Can’t Burp?
You’ve come to the right place.
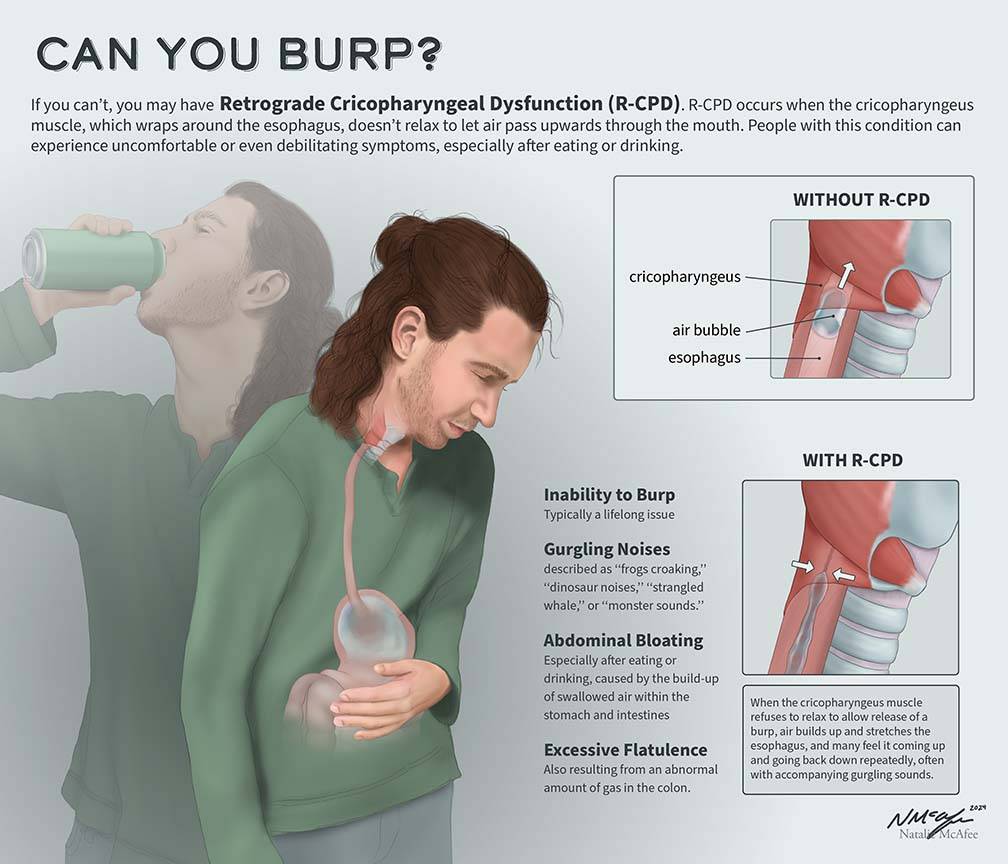
Inability to belch or “burp” (Also known as Retrograde Cricopharyngeus Dysfunction, or R-CPD for short) occurs when the upper esophageal sphincter (UES) loses its ability to relax in order to release the “bubble” of air.
![]()
What is R-CPD (Inability to burp, no-burp)?
People who cannot release air upwards are miserable. They can feel the “bubble” sitting at the mid to low neck with nowhere to go. Or they experience gurgling when air comes up the esophagus only to find that the way of escape is blocked by a non-relaxing sphincter.
It is as though the muscle of the esophagus continually churns and squeezes without success. Common symptoms include the inability to belch, gurgling noises, chest/abdominal pressure and bloating, and flatulence.
![]()
The Top 4 Symptoms of R-CPD
Inability to burp
This is almost always, but not exclusively “lifelong,” often excluding infancy, since many with R-CPD did burp as infants. Most no-burpers can’t remember being conventionally able to burp and can also point to a time when they became aware of this as a “problem” or “difference from others” in childhood or teen years.
Some with R-CPD do burp occasionally but they are micro, random, not harnessable, and they don’t provide relief of the following symptoms.
Socially awkward gurgling noises
These noises can be mostly quiet and “internal,” but more often are loud enough to be embarrassing. Mouth opening makes them louder. Almost everyone says they are easily heard several feet away; not infrequently “all the way to the door.”
They engender social anxiety in most persons with R-CPD, causing some to avoid eating or drinking for hours before social occasions and even during them. Carbonation makes them much worse and is to be avoided at all costs. Some more colorful patient descriptions:
- Symphony of gurgles
- Croaking frogs
- Creaking floorboards
- Dinosaur sounds
- Strangled whale
- The Exorcist
Audio examples of gurgling
Bloating & Pressure
Most common location is high central abdomen. Distention is common, especially later in the day. Using pregnancy as an analogy even in men, the usual degree of distention is described as “3 or 4 months.” “Six months” is not rare, and one slender young man was “full term.”
Almost as often as abdominal distress, patients describe chest pressure, and for some that is the worst symptom. Some have pressure in the low neck. While “pressure” is the frequent descriptor, some experience occasional sharp pain in abdomen, back, or between shoulder blades. Some have to lie down after eating to find some relief.

