Tracheoesophageal Voice Prosthesis (TEP)
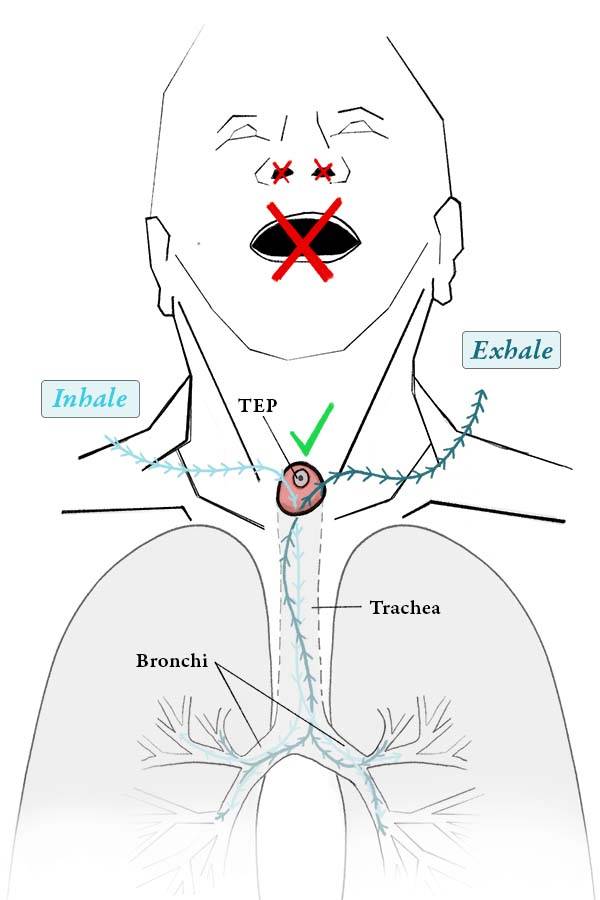
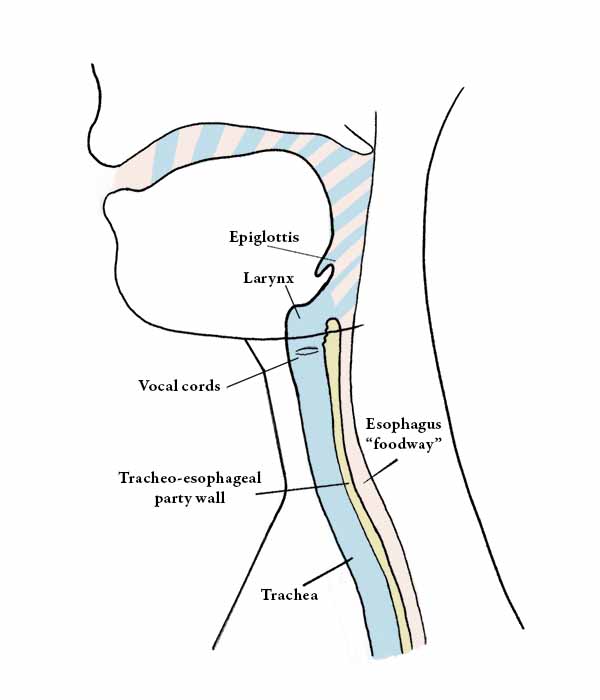
Tracheoesophageal voice prosthesis (TEP) is a device that is placed in the wall that separates the trachea and esophagus in order to enable a total laryngectomy patient to make voice.
