TA + LCA Paresis
TA + LCA paresis is weakness or paralysis of both the thyroarytenoid (TA) and lateral cricoarytenoid (LCA) muscles of one vocal cord, but with normal function of that cord’s posterior cricoarytenoid (PCA) muscle. The TA muscle “inhabits” the vocal cord and normally provides bulk and internal tone to the cord. The LCA muscle helps to bring the vocal cord to the midline for voice production and, more specifically, to bring the “toe” of the arytenoid cartilage to the midline.
Indicators of TA + LCA Paresis
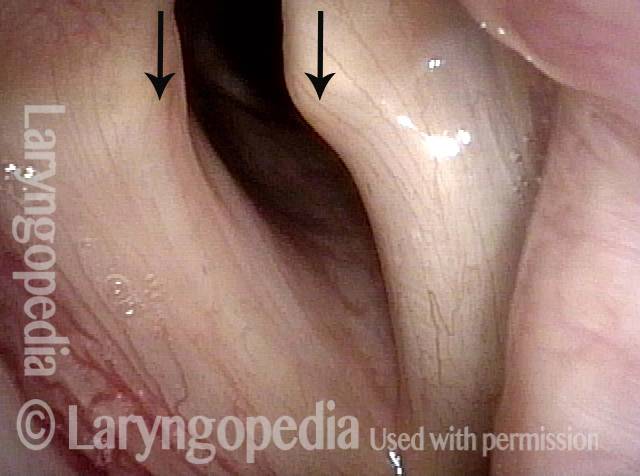
- Movement: Position is normal during breathing, but the vocal cord does not move closer than the intermediate position for voicing. In other words, it is further lateral than the paramedian position one would see with paralysis of all three muscles: TA + LCA + PCA.
- Position and appearance: Due to the TA paralysis, the margin of the cord is slightly concave, the ventricle is capacious, and the conus area below the free margin is lacking in bulk. Due to the LCA paralysis, there is lateral turning of the vocal process. This lateral turning is seen best in low voice, and is a little less apparent with very high voice.