Flatulence
Routinely, this is described as “major,” or even “ridiculous.” Flatulence increases as the day progresses, and many experience it into the night. When around others, some scan their surroundings at all times for a place they can go briefly to pass gas. Understandably, the social ramifications of this problem can also be major.
![]()
Less Common Symptoms of R-CPD
Nausea
especially after eating larger than normal amounts or drinking carbonated beverages.
Throat Nausea?(YouTube short)
Hypersalivation
when symptoms of bloating are major.Painful Hiccups
again, more commonly after eating.
Anxiety & Social Inhibition
This can be MAJOR due to gurgling, flatulence, and discomfort.
Shortness of Breath
A person can be so full of air that athletics—or even the ability to climb stairs—are impaired.
Constipation
(Still under evaluation): Flatulence can’t always be responded to, and the result is descending colon appears to dilate, making stretched muscles in its wall less effective in moving colon contents along.
Inability to Vomit
A few simply cannot vomit; more often it is possible but only after strenuous retching. Vomiting (spontaneous or self-induced) always begins with a very loud noise and major release of air in a phenomenon we call “air vomiting.” Emetophobia can be major.
![]()
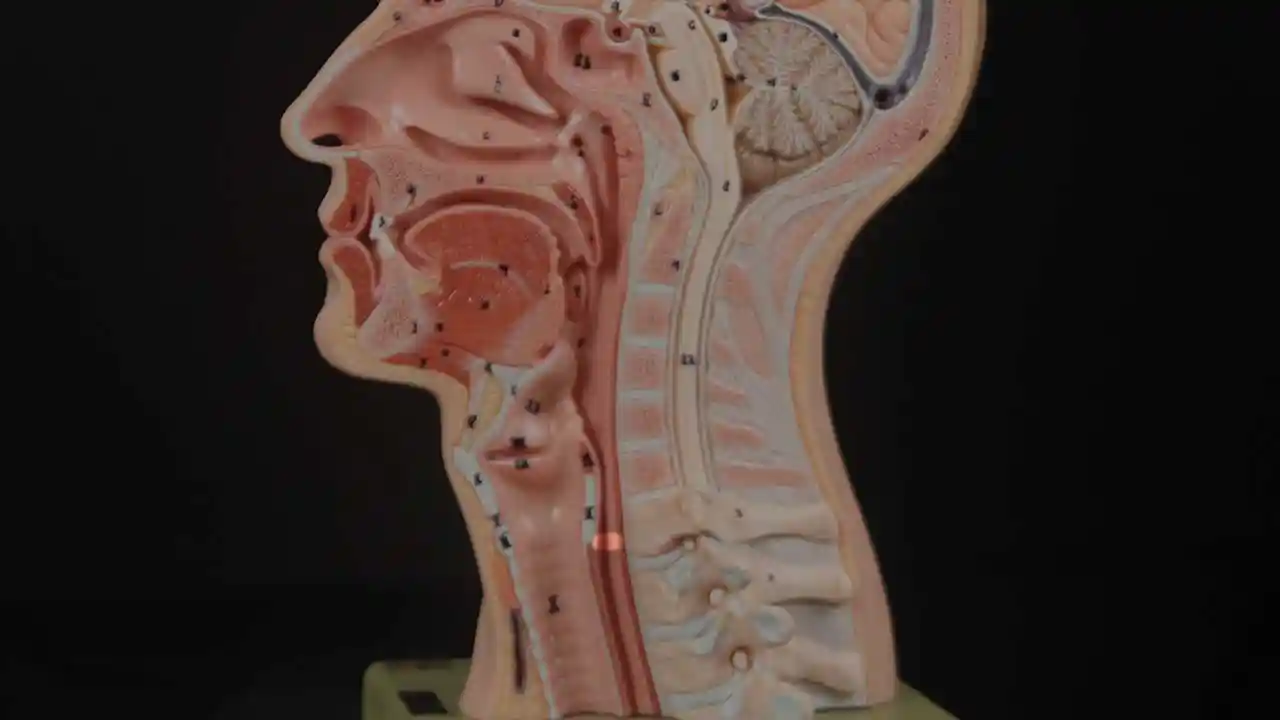
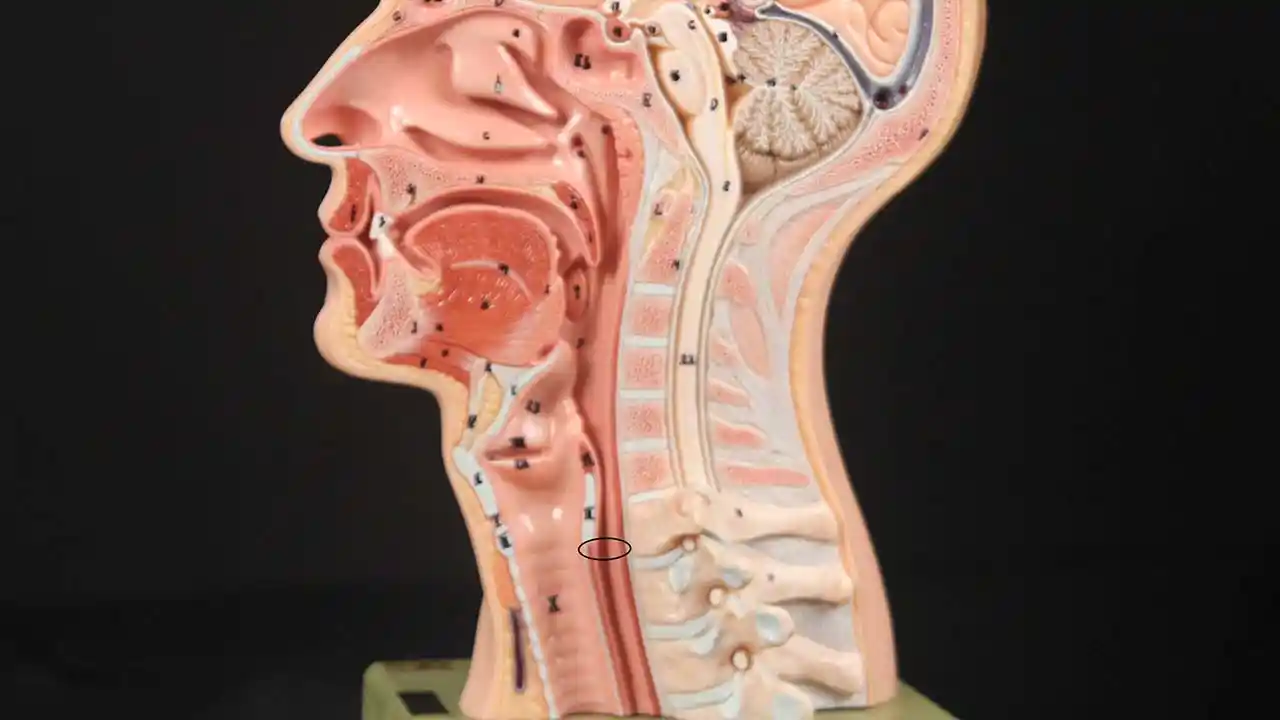
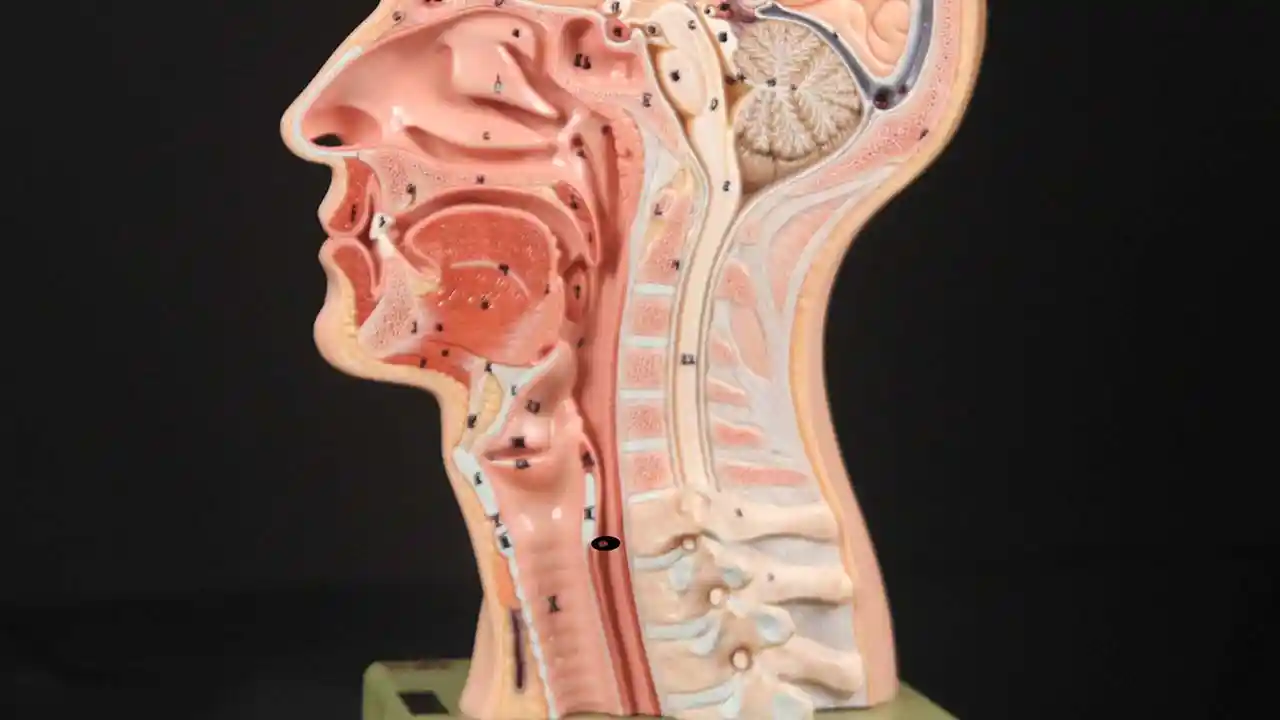
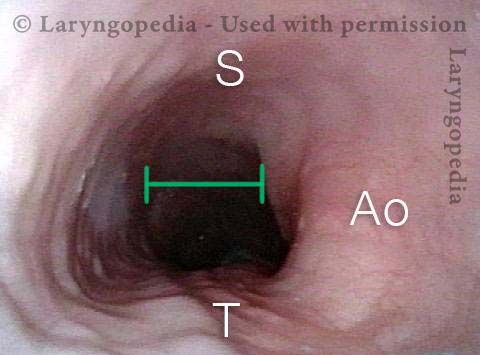
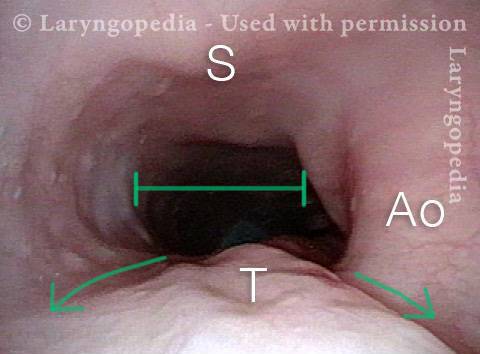
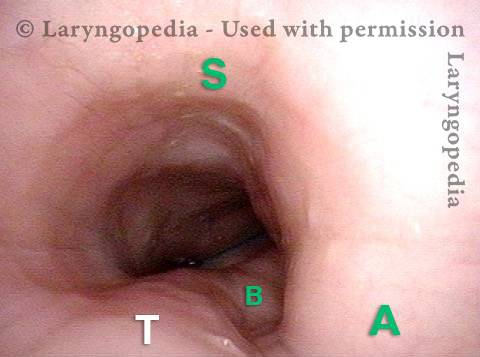
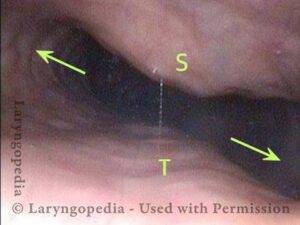
What Causes R-CPD?
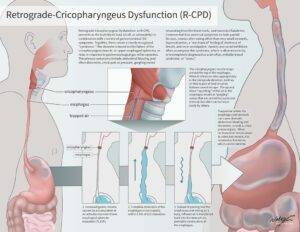
Inability to burp or belch occurs when the upper esophageal sphincter (cricopharyngeus muscle) cannot relax in order to release the “bubble” of air. The sphincter is a muscular valve that encircles the upper end of the esophagus just below the lower end of the throat passage. If looking from the front at a person’s neck, it is just below the “Adam’s / Eve’s apple,” directly behind the cricoid cartilage.
If you care to see this on a model, look at the photos below. That sphincter muscle relaxes for about a second every time we swallow saliva, food, or drink. All of the rest of the time it is contracted. Whenever a person belches, the same sphincter needs to let go for a split second in order for the excess air to escape upwards.
