Vocal Underdoer Syndrome: When Voice Rest or Restraint Is Counterproductive
Introduction
For a voice clinician, it is helpful not only to place each medical disorder in its own unique diagnostic “basket,” but also to search for organizing concepts that might show what certain disorders have in common with each other.
For example, vocal nodules, vocal polyps, and vocal fold hemorrhage are three distinct diagnoses that could be found in three different people. Yet these “different” diagnoses can be understood and addressed better when placed together under a common banner: the vocal overdoer syndrome.1 That is, since each of these kinds of vocal fold injuries (along with other injuries like capillary ectasia and epidermoid cyst) arises from excessive voice use2 , it is most helpful, when dealing with such an injury, to view the vocal overdoer syndrome as (almost always, but not exclusively) the primary diagnosis and the resultant injury as the secondary diagnosis.
Although it is now widely understood that many types of vocal fold injuries are caused by excessive voice use, it remains less clear to many voice clinicians that disorders can also occur because of vocal underuse. A person might underuse one’s voice for a variety of reasons: a personality that limits voice use; a false conclusion one has jumped to about his or her voice, triggering inappropriate, self-imposed voice rest; well-intentioned but misguided medical advice to conserve the voice; or a combination of these.
All of these scenarios, when they lead to a voice problem, fall under the banner of what we call the vocal underdoer syndrome.
Background: vocal underdoers versus vocal overdoers
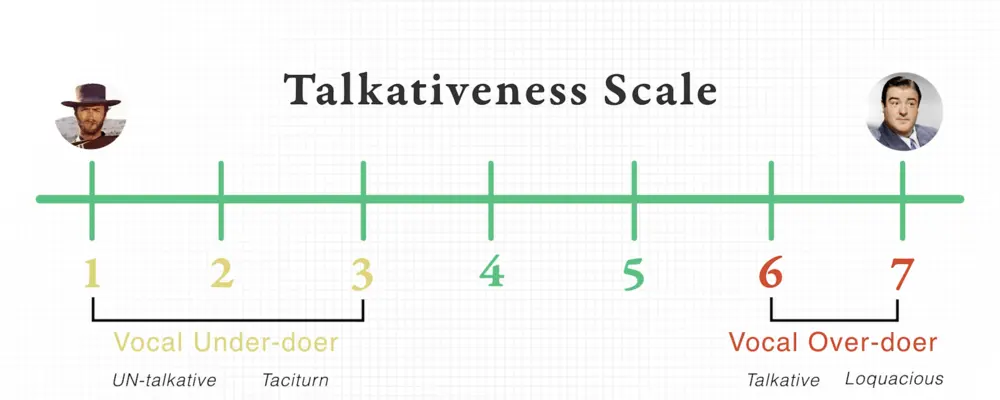
If we use a 7-point scale to rate a person’s talkativeness, vocal underdoers are usually 1’s and 2’s, whereas overdoers are 6’s and 7’s. If we use another 7-point scale to rate a person’s loudness, underdoers again tend to land lower on that scale (that is, they are more soft-spoken) as compared with overdoers.
Typically, overdoers rate themselves accurately on the talkativeness and loudness scales, but underdoers are sometimes less self-aware, describing themselves as more talkative or louder than what their family or friends report.
In addition, even though overdoers are using the vocal fold muscles more vigorously than underdoers, it is paradoxically the vocal underdoers who much more often complain of general voice fatigue.
To be sure, overdoers are the ones who may develop mucosal swelling and thus will report more mucosal “fatigue” symptoms (see swelling checks)—for example, a slight huskiness in the voice that leads them to say, “My voice is tired.” But they don’t typically describe the muscle-based fatigue symptoms that bring underdoers in for consultation: a choking sensation, anterior neck awareness or heaviness, a sense of effort, and so forth.
One reason that vocal underdoers experience more fatigue of the larynx and neck muscles may be that their muscles, being under-conditioned, are more easily fatigued.