- Appearance during voicing (under strobe lighting): Flaccidity as indicated by increased amplitude of vibration; the lateral excursions become exaggerated and the mucosal wave increases. One may also see chaotic fluttering. The gap between the cords is particularly large because of the unopposed lateral pull of the intact PCA muscle. TA and LCA paresis is often mistaken for complete vocal cord paralysis (TA + LCA + PCA). To avoid this mistake, the examiner must notice this lateral position. The examiner can also try to make any such lateral pulling more evident by asking the patient to inhale sharply or, better yet, to sniff, which exaggerates the abductory movements of the patient’s vocal cords.
- Voice quality: Exceedingly weak and air-wasting. After successful medialization, the obligate falsetto and luffing may disappear, while some of the breathy-pressed quality may persist.
Other variants of vocal cord paresis include LCA-only, TA-only, PCA-only, and IA-only (interarytenoid muscle).
Visual Cues of Paresis Validated by their Change with Recovery!
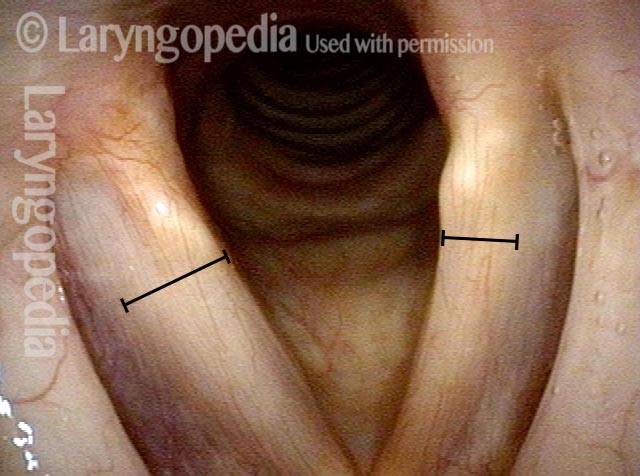
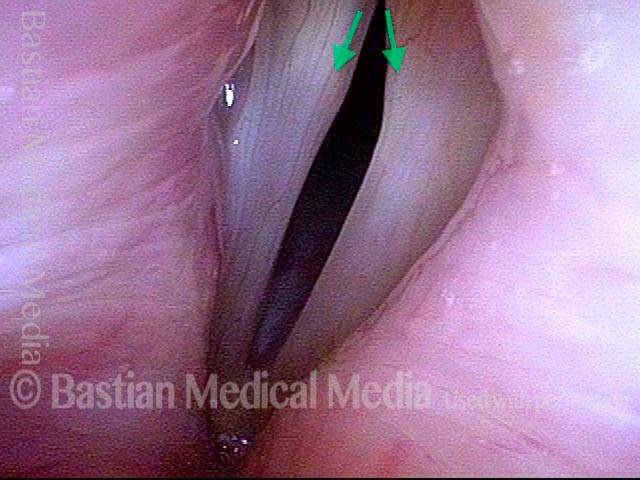
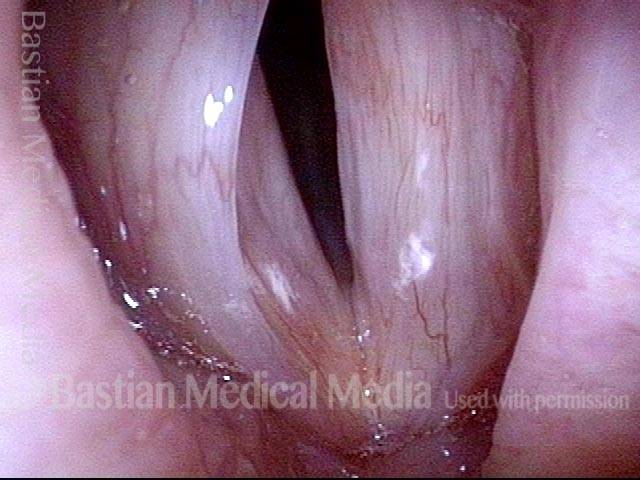
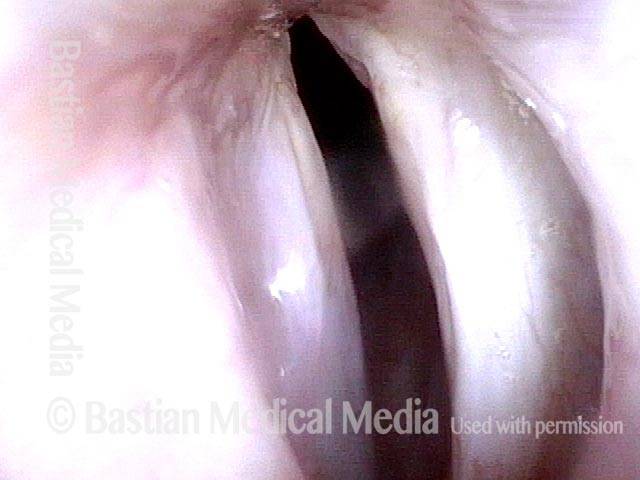
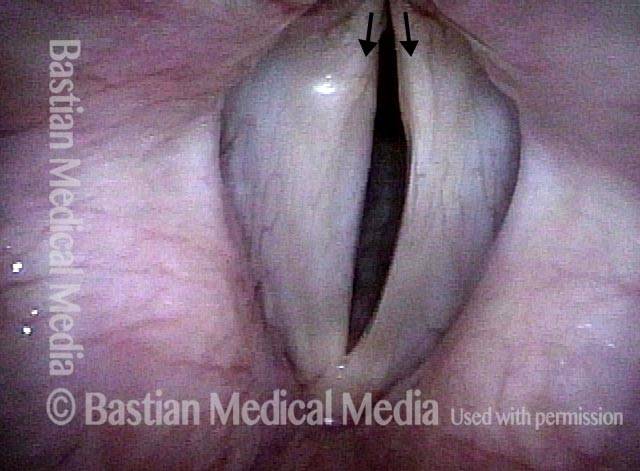