In other words, just as it is necessary that the sphincter “let go” to admit food and drink downwards in the normal act swallowing, it is also necessary that the sphincter be able to “let go” to release air upwards for belching.
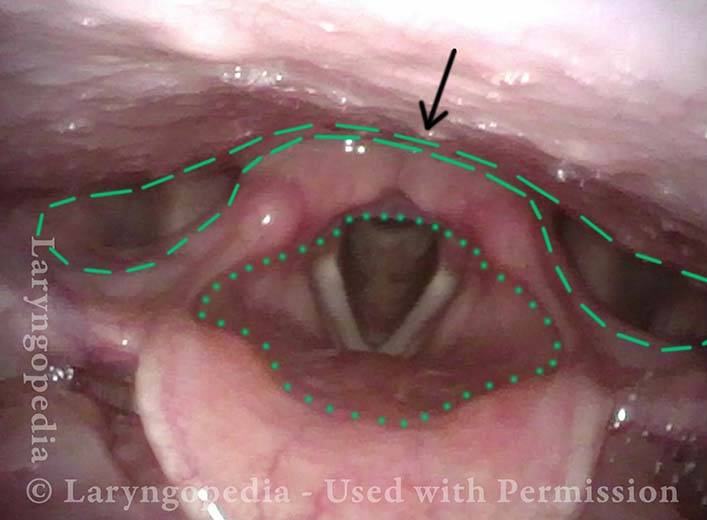
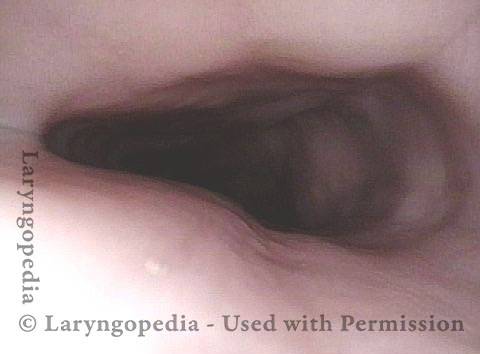
Cricopharyngeus Muscle (1 of 3)
Cricopharyngeus Muscle (1 of 3)
Open Cricopharyngeus Muscle (2 of 3)
Open Cricopharyngeus Muscle (2 of 3)
Closed (3 of 3)
Closed (3 of 3)
![]()
Treatment for R-CPD
Botox Injection at Bastian Voice Institute
For people who experience this problem to the point of discomfort and reduced quality of life, here is one approach:
First, a videofluoroscopic swallow study, perhaps with effervescent granules. This establishes that the sphincter works normally in a forward (antegrade) swallowing direction, but not in a reverse (retrograde) burping or regurgitating fashion. Along with the symptoms described above, this establishes the diagnosis of retrograde-only cricopharyngeus dysfunction (non-relaxation).
Second, a treatment trial involving placement of Botox into the malfunctioning sphincter muscle. The desired effect of Botox in muscle is to weaken it for at least several months. The person thus has many weeks to verify that the problem is solved or at least minimized. (See video, What Tests are Necessary for R-CPD?)
The Botox injection could potentially be done in an office setting, but we recommend the first time (at least) placing it during a very brief general anesthetic in an outpatient operating room. That’s because the first time, it is important to answer the question definitively, that is, that the sphincter’s inability to relax when presented with a bubble of air from below, is the problem.
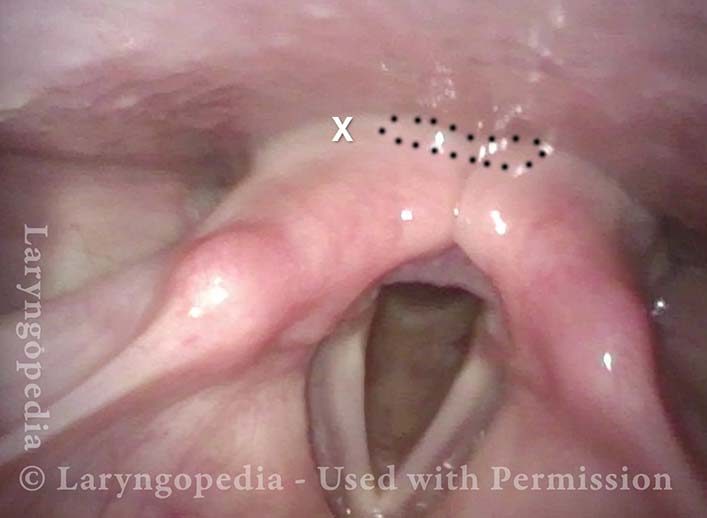
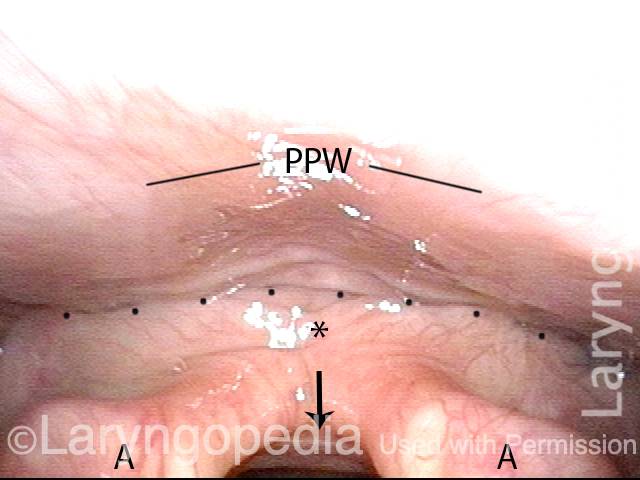
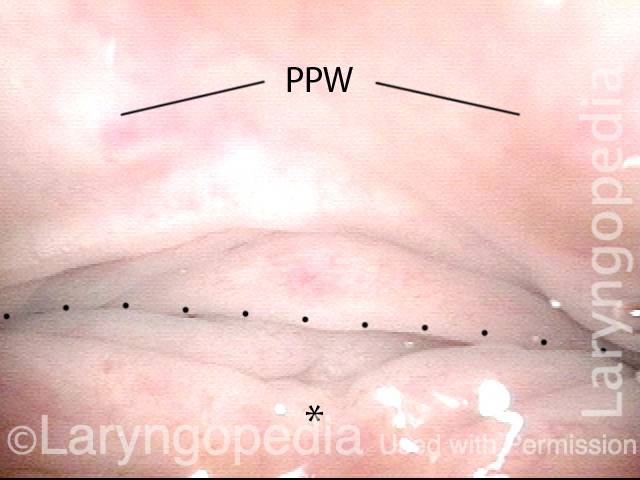
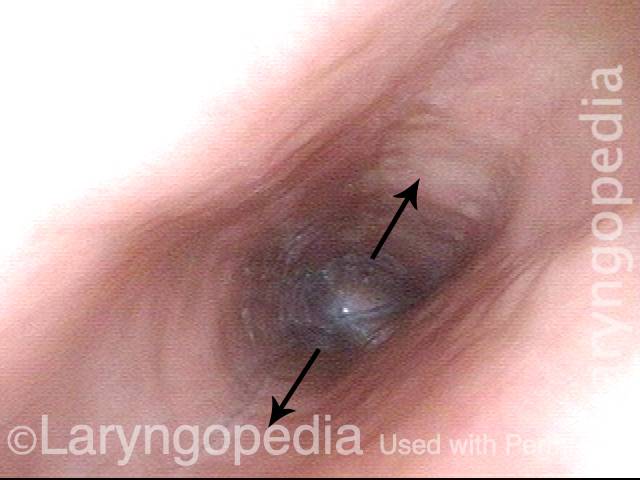
Lifting the CPM for a R-CPD Injection
These are intra-operative photos of one of nearly 2,000 persons treated for R-CPD as of December 2024. This sequence shows several things:
- The dilated, “always open” esophagus distal (below) the muscle
- How to identify the cricopharyngeus muscle
- One way of injecting the muscle.
Above the CPM (1 of 5)
Above the CPM (1 of 5)
Ridge of the CPM (2 of 5)
Ridge of the CPM (2 of 5)
Exposed CPM ( 3 of 5)
Exposed CPM ( 3 of 5)
CPM Palpated ( 4 of 5)
CPM Palpated ( 4 of 5)
Botox injection ( 5 of 5)
Botox injection ( 5 of 5)
How do I Know How Many Units of Botox my Doctor Should Inject for My R-CPD?
Unsatisfyingly, the answer is “that depends,” for two main reasons. The first is placement. If the doctor’s is very accurate, the amount injected can be less than if inaccurate. (And any good ENT doctor should be able to aim accurately without difficulty.)
The second reason is the innate difference of individual sensitivity to Botox. It is known from other sites that one person may need a bigger dose than another to get the same result. And it doesn’t correlate with age, sex, weight, height, etc. and so there is no predicting…
In the larynx, where we inject botox for a rare neurological voice disorder, the dose varies by a factor of at least 20. Most lie in a middle range, of course, but there are “outliers” on both the “hypersensitive” and “insensitive” ends of the scale.