It is as though the professional ballet dancer whose back gets a vigorous daily workout rarely feels back strain, whereas the sedentary attorney who sits at a desk all day needs the chiropractor and massage. In addition, for some vocal underdoers, another cause of fatigue may be their tendency to produce voice with simultaneous over-contraction of antagonistic muscles—driving with the brakes on, as it were.
Because the problem of vocal underuse is not as well recognized by some voice clinicians as compared with the problem of vocal overuse, vocal underdoers can suffer through their voice problems much longer without getting a proper diagnosis and treatment.
Below are the stories of four different vocal underdoers, each with his or her own reasons for underusing the voice. Each person came to harm while he or she went undiagnosed.
Vocal underdoer #1: Underuse by nature, abetted by medical advice
Near the beginning of my career, I saw an older, recently retired man who had lived for many years with what he experienced as a weak and inadequate voice. He explained that, early in his career, he had taught chemistry at the college level. He had begun to notice that his voice mechanism and throat in general seemed tired and almost achy at the end of the four to six single-hour lectures he gave each week. He said he seemed to become hoarse and run out of voice (with rapid recovery after brief voice rest) and that he eventually saw an ENT doctor about this.
Since this man’s problem was clearly experienced in the context of sustained projected voice use, and since recovery was associated with rest, he was advised to conserve voice whenever possible, in order to be ready for the next lecture. But the problem only became worse. He saw a second ENT doctor and received similar advice, so he redoubled his efforts to “protect” his voice. The problem continued, and so a third doctor told him it was clear that since the main problem occurred during lectures, he needed to give up teaching. He did this—regretfully, he told me—and spent his remaining working life as a research chemist.
His wife explained that this voice problem had interfered with much more than his work. “For the past 30 years, I don’t think we’ve ever made it through more than 20 minutes of a loud social event,” she said. “For example, after that span of time at a party, he will come over to me with a look of panic and say that his voice just can’t handle the situation, and we end up leaving early. Another example is that we can never stay and visit in the narthex after church; he has to flee situations like that.”
When I asked him to rate his innate degree of talkativeness/sociability on a 7-point scale, he and his wife together chose “2,” denoting a person who is—by nature—quiet and introverted. Still, by my assessment, his speaking voice sounded normal, and his range capability was as expected for his age. During “swelling checks” elicitation, there was no suggestion of mucosal abnormality.
When I modeled a loud voice—“Hey!”—in order to elicit the same production from this man, he initially demurred. “My voice won’t do that,” he said. I reassured, coaxed, and finally insisted that he try. He appeared anxious and even glanced towards his wife for help. Finally, he made what registered to me as guarded and half-hearted attempts. It was as if he could—or would—only turn up the volume to 2x, in response to my demonstration of 5x. Laryngeal examination was normal, other than mild bowing.
It appeared to me that there was nothing fundamentally wrong with the voice, and that this patient suffered from an exaggerated sense of vocal “vincibility” or vulnerability—almost like a mild phobia. It seemed that, based upon his own vocal discomforts, and abetted by the well-intentioned but misguided suggestions of his doctors, this man had come to believe deeply that his voice was weak and fragile and that he had to treat it with extraordinary gentleness. But all along, this man’s real problem (as proven below) was his wrong view of his voice and consequent minimal voice use.
This man was prescribed an initial “marathon session” of therapy with a voice-savvy speech pathologist. I suggested as much as two hours for the first session, during which he would be asked to project his voice nearly continuously, with appropriate coaching and modeling. He would be taught during this time to produce loud voice correctly, too. I advised him that I thought only a few additional sessions would complete the project.
This idea visibly frightened him. He wanted to know if I would be nearby during this therapy session, in case there was a problem. I assured him that, if necessary, I’d be glad to examine his larynx every 20 minutes with video equipment that would allow him to see for himself. (It never came to that.)
Within a few sessions, this man was almost miraculously let out of his 30-year vocal self-confinement. His wife told me that he had experienced an actual personality change and had become talkative even with strangers!