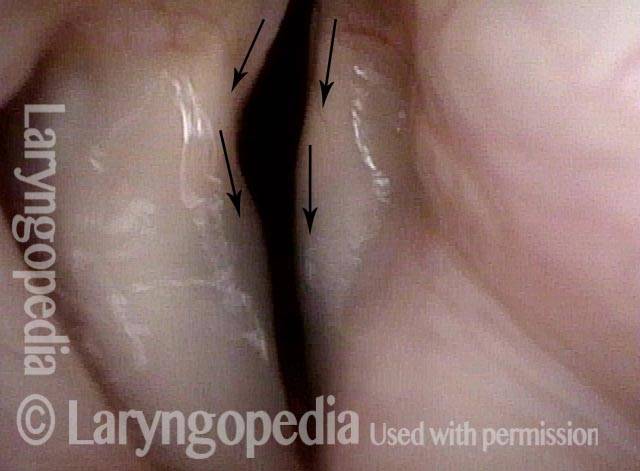
TA weakness (1 of 6)
TA weakness (1 of 6)
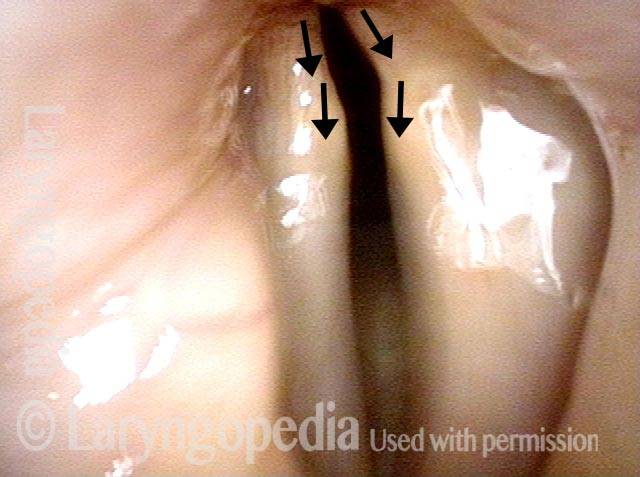
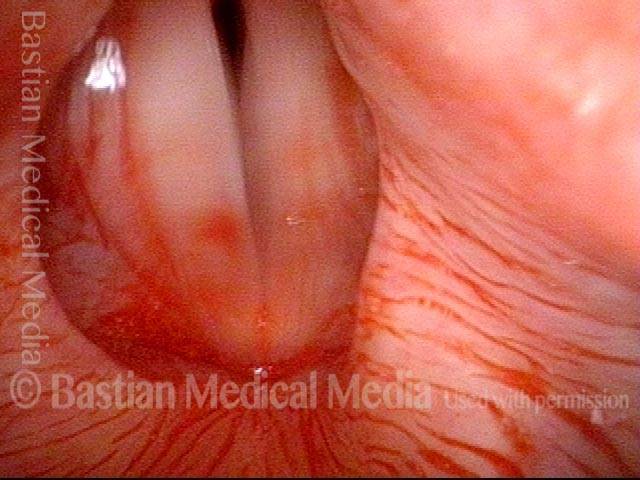
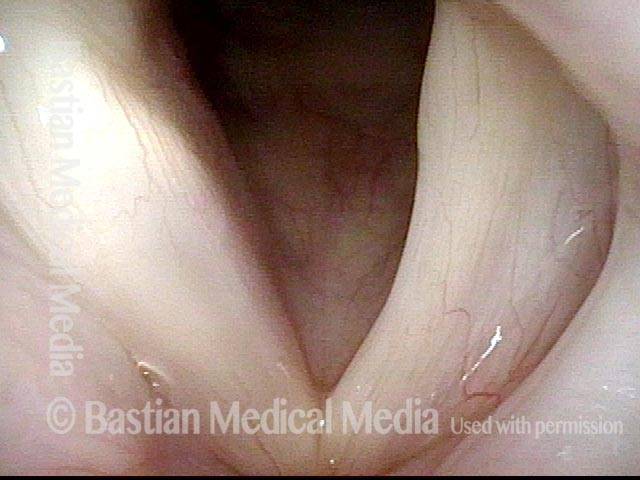
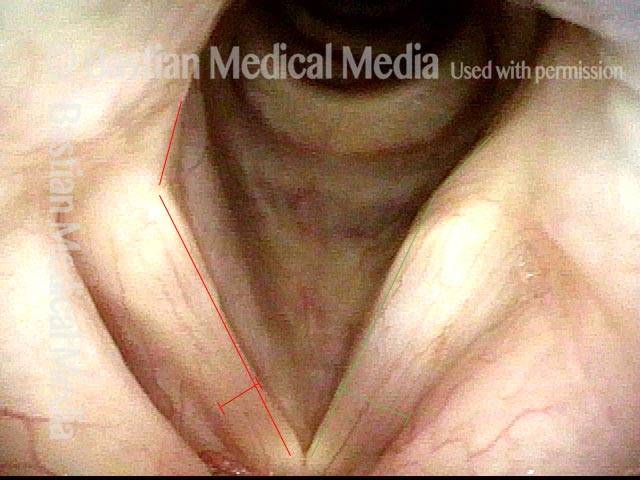
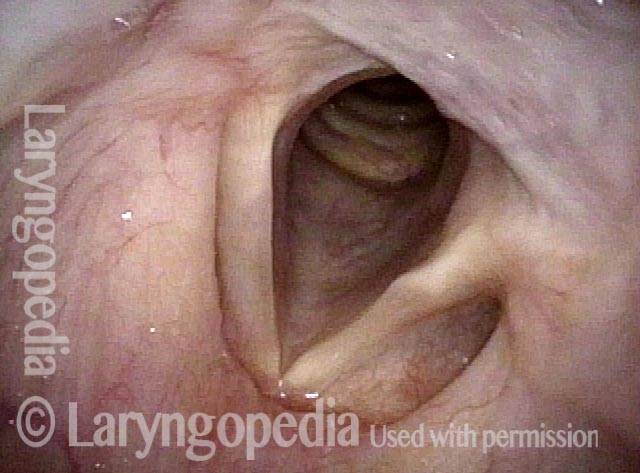
LCA weakness (2 of 6)
LCA weakness (2 of 6)
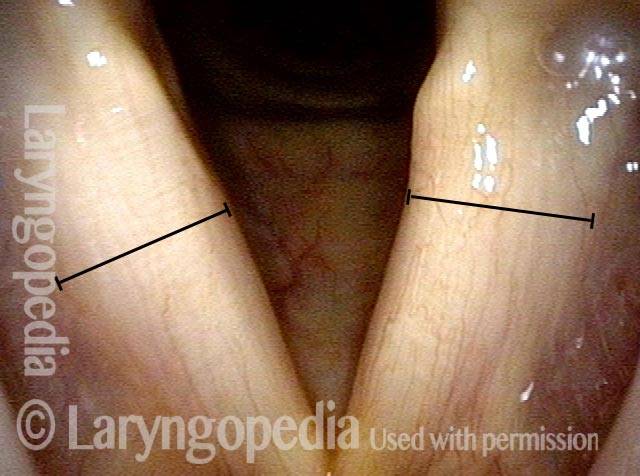
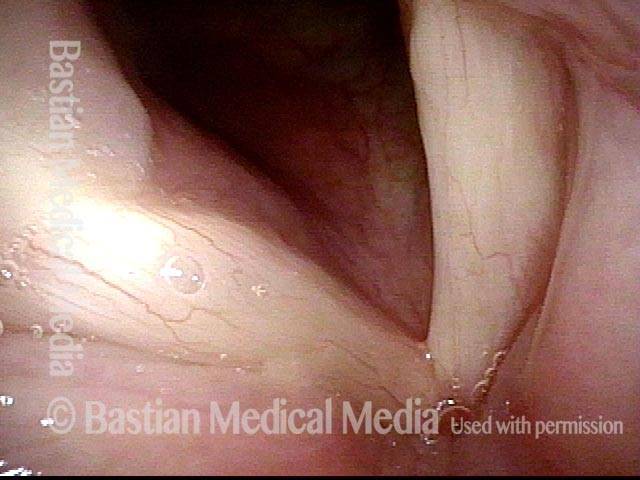
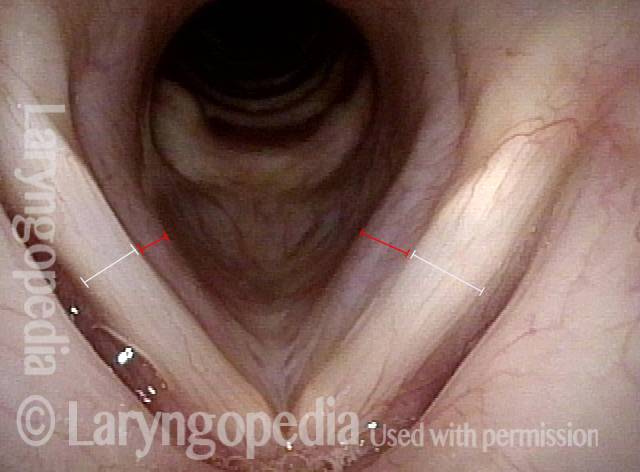
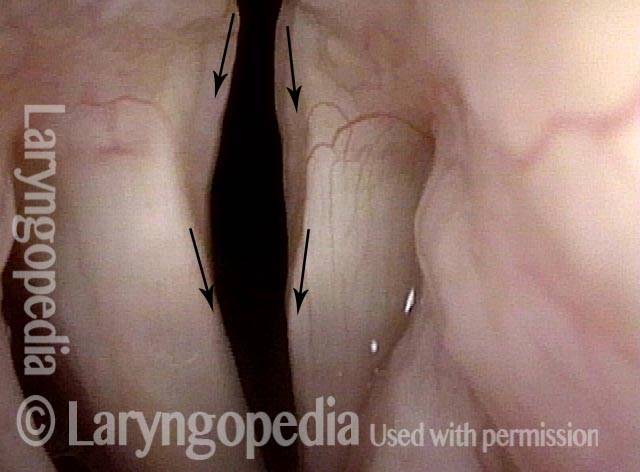
Six weeks later (3 of 6)
Six weeks later (3 of 6)
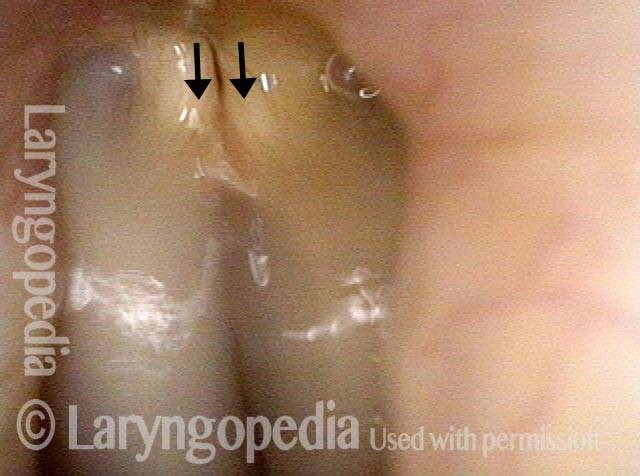
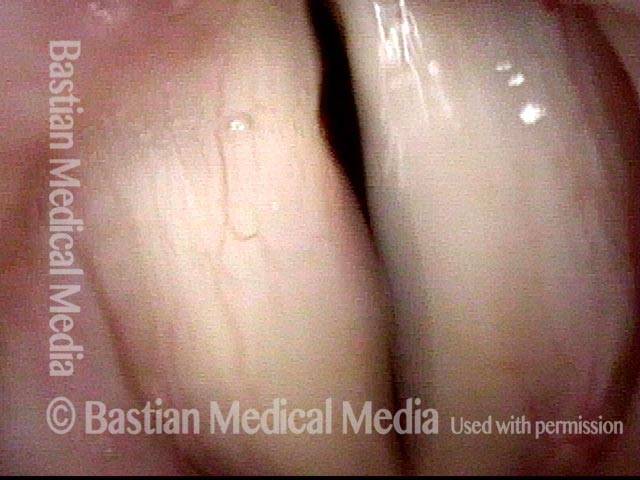
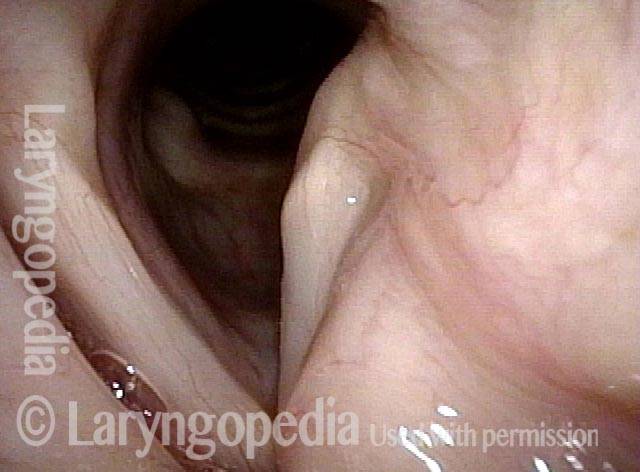
LCA muscle recovered (4 of 6)
LCA muscle recovered (4 of 6)
Closed phase (5 of 6)
Closed phase (5 of 6)
Open phase (6 of 6)
Open phase (6 of 6)
Paresis, TA + LCA, before and after Placement of an Implant
Paresis, TA + LCA (1 of 6)
Paresis, TA + LCA (1 of 6)
Paresis, TA + LCA (2 of 6)
Paresis, TA + LCA (2 of 6)
Paresis, TA + LCA (3 of 6)
Paresis, TA + LCA (3 of 6)
Paresis, TA + LCA: 1 week after implant is placed (4 of 6)
Paresis, TA + LCA: 1 week after implant is placed (4 of 6)
Paresis, TA + LCA: 3 months after implant is placed (5 of 6)
