types:
- Expressive dysphasia, in which the person knows what they want to say but struggles to produce the words.
- Receptive dysphasia, in which the person has trouble understanding spoken or written language. Sometimes both types occur together.
Word Roots
A word-root tip: As you continue learning, you’ll find that understanding word roots is very helpful—and even fun. You’re probably doing this already, but here’s a little encouragement to keep going:
- The prefix dys– means “abnormal.”
- Esthesia refers to sensation—so dysesthesia means abnormal sensation. An– means “without,” so anesthesia means the absence of sensation.
- Phagia refers to swallowing. Add dys– and you get “abnormal swallowing.” Begin with odyno– (pain) and you get odynophagia—”painful swallowing.”
- Phasia refers to language production or understanding. Add dys– and you get “abnormal language processing.”
- Phonia refers to voice, or sound. Add dys– and you get “abnormal voice, or hoarseness.” Add a– and you get “absence of voice”
The more you learn the roots, the easier it is to decode medical terms. So keep looking for those roots—they’ll serve you well!