Vocal underdoer #2: Jumping to a wrong conclusion
I saw a young baritone who was pursuing a voice performance major at a nearby university. Early in the consultation, he told me with an undercurrent of desperation that his voice had been ruined a few months earlier, when he had undergone a tonsillectomy with endotracheal intubation. He said that the surgeon, knowing the patient was a serious singer, suggested a month should elapse before resuming singing, and he, the patient, had decided that if a month was good, two months might be better yet for his instrument, and that he would avoid not only singing, but also talking.
The problem that he explained in the consultation was that, in his words, “I have a different voice than I used to have.” He further stipulated that his new voice had no strength or depth or “body.” He didn’t remember any unusual early postoperative hoarseness, partly because during that time he had written messages instead of speaking. He had used his voice minimally and always gently during the remainder of the two months, and when he resumed using his voice two months after the procedure, he immediately came to believe that the breathing tube must have damaged his vocal folds.
At the time I saw him, he was continuing to rest his voice, but checking it briefly every day for recovery. Now, as he was about to begin the final month of the fall semester and without any apparent progress, he was in panic mode.
On the 7-point scale for innate talkativeness, this man chose “5.” Just as with the man in case 1, I was interested that this young singer’s speaking voice sounded normal—average man-on-the street for his age. He was only slightly tentative when asked to project voice. I did not notice any hypernasality, nor was there any leakage of air when he pretended to blow up a stiff balloon. (Rarely, tonsil surgery can unmask or create a palate deficiency such that it doesn’t fully seal off the nasopharynx during speech.3 The result is a hypernasal resonance quality.) Swelling checks for mucosal injury were normal up into a fairly clear and high falsetto, and laryngeal examination, including stroboscopy, was also normal.
My diagnosis was that this voice was actually normal: there had been no injury to his vocal folds nor to his resonators at the time of the tonsillectomy. My alternate diagnosis was that this young man had developed a firm belief in injury, when in fact the problem was vocal deconditioning below the threshold needed for good singing. He was initially dubious. Therefore, with an eye to his skepticism, I asked him to adopt a regimen, with a timer as the arbiter.
He was to begin having voice practice sessions twice a day, on day one for five minutes per session, and then each day adding another five minutes to each practice session, so that by the end of a week he would be singing 30 minutes twice a day. And so forth. Within a few weeks, the problem vanished.
Vocal underdoer #3: Panic and extended voice rest from red herring findings
I saw a late-career, classically trained soprano who was quietly distraught. She announced that she had nodules and that her career was on hold waiting for them to resolve. She mentioned that singing was her livelihood, her sole means of support; she was now in financial distress because of the problem.
It all began three months earlier, when she had seen an otolaryngologist due to some allergy symptoms of sneezing, runny nose, and itchy eyes. In the course of a complete ear, nose, and throat examination, he had told her that he saw vocal nodules. She had panicked, gone into strict voice rest, and begun canceling performances around the country so that she could resolve her nodules. She was seeing me because, three months later, her voice was not improving at all, and in fact seemed to have gotten worse as a result of her voice rest.
I asked her to place herself on the 7-point innate talkativeness scale. Without a second’s thought and with a smile and a shrug, she chose “7.” (This is often the talkativeness profile of successful performers.) I then asked if the weeks or months leading up to the allergy symptom consultation had been particularly demanding vocally. She said no. I asked her if the reason for the visit three months earlier included any worries about her voice. She said that her voice had seemed fine—it was primarily her nose and eye symptoms that had caused her to make that appointment.
In the course of my evaluation of her voice, I noted that her swelling checks were very impaired, confirming mucosal injury. She began to struggle with onset delays as low as A4, a full octave below her necessary public singing range. Laryngeal examination confirmed small, pointed spicule-like vocal nodules.
Even though the soprano’s voice had been working at its normal baseline when her vocal nodules were first noticed, she had become convinced that she needed to rest her voice until those nodules went away. I was convinced that this well-intentioned voice rest had caused her voice to deteriorate. I believed that she had been singing with nodules at a professional level for years, and that rest had actually made her less able to coexist with or conceal these “baseline” nodules.