The muscle we are injecting is small, and that is why I initially thought that 50 units—the dose I used for my first 200 patients—was generous. That dose worked well for virtually everyone I injected. In fact, it was likely a higher dose than needed for some. But it was not enough for the very occasional patient. And so, to “capture” the rare patient who needs higher dose, I increased to 75 units for approximately the next 700 patients.
Again, a really good result followed for “almost” all 700. But for the next 150 or so, I used 100U for two reasons. One is that the patient has purchased the entire vial of 100, so I figure to just give the full amount. The second is that so many travel from such a distance (even internationally) that we want to make certain even if they are a bit insensitive to Botox, they still get a good result…
So many patients would do fine with 50 or even 75, but the above reasons explain my current dose of 100. To repeat, keep in mind it is not only dose but – critically – accurate placement that may determine the effectiveness of any given injection. Thankfully targeting is only occasionally difficult, so most people will do well with 50, 75 or 100. If we could know in advance each individual’s dose requirement, I am sure some would do well even with 25 units!
Is there any downside to using a higher dose than (in retrospect) would have been necessary? The only downside of higher dose would be a bit more of the initial “slow swallow” which everyone gets through…
What to Expect Post Botox Procedure?
Review Dr. Bastian’s published Journal entry for a complete explanation, but in a nutshell:
- There will be no relief of R-CPD symptoms for 1—5 days.
- Only when micro-burps begin do patients start to notice the beginning of symptom relief. So do not try carbonation for lunch on the day of the injection!
- Initial Botox side effects can be “weird” for a few days to weeks.
- If you can manipulate your gurgles prior to Botox treatment, to make them softer or louder, use that technique to see if you can hurry burps along or make them bigger.
For a few months at least, patients should experience dramatic relief of their symptoms. And, early experience suggests that it may be that this single Botox injection allows the system to “reset” and the person may never lose his or her ability to belch. Of course, if the problem returns, the individual could elect to pursue additional Botox treatments, or in a truly severe case, might even elect to undergo endoscopic laser cricopharyngeus myotomy.
![]()
Frequently Asked Questions
How long does it take to burp after the procedure?
As little as 24 hours (occasionally less), often on the second or third day. But we see some beginning to burp only after several days.
How common are laryngospasms after the procedure?
Not very. They seem more often in people who have commenced the slow swallow phenomenon and then take big bites, chew only a couple of times, and then swallow. Our advice is to take small to medium bites, chew well, and include liquid in your mouth with the food, or immediately chase the food with a sip of liquid. See this video for more information.
I think my 8 year old has R-CPD. Can she get the botox injection?
Of course, everything depends upon confirmation of diagnosis, by a personal physician, age eight is a very good time to identify and resolve this.
In fact, the hope is that more people are diagnosed early so that they don’t have to suffer through high school, into adulthood, etc. An 8-year-old has a very high likelihood of a “once and done” result (expectation is 80% chance…)
I’ve had two injections without success. Should I have a Cricopharyngeal Myotomy?
In our patients, we consider myotomy after a minimum of 2 extremely effective Botox injections (very good burping, relief of symptoms followed by return of the R-CPD symptoms). Sometimes a change of dose or targeting is the answer. “It isn’t what is in the syringe, but what makes it into the muscle…” I’d even prefer 3 “perfect” injections in patients younger than 30 years old.
Is it possible to have Barrett’s esophagus and R-CPD at the same time?
It is theoretically possible to have any other GI condition alongside R-CPD. We have found that most GI symptoms end up being related to R-CPD, and maybe first among the associations might be acid reflux.
This is common in our R-CPD population, likely due to the constant upward pressure on the lower esophageal sphincter, causing it to weaken over time. And since chronic acid reflux may be a potentiator of Barrett’s esophagus findings, it could be that treating R-CPD and reducing the acid reflux that results might over time heal the Barrett’s findings…We have not proven this, however.
Is acid reflux (GERD) a symptom of R-CPD?
GERD is very common, because of years of high pressure endured by the lower esophageal sphincter. Often people with R-CPD get told the primary diagnosis is acid reflux, when acid reflux is only one of the symptoms of R-CPD.
Keep in mind that symptoms of R-CPD are “all” GI, rather than at the cricopharyngeus muscle itself. So if gurgling, bloating, hiccups, are present even with ability to burp, consider the idea of not inability, but ‘insufficiency’ of burping where air out (via burping) is less than air in.
What to expect with pregnancy and R-CPD?
It is impossible to say how it will go for any individual. Of our nearly 1900 patients (August 2024), we have a number who had gone through pregnancy. A few could burp somewhat during pregnancy, likely due to the increased pressure upwards, but then lost the ability postpartum. More often, it is just more misery during that time, but then again, everyone got through it…
Can you have partial R-CPD?
Yes, there are people who can do microburps but usually not relieving. Therefore they don’t have complete inability to burp but burping insufficiency.
If they have sufficient symptoms of R-CPD, they have it, even if they can burp somewhat. If you have a significant number of these symptoms, that makes the working diagnosis of R-CPD.
![]()
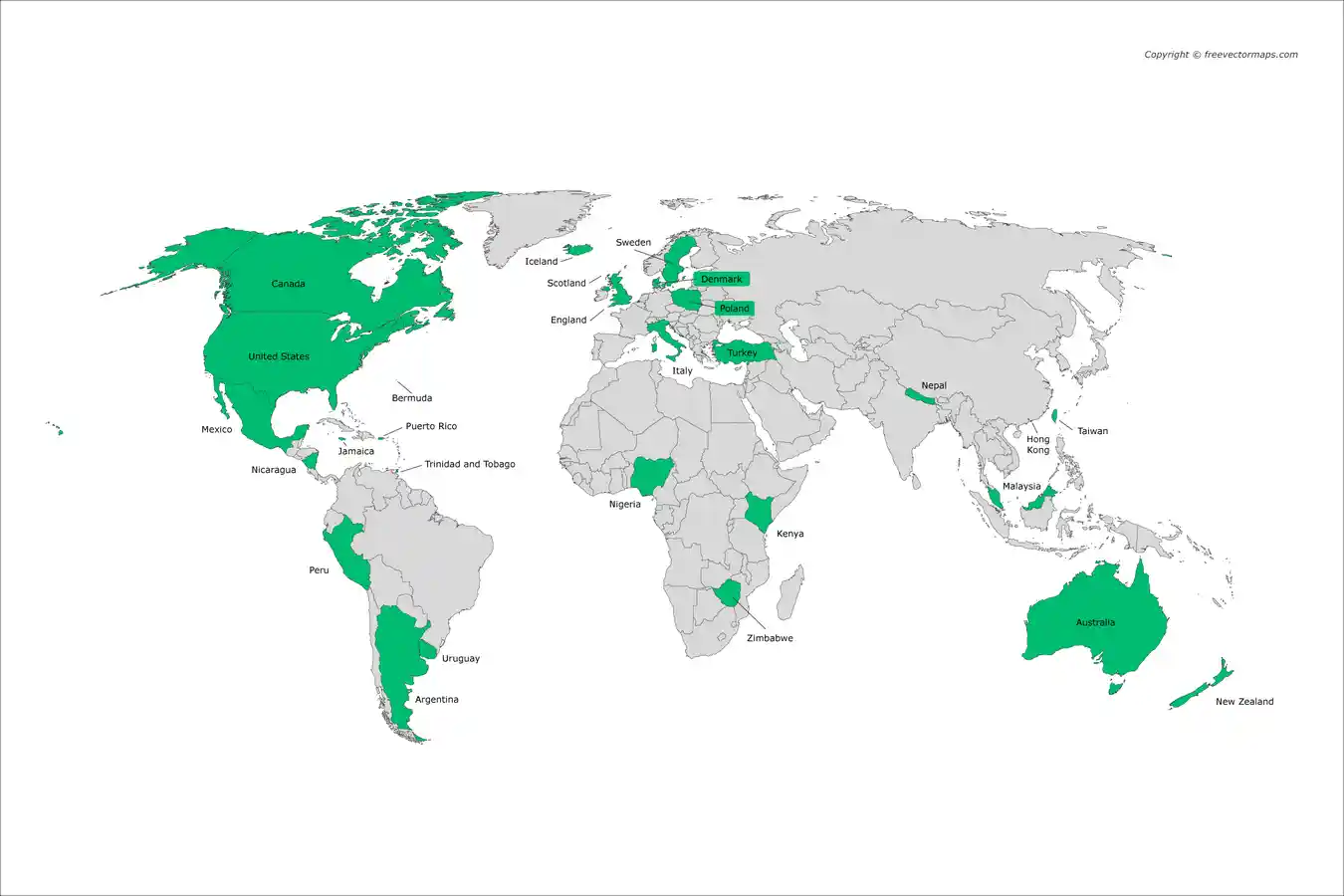
Where do Our R-CPD Patients Come From?
NO-BURPERS turned burpers!