Paresis, TA + LCA: 3 months after implant is placed (5 of 6)
Paresis, TA + LCA: 3 months after implant is placed (6 of 6)
Paresis, TA + LCA: 3 months after implant is placed (6 of 6)
Paresis, TA + LCA, before and after Injection of Voice Gel
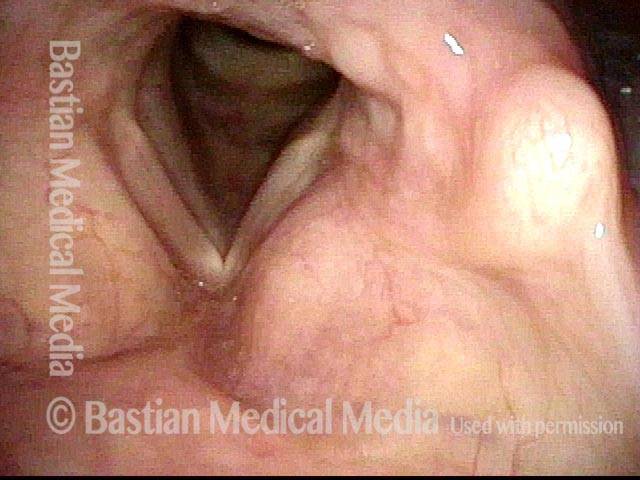
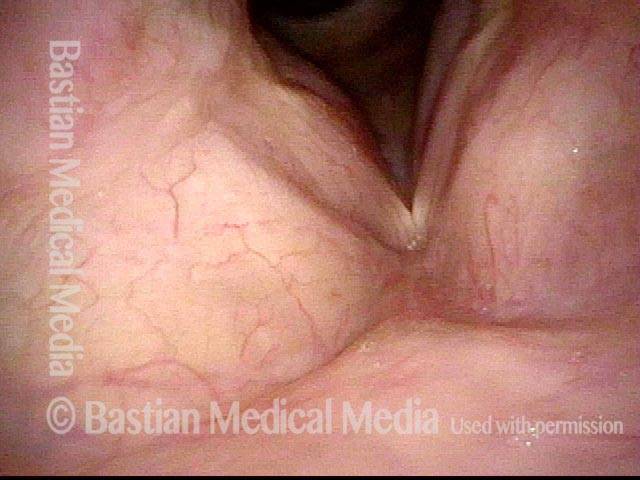
Normally functioning PCA muscle (1 of 8)
Normally functioning PCA muscle (1 of 8)
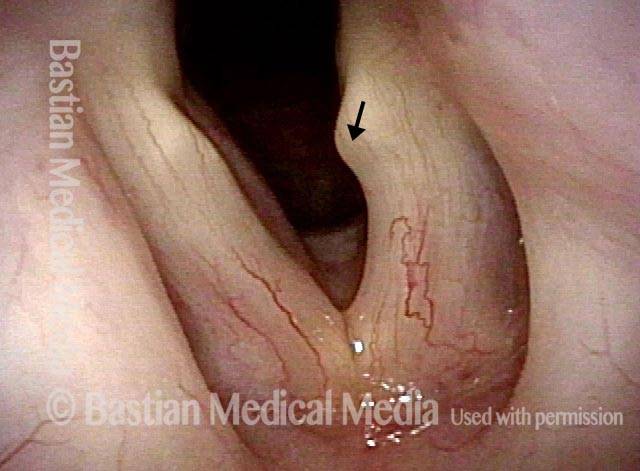
Paresis, TA + LCA (2 of 8)
Paresis, TA + LCA (2 of 8)
Paresis, TA + LCA (3 of 8)
Paresis, TA + LCA (3 of 8)
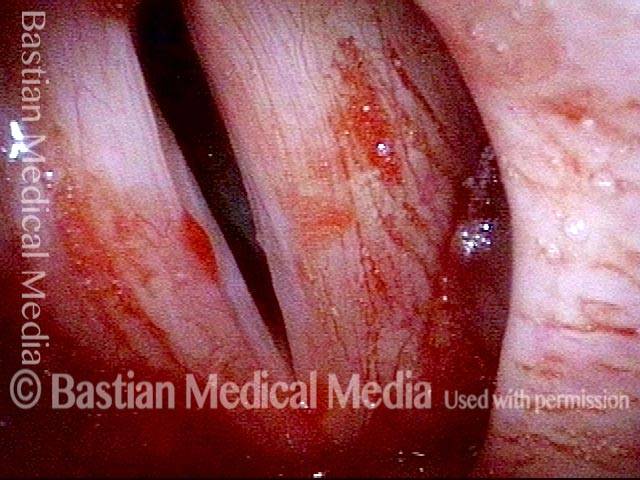
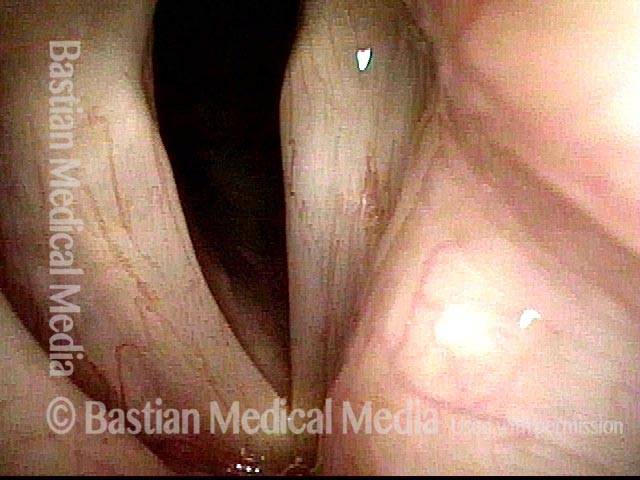
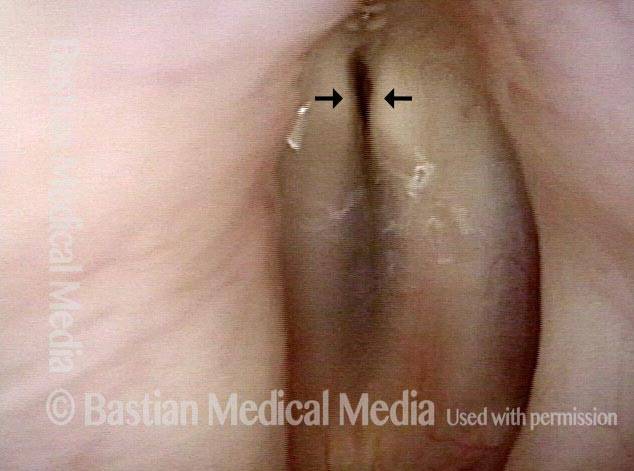
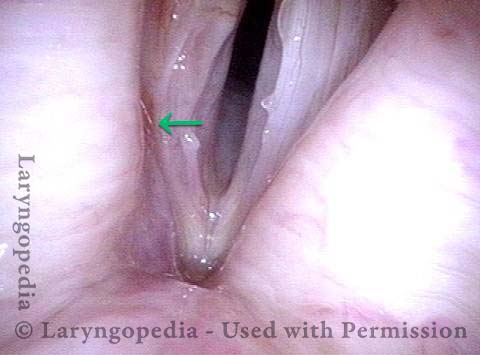
Lateral buckling (4 of 8)
Lateral buckling (4 of 8)
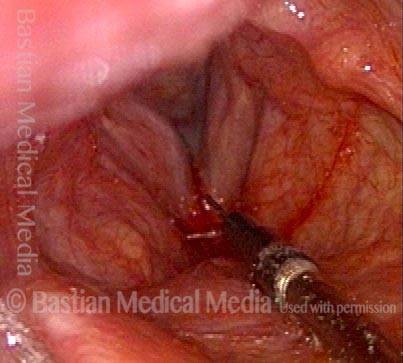
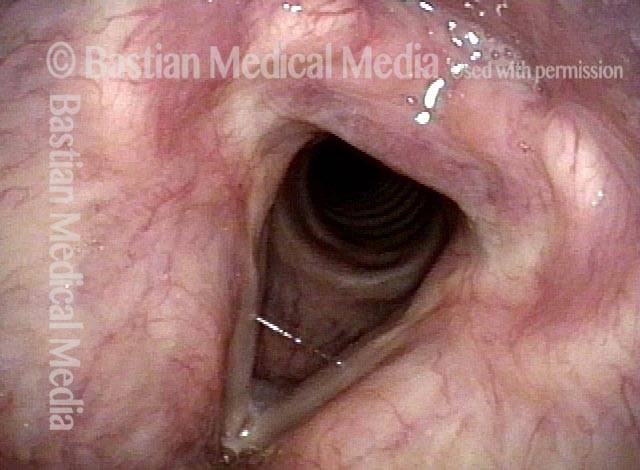
Voice gel injection (5 of 8)
Voice gel injection (5 of 8)
After voice gel injection (6 of 8)
After voice gel injection (6 of 8)
After injection (7 of 8)
After injection (7 of 8)
Strobe light after injection (8 of 8)
Strobe light after injection (8 of 8)
Example 2
Paresis, TA + LCA (1 of 5)
Paresis, TA + LCA (1 of 5)
Paresis, TA + LCA (2 of 5)
Paresis, TA + LCA (2 of 5)