After all, I reasoned, she had been a “7” all her life. More importantly, there had been no sense of vocal indisposition or increased voice use prior to the time of her nodule diagnosis. I explained that she was like a premier ice skater with a few ounces of lead in her skates. She had indeed been laboring with an impediment, but quite successfully, and she could likely return to doing the same going forward, as these were probably stubborn, chronic nodules that might not resolve without the help of surgery. I predicted that, as long as she stayed in very good shape by vocalizing regularly, she could likely again “skate circles around others.” If I was wrong, or if she became unwilling to adapt to the “lead in the skates,” I explained, there would be an excellent surgical option to restore her voice.
As with case 2, I advised her to gradually build up her voice. She departed mostly unconvinced, but promised to “give it a try.” After the first week, she reported by telephone, “Well, it is definitely better, but I can’t return to performing with this voice.” We established together that “50%” described her voice at our first consultation, and now, she felt she had progressed to 75% of her baseline voice. After another week, however, it was up to 85%, and within three or four weeks, she stopped canceling performances and returned to her work.
Her nodule problem remained, causing detectable impairment of the swelling checks for the several additional years that I followed her, but her excellent technique and careful choice of repertoire allowed her to continue performing successfully for many more years.
Vocal underdoer #4: Inaccurate self-perception and loudness set-point
A thirty-something woman visited me because of irritated comments she was getting from co-workers and others. They were complaining, she said, that they could never hear her. The patient seemed perplexed and troubled by their frustration. During the entire encounter, she spoke like this, or less. Halfway through our lengthy conversation I remember feeling a little irritated at the effort needed to understand her, just as one might feel if forced to read a book chapter in extra-fine print. To the present, this person remains the most soft-spoken person I have ever met whose voice mechanism was normal.
During my evaluation, I did not notice any roughness or hoarseness. There was no air-wasting quality. When I elicited (by first demonstrating myself) loud voice, she repeated her “baseline” soft-spoken voice. That is, she responded still with this voice. Or perhaps at most this voice. I continued to request, and coax, and finally to insist that she produce this voice. But without continual cues and encouragement from me to keep this up, she reverted to this voice. And when I asked her what she thought of the normal-loudness voice she had produced briefly at my insistence, she said in all sincerity, “I could never talk like that—that’s yelling.”
This quiet woman manifested an inappropriate set-point for vocal loudness. Although others would be incredulous to hear her say it, she truly believed that her vocal loudness was normal, rather than recognizing, as everyone else did, that she was remarkably soft-spoken.
Here, I pointed out the concept of a “loudness set-point” to explain why people speak at differing loudness levels, each of which seems normal to them. I explained that just as someone else might go through life “yelling” as perceived by ears of everyone but themselves, she was going through life practically whispering in everyone’s view but her own.
We established that she would explain to family and friends the 7-point loudness scale and that she would give them permission to do “sound checks” with her. That is, they were permitted to hold up one finger, or three, or whatever the case might be, in order to indicate how loud her voice seemed to them in that moment, in comparison with the rest of the human race. In addition, I suggested that she occasionally solicit a “sound check.” For example, she might decide in advance to adopt a “5” loudness level at a dinner out with friends, and then mid-meal, request a “sound check” to see if her perception matched theirs.
Using these means, her assignment was to figuratively graft other people’s auditory perceptions into her own, in order to first understand and accurately perceive—and then possibly to realign—her own innate “set-point.” She would come to understand and measure for herself when she was talking like this, and when like this. She would no longer feel perplexed at how others experienced her voice.
Understanding vocal underdoers
What is the common thread in all these stories? In each case, the person’s voice problem did not arise primarily from a disorder or injury of the voice-making apparatus (weak, deconditioned muscles and nodules notwithstanding), but instead from a personality or a conviction, supported in some cases by misguided external advice, which caused that person to inappropriately rest or restrain the voice.