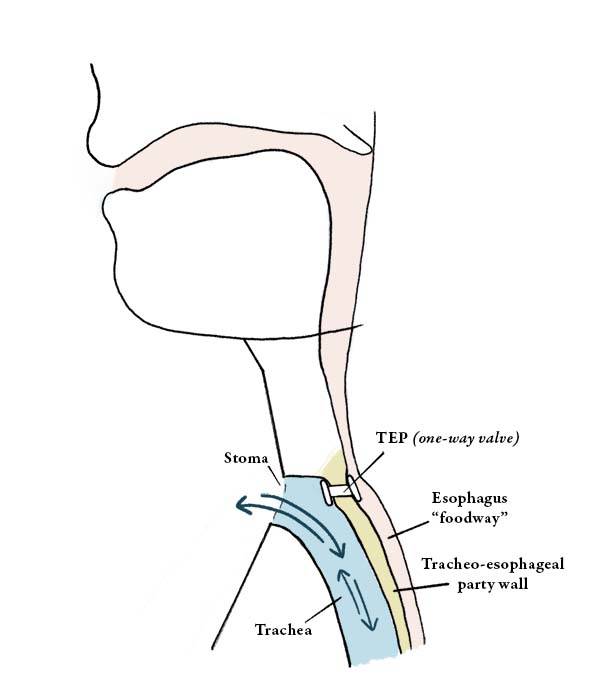
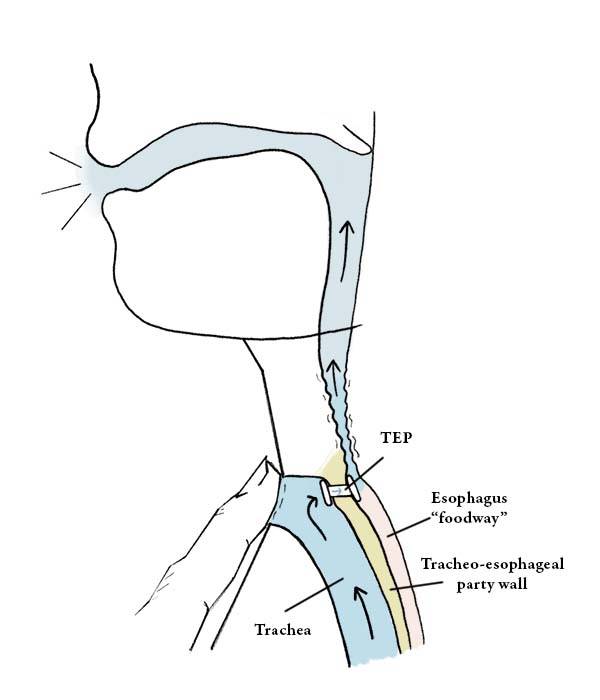
The TEP uses a one-way valve to let air pushed up from the lungs to pass through from the trachea and enter the esophagus, causing the walls of the esophagus to vibrate as a new voice, but without letting food or liquids to pass through the other way, from the esophagus to the trachea.
The Need for a TEP
A patient who undergoes a total laryngectomy procedure will have the entire larynx removed and the end of the trachea redirected to an opening—called a stoma—created in the front of the neck (see figures above).
The result is that the patient can now breathe through this stoma, but would be unable to make any voice, because the larynx (voice box) is gone, and the air for voicing that once passed up through the larynx, causing the vocal cords to vibrate and thereby make voice, now simply exits the trachea at the stoma. Such a patient can obtain an alternate voice by using a TEP device.