Voice gel injection (3 of 5)
Voice gel injection (3 of 5)
1 month after injection (4 of 5)
1 month after injection (4 of 5)
Phonation 1 month after injection (5 of 5)
Phonation 1 month after injection (5 of 5)
Example 3
TA + LCA paresis (1 of 4)
TA + LCA paresis (1 of 4)
Breathy voice (2 of 4)
Breathy voice (2 of 4)
Voice gel injection (3 of 4)
Voice gel injection (3 of 4)
Injection complete (4 of 4)
Injection complete (4 of 4)
TA + LCA Paresis
TA + LCA paresis (1 of 4)
TA + LCA paresis (1 of 4)
Weak left vocal cord (2 of 4)
Weak left vocal cord (2 of 4)
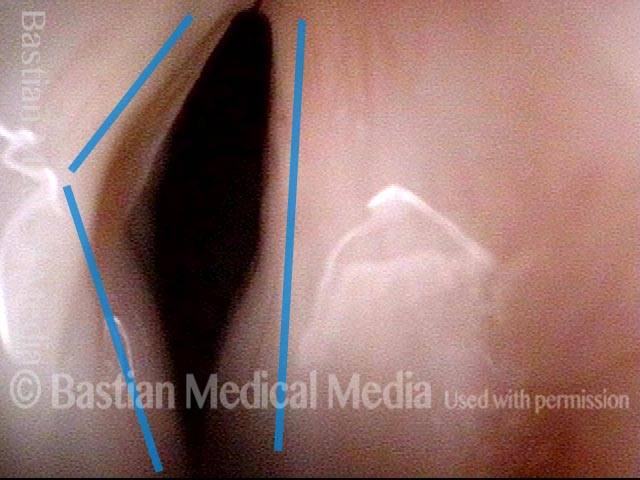
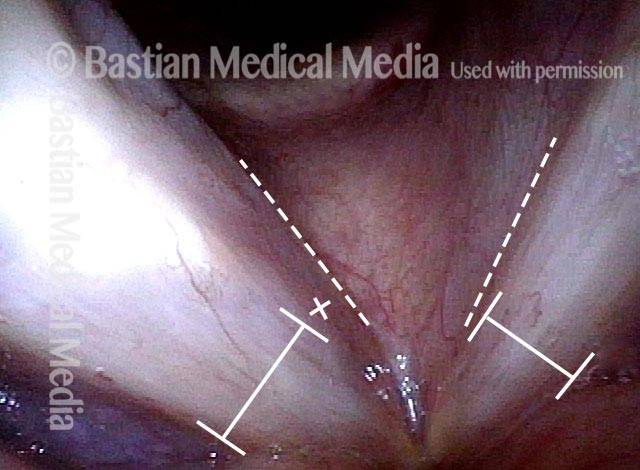
Vocal process points laterally (3 of 4)
Vocal process points laterally (3 of 4)
Strobe light during phonation (4 of 4)
Strobe light during phonation (4 of 4)
Paresis, TA + LCA, with Recovery
Paresis, TA + LCA, with recovery (1 of 4)
Paresis, TA + LCA, with recovery (1 of 4)
Paresis, TA + LCA, with recovery (2 of 4)
Paresis, TA + LCA, with recovery (2 of 4)
Paresis, TA + LCA, with recovery (3 of 4)
Paresis, TA + LCA, with recovery (3 of 4)
Paresis, TA + LCA, with recovery (4 of 4)
Paresis, TA + LCA, with recovery (4 of 4)
Paresis, TA + LCA, before and after Medialization
Paresis, TA + LCA (1 of 7)