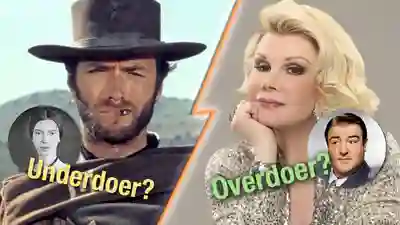
It is important to recognize that, like the soprano in case 3, an individual can have a lifelong classic vocal overdoer profile, and yet abruptly, due to some new life circumstance or belief, become instead a vocal underdoer. Also, as illustrated by her story, one can have an actual vocal disorder (nodules, in her case) that is a red herring alongside the main issue: quailing from voice use and disbelieving in the larynx’s capabilities. Others are innately vocal underdoers, like the man in case 1 and the young woman in case 4.
These vocal underdoer cases illustrate that voice rest is not always the answer, that rest can actually become a hindrance to having or re-gaining a normal voice. Just as vocal overdoers need to learn the skills of voice care and conservation in order to avoid injury to mucosa, and also to perform “swelling checks” regularly, vocal underdoers often need to get in touch with the “big voice” that they might never use across an entire lifetime due to personality, and to understand that the voice, like any other body part, can benefit from and “enjoy” a degree of vigorous use. Vocal overdoers need to learn vocal underdoer skills, and vocal underdoers need to learn vocal overdoer skills.
Share this article
Vocal Underdoer – Overdoer Continuum | Understanding Proper Voice Use
What is the Vocal Under-Doer and Vocal Over-Doer Continuum? Why is it an important concept for everyone interested in the voice (voice teachers, speech pathologists, voice doctors, singers, actors, etc.)? Because it provides critical insights into understanding and responding to potential voice disorders or risk of developing voice disorders.
Dr. Bastian’s 7-point “talkativeness scale” allows individuals to rate and become self-aware of their level of talkativeness and sociability.
“Vocal under-doers” may currently have, or eventually develop conditions such as vocal weakness, vocal inconfidence, and vocal fatigue.
On the other hand, “vocal over-doers” are more at risk than the average person of vocal cord injuries such as nodules and polyps. A “curriculum” is suggested by Dr. Bastian for persons on each end of the under-doer / over-doer continuum.

3 Simple Exercises to Strengthen A Weak Voice
A weak voice that can’t be heard in noisy places, or that “fades” in quality and strength across a day can be frustrating!
There is a long list of potential explanations. A common one is weak, atrophied, flaccid vocal cord—and other vocal tract—muscles. When this is the cause for a weak voice determined by medical evaluation, voice building is the first place to start.
In this video, Dr. Bastian provides background information about muscle building in general, and why vocal muscles can weaken in some people.

Here Are 3 Voice Strengthening Strategies for Parkinson’s Disease
Persons with Parkinson’s Disease (PD) often develop weak, even whispery voices. The explanation is not only a weak mechanism (primarily muscles), but also PD’s reduction of the inner vitality that “energizes” voice and speech.
This video outlines a rationale and strategy for voice building designed specifically for PD. The two fundamental ideas are to challenge the muscles of voice and speech, and also to “rev the engine” of the voice. Simple at-home exercises are explained that the affected individual and family/friends can easily master.
Along with expert medical / pharmacological management, a trial of this sort is appropriate before considering anything else (like vocal cord implants).
- Bastian RW. The vocal overdoer syndrome: a useful concept from the voice clinic. Journal of Singing. 2002; 58(5): 411-13. [↩]
- Johns MM. Update on the etiology, diagnosis, and treatment of vocal fold nodules, polyps, and cysts. Curr Opin Otolaryngol Head Neck Surg. 2003; 11(6):456-61. [↩]
- Haapanen ML, Ignatius J, Rihkanen H, Ertama L. Velopharyngeal insufficiency following palatine tonsillectomy. Eur Arch Otorhinolaryngol. 1994; 251(3):186-9. [↩]