The Placement of a TEP
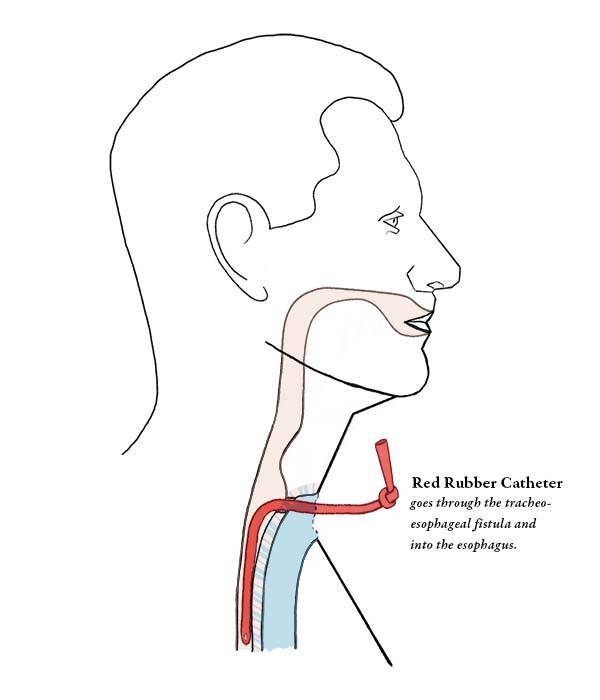
In order to place a TEP device into the wall that separates the trachea and esophagus (the tracheoesophageal party wall), a puncture must first be made, into which the device can fit. This puncture can be made during the laryngectomy procedure (primary tracheoesophageal puncture) or afterward in a separate procedure (secondary tracheoesophageal puncture), typically some weeks after the laryngectomy.
Some clinicians prefer to place the device itself as part of the primary puncture. Others first place a catheter to hold the puncture open and allow for tube feedings while the pharynx heals, and then they place the actual device in an office setting 10 days or more later.
The Use of a TEP
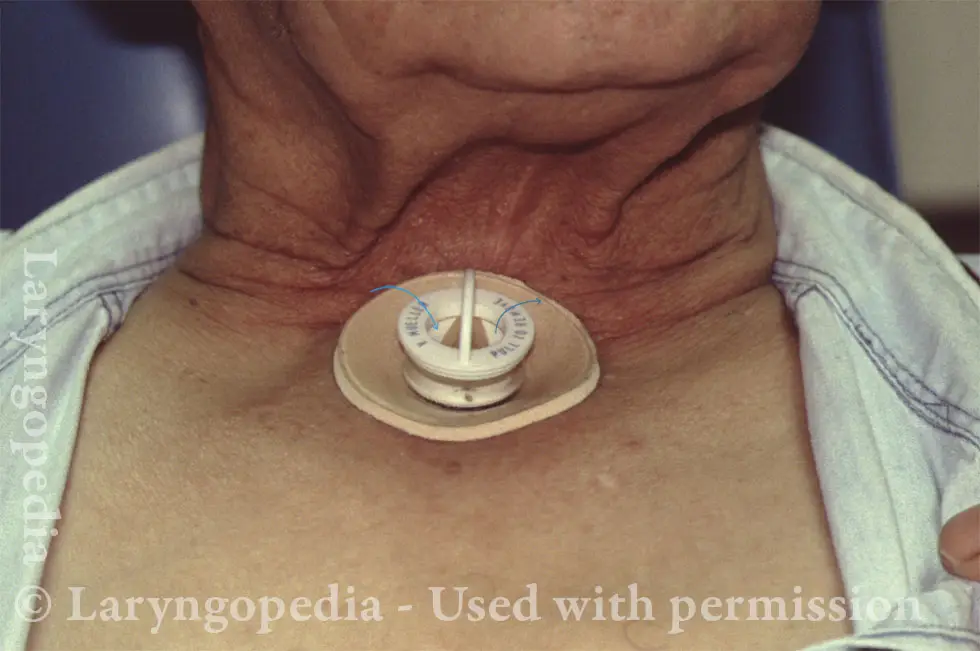
When a patient with a TEP device wants to speak, he or she must momentarily cover the stoma in the front of the neck, so that air coming up from the lungs is redirected through the TEP and into the esophagus to make voice. Some patients will simply cover the stoma as needed with their thumb, if their stoma is normally left entirely open, or is only concealed from view with a small, unobtrusive, breathable cloth.
More commonly, however, the patient’s stoma is fitted with a housing, into which is placed a heat and moisture exchanger (HME); in these cases, the HME, which looks like a flat, plastic button, can be pushed as needed to block the stoma and enable voicing. Whatever the case, speaking with a TEP device is a learned skill and requires training through speech therapy.