Paresis, TA + LCA (1 of 7)
Paresis, TA + LCA (2 of 7)
Paresis, TA + LCA (2 of 7)
Paresis, TA + LCA (3 of 7)
Paresis, TA + LCA (3 of 7)
Paresis, TA + LCA (4 of 7)
Paresis, TA + LCA (4 of 7)
Paresis, TA + LCA: after medialization (5 of 7)
Paresis, TA + LCA: after medialization (5 of 7)
Paresis, TA + LCA: after medialization (6 of 7)
Paresis, TA + LCA: after medialization (6 of 7)
Paresis, TA + LCA: after medialization (7 of 7)
Paresis, TA + LCA: after medialization (7 of 7)
TA + PCA-only Paresis
Breathing position (1 of 5)
Breathing position (1 of 5)
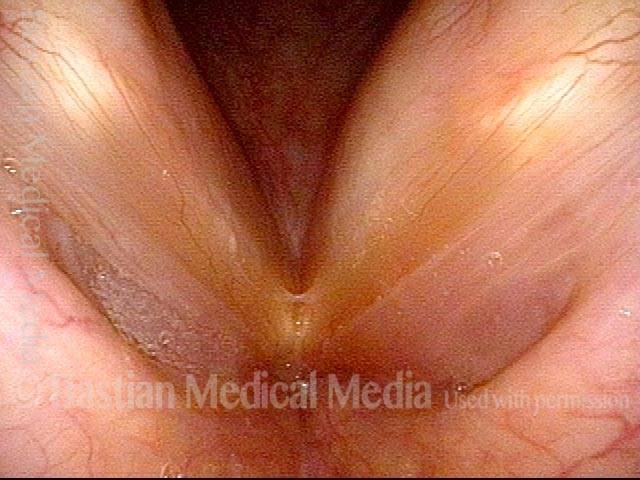
Phonatory position (2 of 5)
Phonatory position (2 of 5)
Voice gel injection (3 of 5)
Voice gel injection (3 of 5)
Plumped vocal cord (4 of 5)
Plumped vocal cord (4 of 5)
After voice gel injection (5 of 5)
After voice gel injection (5 of 5)
Example 2
Breathing position (1 of 6)
Breathing position (1 of 6)
Phonation (2 of 6)
Phonation (2 of 6)
Closed phase, A3 (3 of 6)
Closed phase, A3 (3 of 6)
Open phase, A3 (4 of 6)
Open phase, A3 (4 of 6)
Closed phase, C3 (5 of 6)
Closed phase, C3 (5 of 6)
Open phase, C3 (6 of 6)
Open phase, C3 (6 of 6)
Telescope Panoramic Views are Routinely not Adequate for Assessing Paresis!