![]()
Photo Essays from our R-CPD Patients
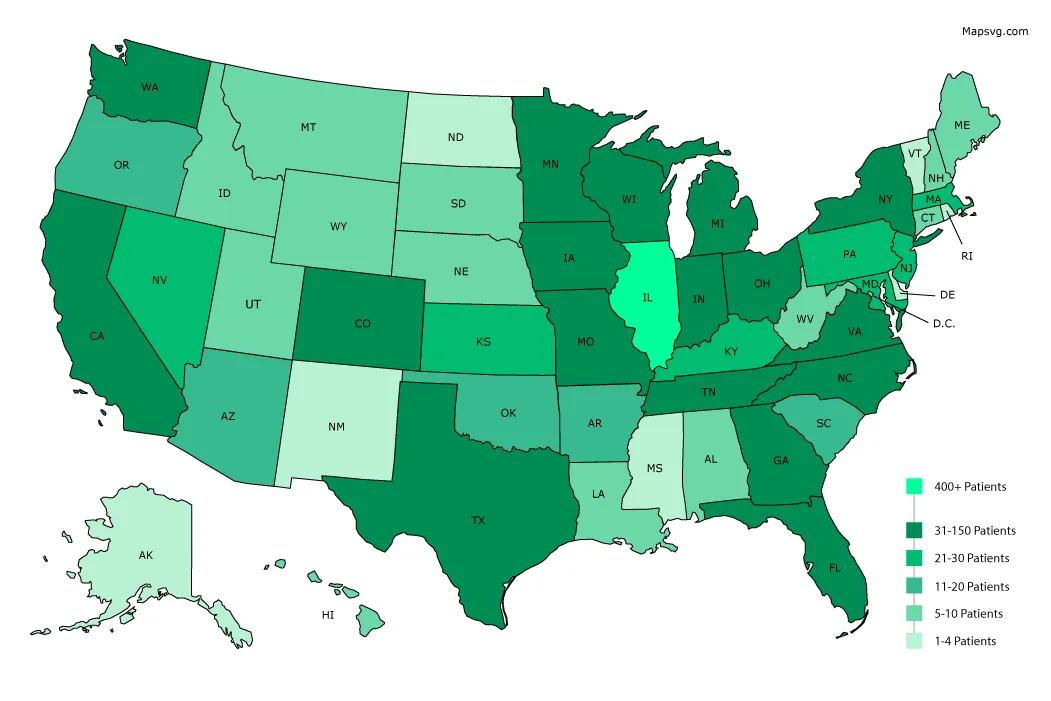
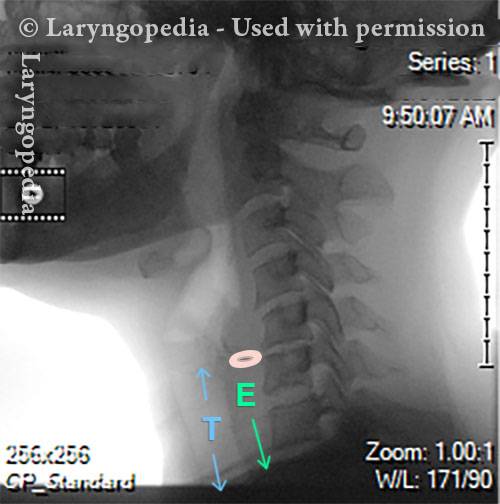
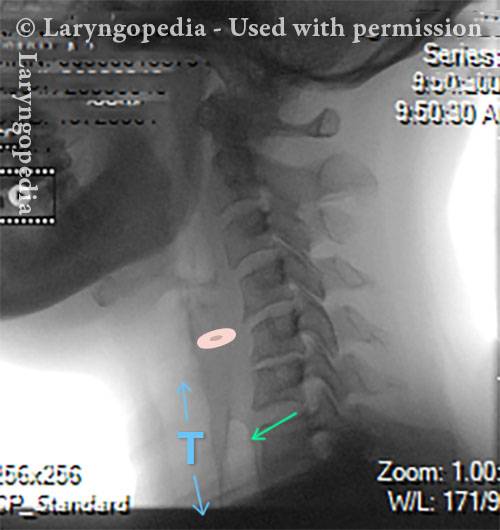
R-CPD, Aerophagia and Burping
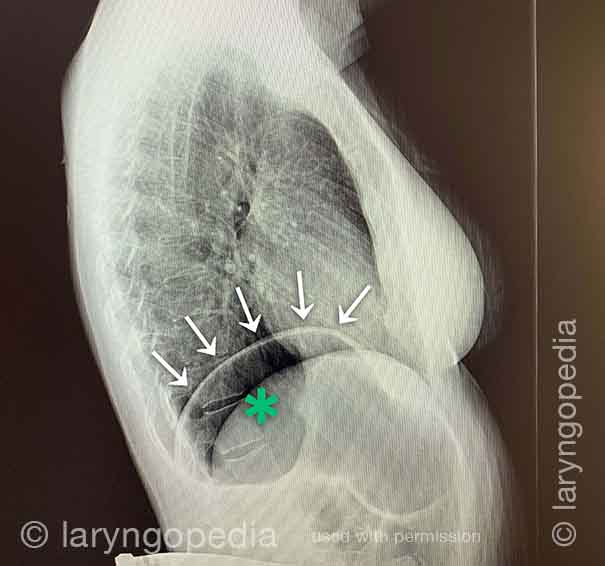
This lateral x-ray of the neck is part of a swallow study, and illustrates how air can accumulate and need to be burped up. The focus of this post is the esophagus, or “foodway,” that connects the lower part of the throat to the stomach. The esophagus is a muscular tube that remains mostly collapsed—closed—except when food, liquid, or saliva traverses it.
X-Ray of Larynx (1 of 6)
X-Ray of Larynx (1 of 6)
Barium swallow (2 of 6)
Barium swallow (2 of 6)
Collapsed esophagus (3 of 6)
Collapsed esophagus (3 of 6)
Air is swallowed (4 of 6)
Air is swallowed (4 of 6)
UES refuses to open for a burp (5 of 6)
UES refuses to open for a burp (5 of 6)
Abdominal Distention from R-CPD (6 of 6)
Abdominal Distention from R-CPD (6 of 6)
Abdominal Distention of R-CPD
Gastric Air Bubble (1 of 3)
Gastric Air Bubble (1 of 3)
Bloated Abdomen (2 of 3)
Bloated Abdomen (2 of 3)
Non-bloated Abdomen (3 of 3)
Non-bloated Abdomen (3 of 3)
Abdominal Distention Caused by R-CPD
Bloating and abdominal distention before botox injection for inability to burp (1 of 2)
Bloating and abdominal distention before botox injection for inability to burp (1 of 2)
Resolved, one month after botox, with burping restored (2 of 2)
Resolved, one month after botox, with burping restored (2 of 2)
Can’t Burp: Progression of Bloating and Abdominal Distention – a Daily Cycle for Many with R-CPD
This young woman has classic R-CPD symptoms—the can’t burp syndrome. Early in the day, her symptoms are least, and abdomen at “baseline” because she has “deflated” via flatulence through the night.
In this series you see the difference in her abdominal distention between early and late in the day. The x-ray images show the remarkable amount of air retained that explains her bloating and distention. Her progression is quite typical; some with R-CPD distend even more than shown here especially after eating a large meal or consuming anything carbonated.
Side view of a bloated abdomen (1 of 6)
Side view of a bloated abdomen (1 of 6)
Front view (2 of 6)
Front view (2 of 6)
Greater Distention (3 of 6)
Greater Distention (3 of 6)
Front view of bloating stomach (4 of 6)
Front view of bloating stomach (4 of 6)
X-ray of trapped air (5 of 6)
X-ray of trapped air (5 of 6)
Side view (6 of 6)
Side view (6 of 6)
The Daily Inflation-Deflation Cycle for R-CPD
Deflated Abdomen (1 of 4)
Deflated Abdomen (1 of 4)
Bloated lateral view (2 of 4)
Bloated lateral view (2 of 4)
Deflated abdomen (3 of 4)
Deflated abdomen (3 of 4)
R-CPD distention (4 of 4)
R-CPD distention (4 of 4)
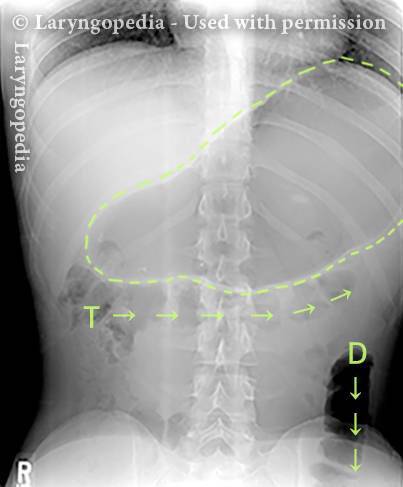
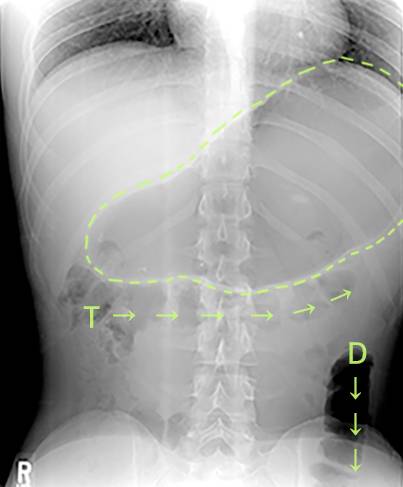
A Rare “abdominal crisis” Due to R-CPD (inability to burp)
This young man had an abdominal crisis related to R-CPD. He has had lifelong symptoms of classic R-CPD: inability to burp, gurgling, bloating, and flatulence. During a time of particular discomfort, he unfortunately took a “remedy” that was carbonated.