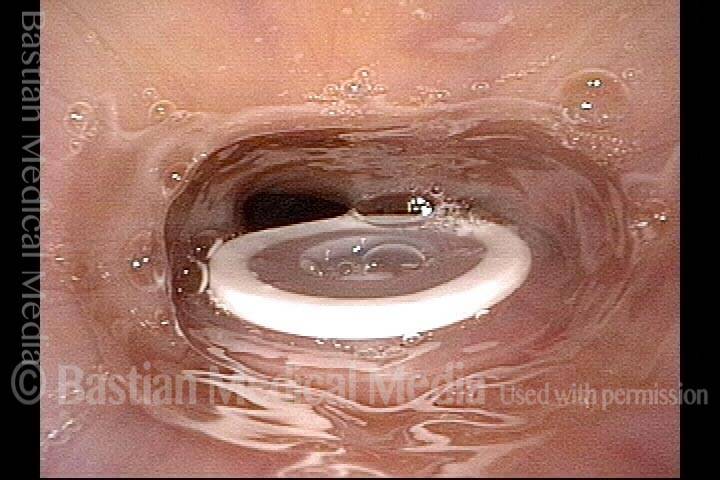
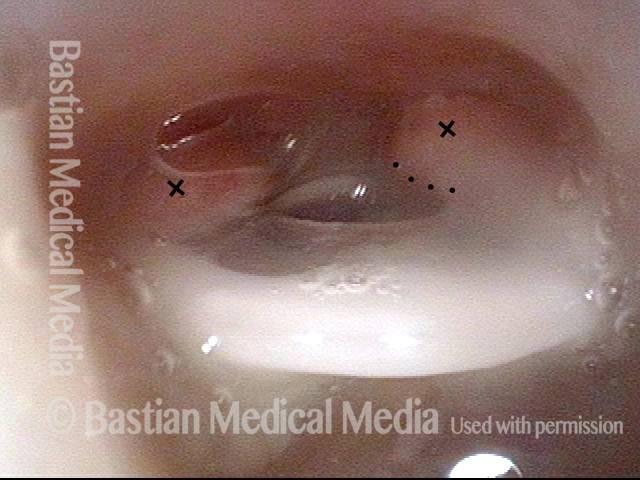
Tracheoesophageal voice prosthesis (1 of 4)
Tracheoesophageal voice prosthesis (1 of 4)
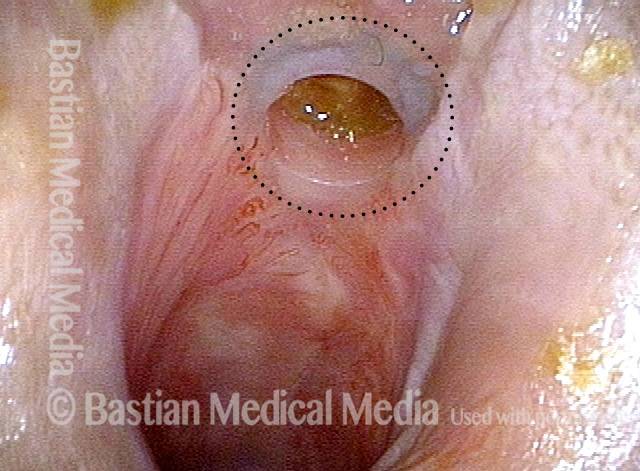
Tracheoesophageal voice prosthesis (2 of 4)
Tracheoesophageal voice prosthesis (2 of 4)
Tracheoesophageal voice prosthesis, corrected fitting (3 of 4)
Tracheoesophageal voice prosthesis, corrected fitting (3 of 4)
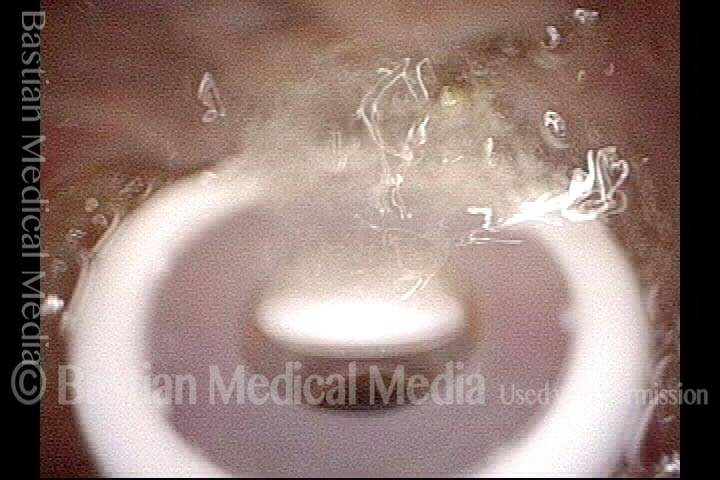
Tracheoesophageal voice prosthesis, during voicing (4 of 4)
Tracheoesophageal voice prosthesis, during voicing (4 of 4)
Hands-Free Tracheoesophageal Voice
After laryngectomy, most people prefer to glue a small voice button over the stoma that they push when they wish to speak. When not pushed, the button springs up and allows air into the trachea.