TA weakness (1 of 4)
TA weakness (1 of 4)
Prephonatory instant (2 of 4)
Prephonatory instant (2 of 4)
LCA not working (3 of 4)
LCA not working (3 of 4)
Phonatory blur (4 of 4)
Phonatory blur (4 of 4)
Classic TA + LCA-only Paresis, Right Vocal Cord
Atrophy of the conus (1 of 5)
Atrophy of the conus (1 of 5)
Inability to adduct (2 of 5)
Inability to adduct (2 of 5)
LCA weakness (3 of 5)
LCA weakness (3 of 5)
Further review (4 of 5)
Further review (4 of 5)
Luffing (5 of 5)
Luffing (5 of 5)
Breathing Tube Injury—A Rare Complication of Intubation for General Anesthesia
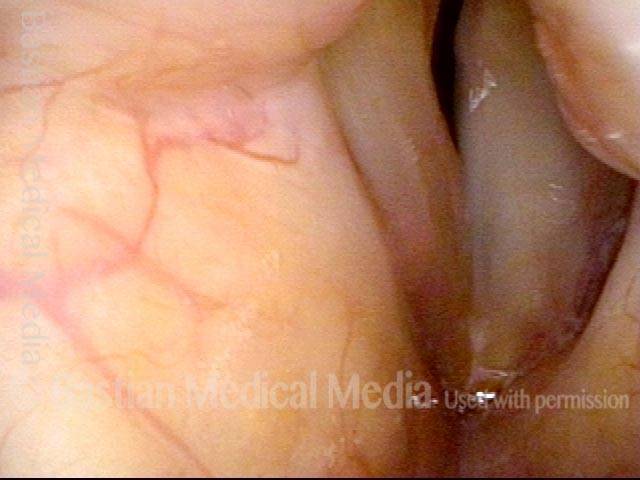
Inflamed vocal cord (1 of 5)
Inflamed vocal cord (1 of 5)
Closer view (2 of 5)
Closer view (2 of 5)
Scarring from intubation tube (3 of 5)
Scarring from intubation tube (3 of 5)
Mucosal Injury (4 of 5)
Mucosal Injury (4 of 5)
Flaccidity of right vocal cord (5 of 5)
Flaccidity of right vocal cord (5 of 5)