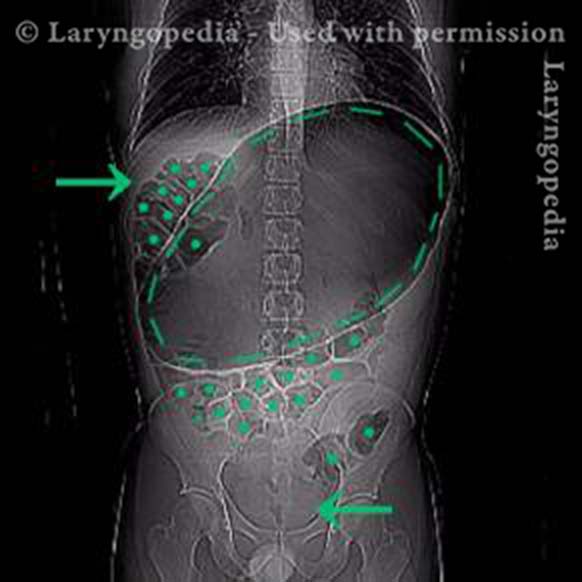
Here you see a massive stomach air bubble. A lot of his intestines are air-filled and pressed up and to his right (left of photo, at arrow). The internal pressure within his abdomen also shut off his ability to pass gas.
X-Ray of Abdominal Bloating (1 of 2)
X-Ray of Abdominal Bloating (1 of 2)
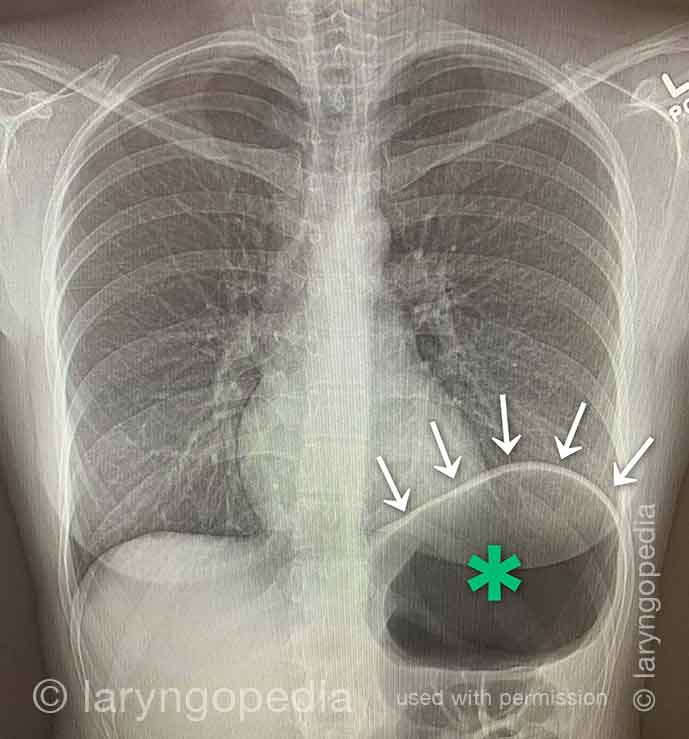
Shortness of Breath Caused by No-Burp
Persons who can’t burp and have the full-blown R-CPD syndrome often say that when the bloating and distention are particularly bad—and especially when they have a sense of chest pressure, they also have a feeling of shortness of breath.
They’ll say, for example, “I’m a [singer, or runner, or cyclist or _____], but my ability is so diminished by R-CPD. If I’m competing or performing I can’t eat or drink for 6 hours beforehand.” Some even say that they can’t complete a yawn when symptoms are particularly bad. The x-rays below explain how inability to burp can cause shortness of breath.
X-ray of trapped air (1 of 2)
X-ray of trapped air (1 of 2)
Side view (2 of 2)
Side view (2 of 2)
Esophageal Findings
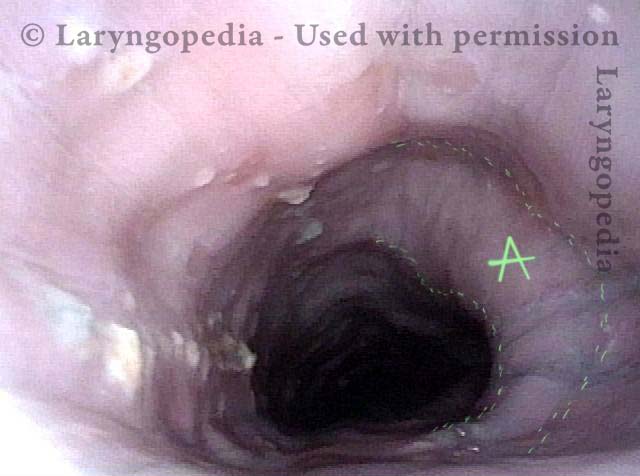
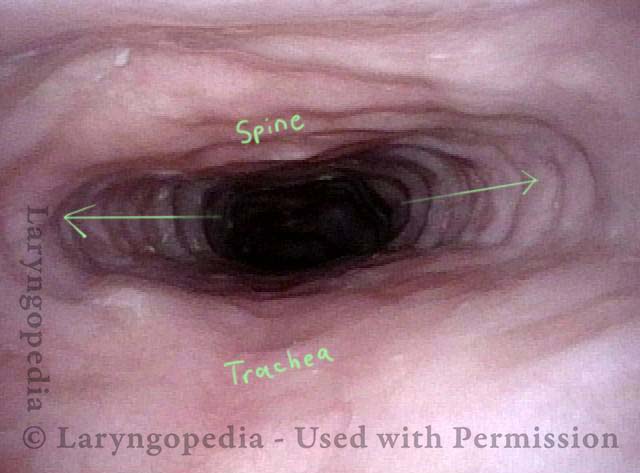
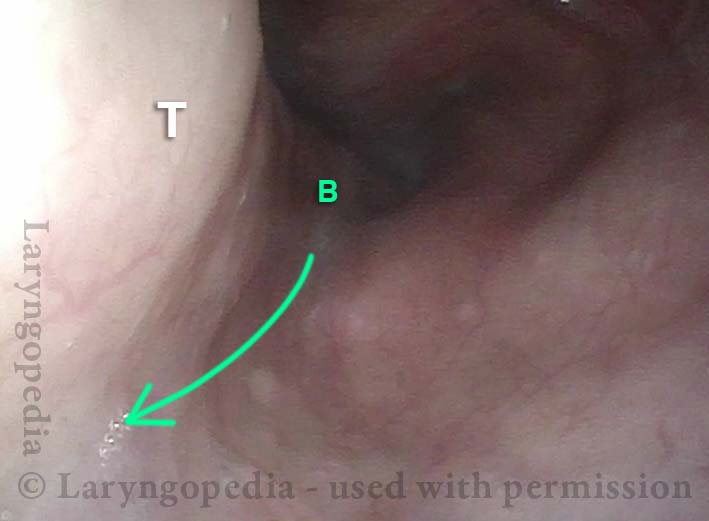
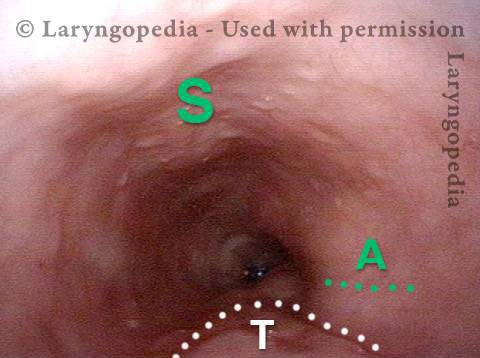
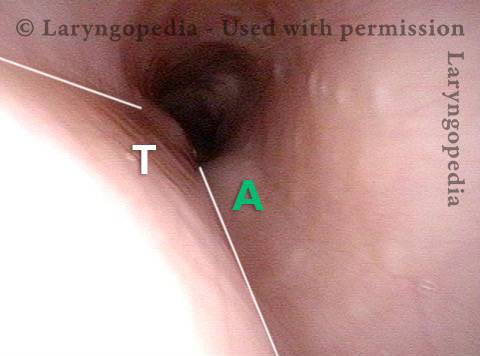