This person is instead using a hands-free valve. He can initiate voice by beginning each sentence with a little “kick” of exhaled air that closes a flexible diaphragm and diverts pulmonary air through the TEP device and into the pharyngoesophageal segment.
Hands-Free TEP when breathing
Here is the hands-free device during quiet breathing. It is attached with a biological glue to the skin that surrounds the stoma. When this man breathes in, the path of air follows the arrows into the “open white crescent” on either side of the tan flutter valve. When he breathes out normally, the air travels though the same space in the opposite direction.

Hands-free TEP during voicing
If he “kicks” the air out slightly, the curled diaphragm unfurls in an outward direction and plugs the passage, so that air is diverted through the tracheoesophageal prosthesis (not seen here). The result: hands-free tracheoesophageal voice.
TEP Voicing
Hypopharynx of a tracheoesophageal voice prosthesis patient (1 of 4)
Hypopharynx of a tracheoesophageal voice prosthesis patient (1 of 4)
Hypopharynx, as the tracheoesophageal voice prosthesis patient makes voice (2 of 4)
Hypopharynx, as the tracheoesophageal voice prosthesis patient makes voice (2 of 4)
Tracheoesophageal voice prosthesis (3 of 4)
Tracheoesophageal voice prosthesis (3 of 4)
Tracheoesophageal voice prosthesis, as the patient makes voice (4 of 4)
Tracheoesophageal voice prosthesis, as the patient makes voice (4 of 4)
TEP’s that Want to Become Buried
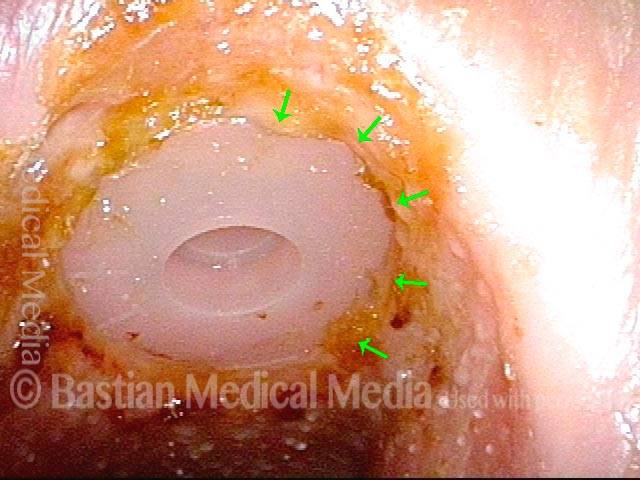
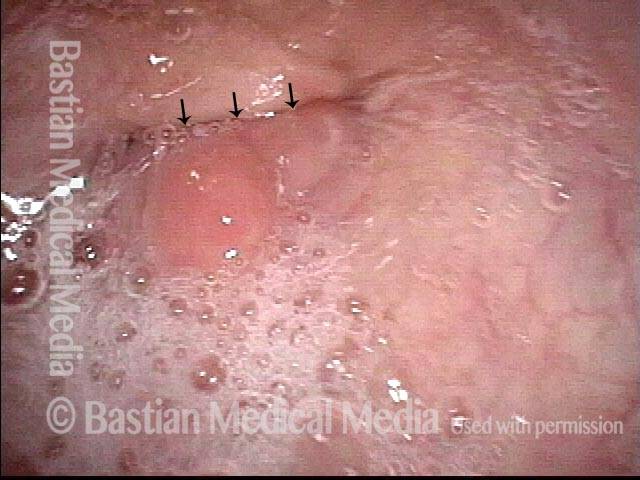