Conclusion: While we try to explain abnormality due to one cause, here, the patient has a mucosal injury and paresis of right TA and LCA muscles, which can also follow intubation. This explains why the initial postop voice was so weak and whispery, and also the rapid partial improvement. This voice will likely continue to improve and be very functional as a speaking voice. Fortunately, this person is not a singer, as clarity especially in upper notes, will likely be remain impaired even after full recovery.
PCA working; TA and LCA Are not in this Paresis Subtype
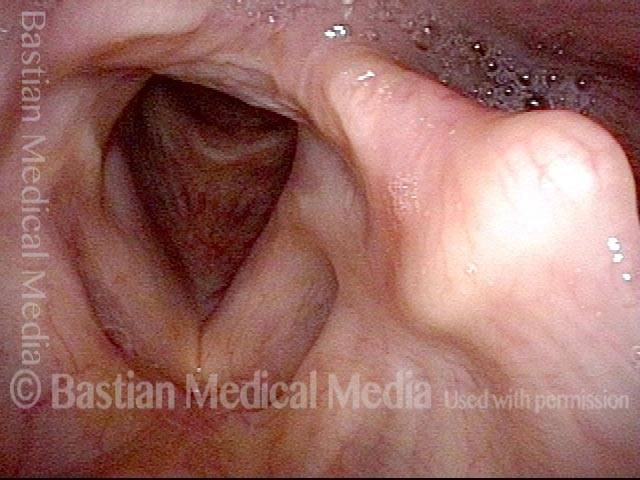
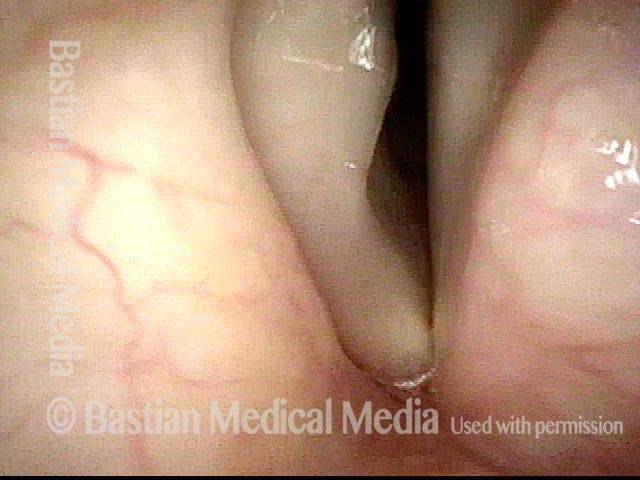
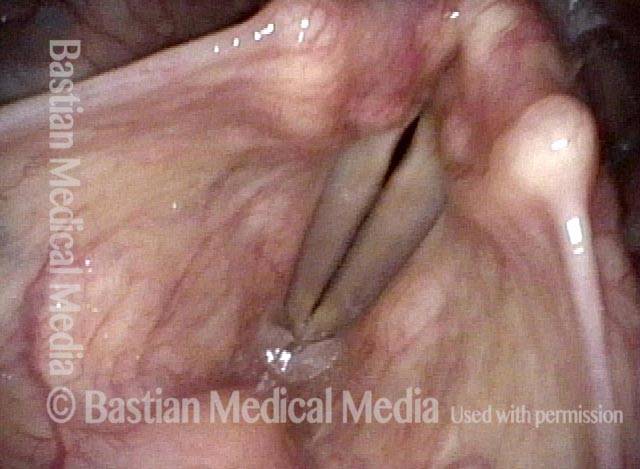
Capacious ventricle, bowed margin (1 of 4)
Capacious ventricle, bowed margin (1 of 4)
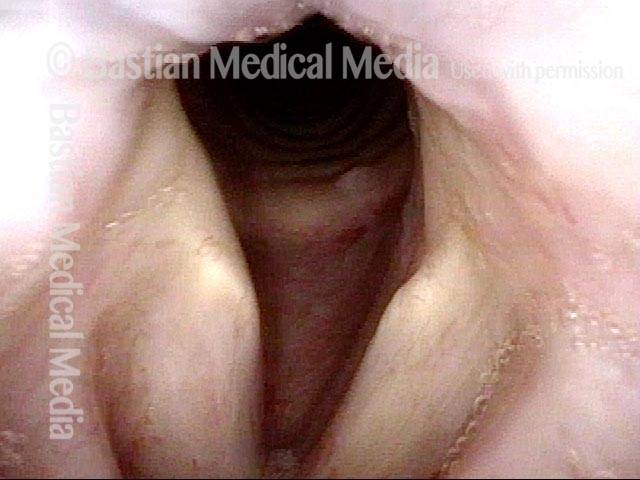
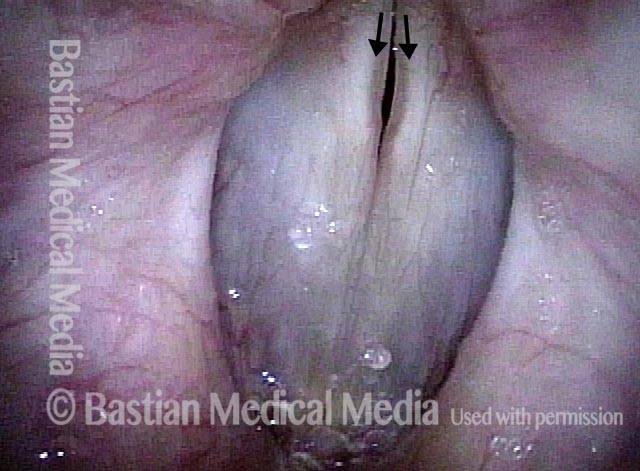
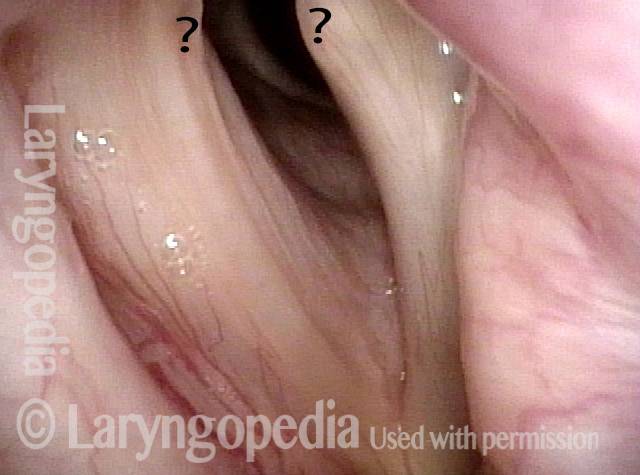
Pre-phonatory (2 of 4)
Pre-phonatory (2 of 4)
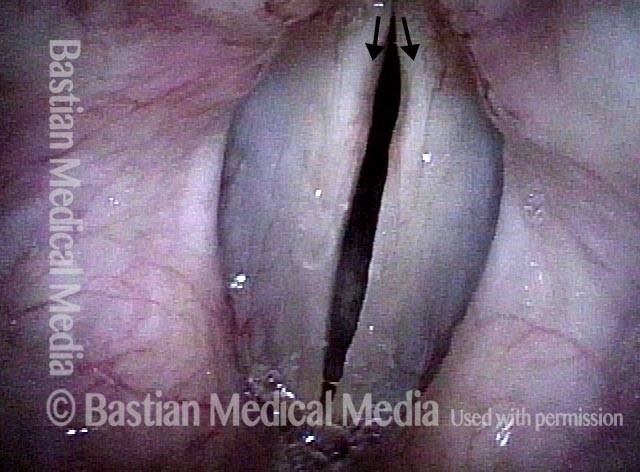
Posterior view (3 of 4)
Posterior view (3 of 4)
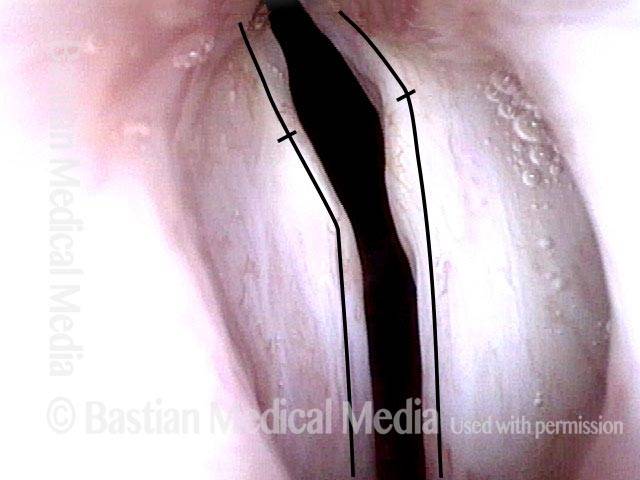
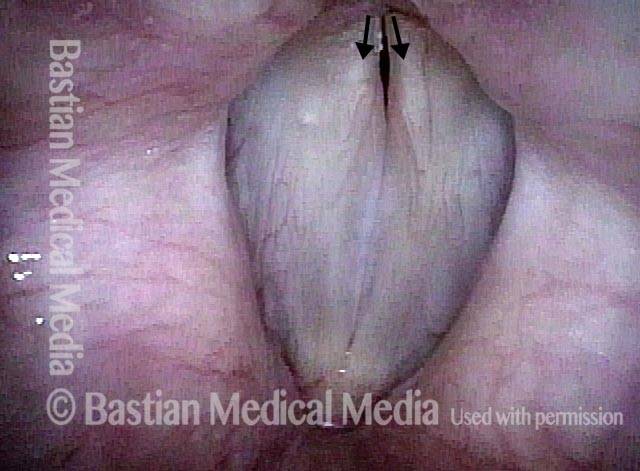
Right TA + LCA-only paresis (4 of 4)
Right TA + LCA-only paresis (4 of 4)
Share this article