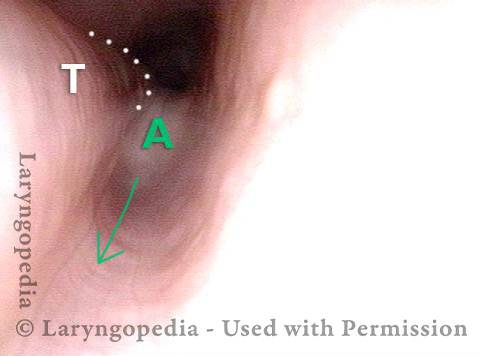
The esophagus is typically collapsed around endoscopes inserted into them and air is pumped in through a tiny channel in order to gently expand the esophagus so that its walls can be seen. Here, the air the patient cannot belch/evacuate is doing that work for us. And the esophagus remains open for extended time, the full duration of the examination. See more photo essays…
Aortic shelf (1 of 3)
Aortic shelf (1 of 3)
Bony spur emerges due to stretched esophagus (2 of 3)
Bony spur emerges due to stretched esophagus (2 of 3)
Stretched esophagus due to unburpable air (3 of 3)
Stretched esophagus due to unburpable air (3 of 3)
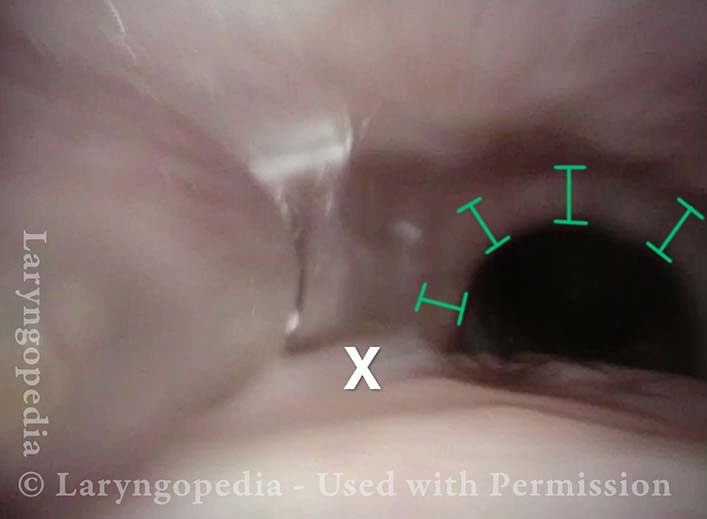
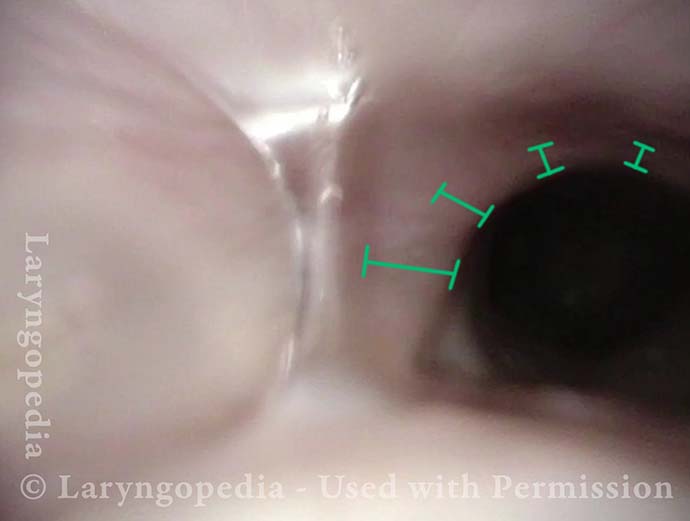
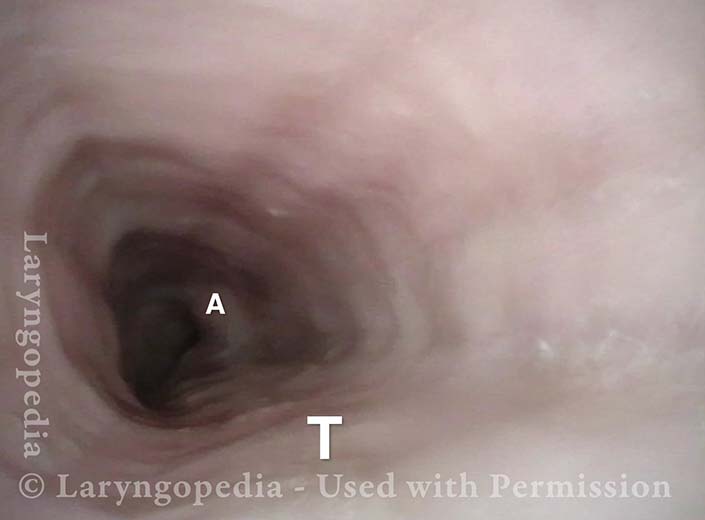
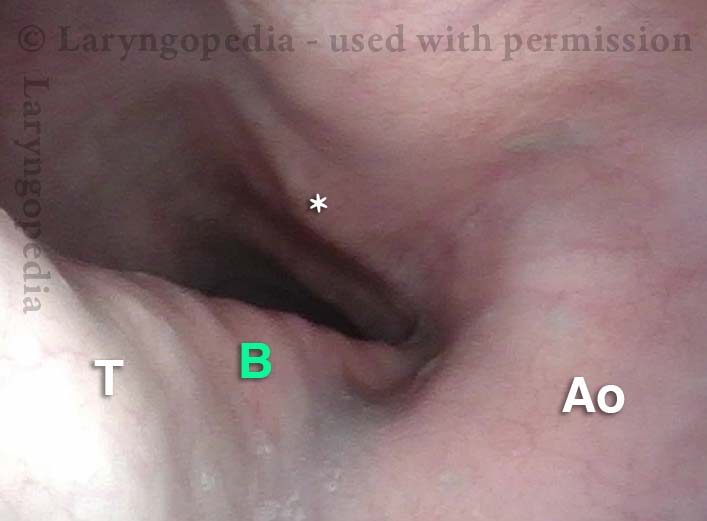
Airway, Foodway, Cricopharyngeus Muscle, and Esophagus in R-CPD
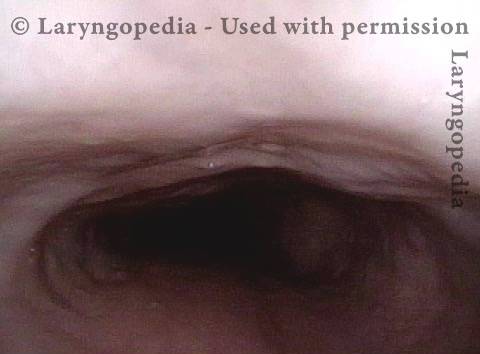
This young woman has never been able to burp normally. She experiences typical, severe R-CPD symptoms of daily bloating, loud gurgling noises, and excessive flatulence. Botulinum toxin injection of the cricopharyngeus muscle is planned to rid her of the syndrome of R-CPD in the short term, and to teach her how to burp “permanently” (even after the botulinum toxin has worn off).