TEP buried (1 of 4)
TEP buried (1 of 4)
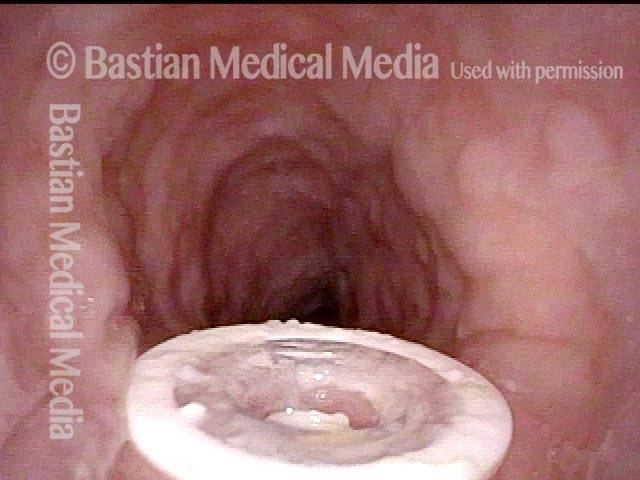
Re-inserted and re-positioned TEP (2 of 4)
Re-inserted and re-positioned TEP (2 of 4)
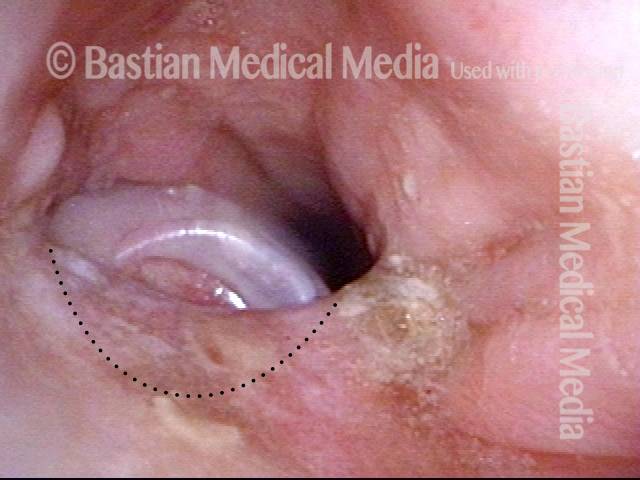
Tissue overgrowing flange (3 of 4)
Tissue overgrowing flange (3 of 4)
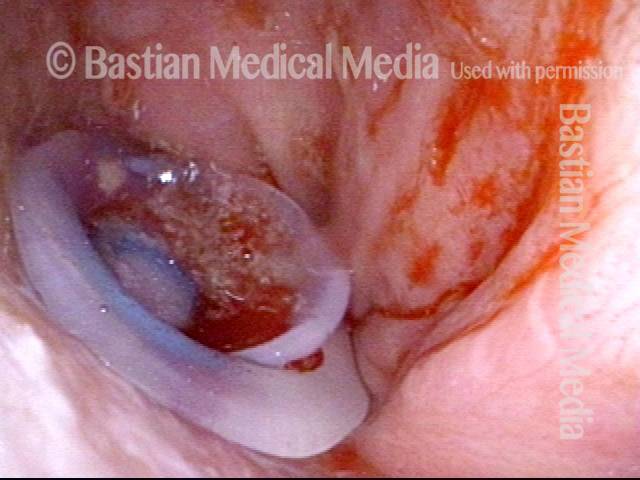
Flange partially buried (4 of 4)
Flange partially buried (4 of 4)
How the One-way Flapper Valve Works in a TEP Prosthesis
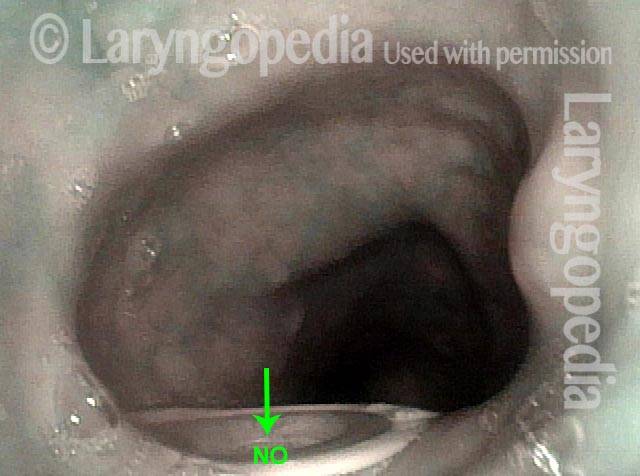
Food and liquid blocked from trachea (1 of 3)
Food and liquid blocked from trachea (1 of 3)
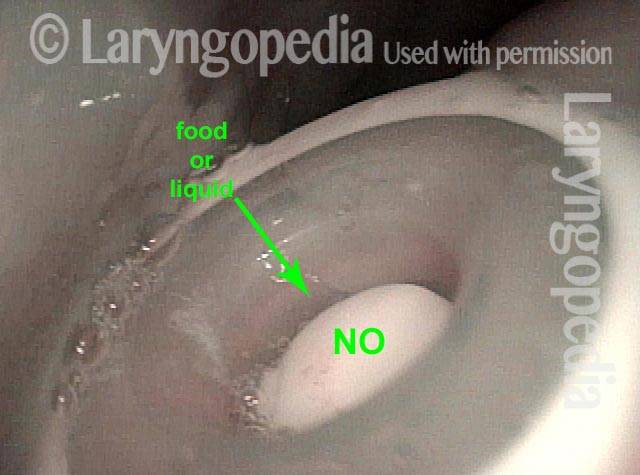
Closer look at closed valve (2 of 3)
Closer look at closed valve (2 of 3)
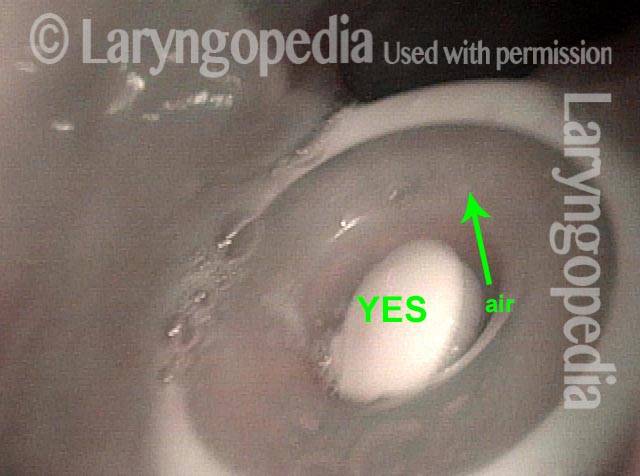
Opened valve (3 of 3)
Opened valve (3 of 3)
Share this article