Laryngopharynx (1 of 5)
Laryngopharynx (1 of 5)
Esophageal opening (2 of 5)
Esophageal opening (2 of 5)
Ridge of UES (3 of 5)
Ridge of UES (3 of 5)
Ridge of UES (4 of 5)
Ridge of UES (4 of 5)
Distended Esophagus (5 of 5)
Distended Esophagus (5 of 5)
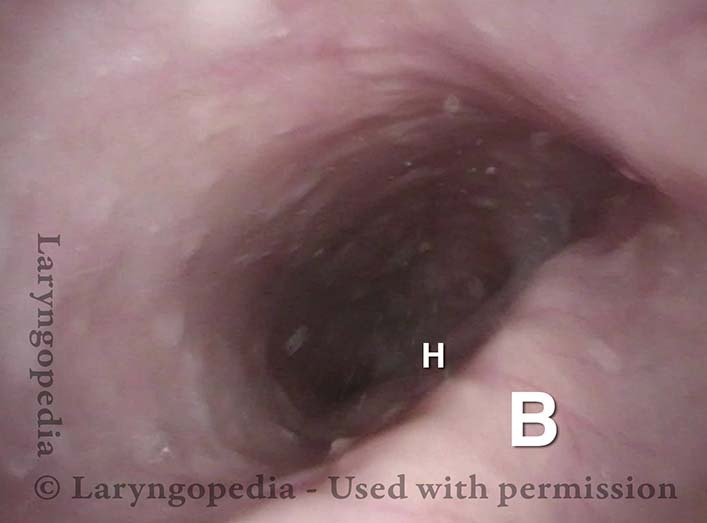
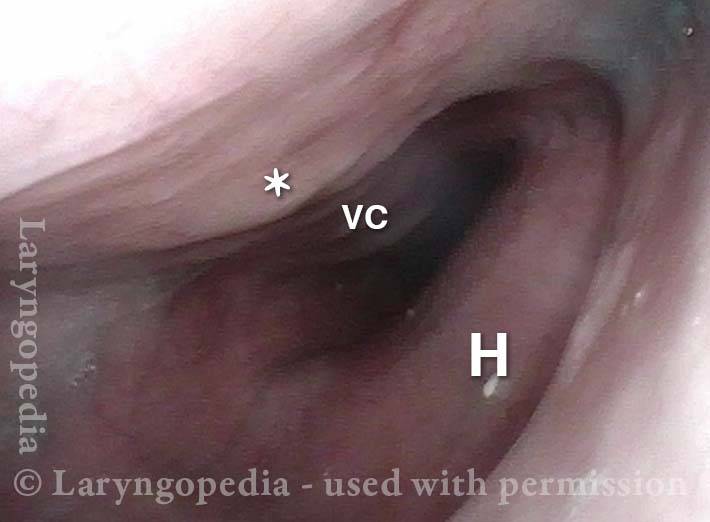
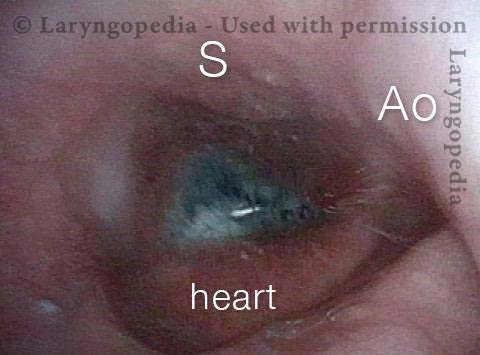
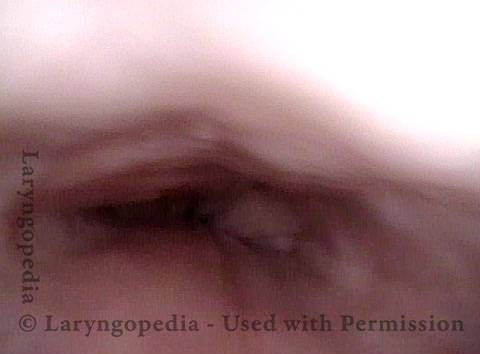
In R-CPD, Esophageal Findings May Correlate with Symptoms
This middle-aged patient has suffered all her life with inability to burp, and symptoms seem to be ever increasing. Currently, she has all 3 levels of pressure/bloating: abdomen, chest, and neck. Her abdomen often distends to “8 months pregnant” by end of day, and is flat in the morning after an evening/night of flatulence.
Abdominal symptoms are constant; when chest symptoms occur (pressure, etc.) they are even more uncomfortable. Her office upper esophagoscopy using a 3.7 mm ENT scope without air insufflation shows typical findings:
- The column of her own un-burped air, holding the esophagus in “always open” position all the way to the gastro-esophageal junction; tracheal mound, and aortic shelf.
- More than in most cases, the left mainstem bronchus is shown in high relief.
Distended upper esophagus (1 of 4)
Distended upper esophagus (1 of 4)
Distended mid-esophagus (2 of 4)
Distended mid-esophagus (2 of 4)
Left-mainstem bronchus (3 of 4)
Left-mainstem bronchus (3 of 4)
View includes open lower esophageal sphincter (4 of 4)
View includes open lower esophageal sphincter (4 of 4)
Dramatic esophageal dilation from R-CPD, even in a young person!
The central problem for persons with R-CPD is (obviously) the inability to burp. Bits of air travel through the upper esophageal sphincter (cricopharyngeus muscle) which closes behind each swallow.
Even as the air builds up, expanding the esophagus and sending increasing signals of the need to burp, the air is unable to “get back out” via burping. Initial discomfort from stuck burps-in-waiting may elicit reflexive “extra” swallows that only add more air that cannot be burped.
Gradually this dilates the esophagus (and eventually the stomach, and as air traverses the GI tract, the intestines all the way to the rectum, where it must be released as flatulence). Even in young people, esophageal dilation can be dramatic, causing chest discomfort.
The images below are from the office examination of a teenager sitting in the examination chair with a small ENT scope in his esophagus. The column of air he cannot burp up is holding the esophagus widely open. No air has been insufflated through the scope. The stretched esophagus throws structures outside it into high relief as seen below.
Stretched esophagus (1 of 3)
Stretched esophagus (1 of 3)
Mid-esophagus (2 of 3)
Mid-esophagus (2 of 3)
Stretching esophagus (3 of 3)
Stretching esophagus (3 of 3)
Esophageal Stretching by Unburpable Air in R-CPD
This young man has had the classic syndrome of R-CPD lifelong. His esophageal findings at the end of a videoendoscopic swallow study are classic. The esophagus is mostly a collapsed muscular tube in young people, yet his esophagus is widely open on a continuous basis due swallowed air that he cannot burp up.
Typical view of an esophagus (1 of 4)
Typical view of an esophagus (1 of 4)
Lower esophagus (2 of 4)
Lower esophagus (2 of 4)
Stretched mid-esophagus (3 of 4)
Stretched mid-esophagus (3 of 4)
Esophagus stretches laterally (4 of 4)
Esophagus stretches laterally (4 of 4)
More Interesting Esophageal Findings of R-CPD (Inability to Burp)
Stretched Esophagus (1 of 4)
Stretched Esophagus (1 of 4)
Tracheal Wall (2 of 4)
Tracheal Wall (2 of 4)
Over-dilation (3 of 4)
Over-dilation (3 of 4)
Bronchus is visible (4 of 4)
Bronchus is visible (4 of 4)
R-CPD and Esophageal Dilation
Posterior pharyngeal wall (1 of 3)
Posterior pharyngeal wall (1 of 3)
Is it R-CPD? (2 of 3)
Is it R-CPD? (2 of 3)
Stretched esophagus indicates R-CPD (3 of 3)
Stretched esophagus indicates R-CPD (3 of 3)
What the Esophagus Can Look Like “Below A Burp”
Baseline (1 of 3)
Baseline (1 of 3)
Pre-burp (2 of 3)
Pre-burp (2 of 3)
Post-burp (3 of 3)
Post-burp (3 of 3)
Click on a heading above to expand.
![]()
Videos about R-CPD
In-Office Injection of Botox for R-CPD | EMG-Guidance Compared to O.R. Esophagoscopy
Thankfully, awareness and availability of treatment for R-CPD are growing around the world. The often-permanent solution is botulinum toxin ("Botox") injection into the malfunctioning cricopharyngeus muscle.
There are two main approaches: one performed under brief general anesthesia through the mouth in an operating room, and another done in a clinic setting by injecting through the front or side of the lower neck using EMG (electromyographic) guidance with partial local anesthesia.
In this video, Dr. Bastian explains both techniques, with a special focus on the EMG-guided office procedure.What to Expect During the Initial Weeks After Botox Injection
A person with R-CPD (no-burp) who is considering undergoing treatment may encounter "concerning" comments online, such as on the Reddit no-burp site, or the R-CPD Facebook group. Such a comment might be an "outlier" result, but the reader may not know that. And so the comment can create a worry or question in the mind of a prospective patient. They might wonder "Is this going to happen to me?”
To address this potential scenario, this video explains systematically what happens to burping, swallowing, breathing, and voice after botox injection into the cricopharyngeus muscle to resolve inability to burp. The viewer should be reassured....Laryngospasm after Botox Injection for R-CPD - How to Avoid It
Persons with no-burp, aka retrograde cricopharyngeus dysfunction (R-CPD) can usually learn to burp with the help of a single botulinum toxin (botox) injection ("once and done" in about 80%). The diagnosis and treatment are remarkably straightforward.
BUT...about one of 200 or so experience laryngospasms after the treatment and this is a source of anxiety for some considering the procedure. This video explains why laryngospasm occasionally occurs in this scenario and how to avoid it.
Emetophobia and R-CPD | Can You Overcome the Fear?
Some people experience exaggerated and even debilitating fear of vomiting. They may panic at the very thought, and require psychotherapy. The term for this is emetophobia, and it occurs in perhaps one person per thousand of the general population.
But it may occur far more frequently—in as many as one of three persons—who have a condition called retrograde cricopharyngeus dysfunction (R-CPD, aka "no-burp"). Dr. Bastian explains why this might be, and what effect the successful treatment of R-CPD may have on emetophobia.
How to Keep the Ability to Burp After Botox Treatment for R-CPD
R-CPD can thankfully be treated successfully with a simple outpatient injection of Botox into a muscle in the upper esophagus. Since the Botox effect on the muscle serves as "training wheels" for burping, about 4 out of 5 people are "cured" by a single treatment. That's why we aim for "once and done" treatment.
Dr. Bastian describes here how to maximize the likelihood that the ability to burp will continue after Botox has worn off.
Complications Compared to Expected Effects in Treatment of R-CPD
In this video, Dr. Bastian distinguishes the difference between early EFFECTS that are expected, and COMPLICATIONS patients have experienced in a caseload of approximately 870 people. This informal discussion will likely reassure persons considering this treatment for the severe daily misery caused by R-CPD.R-CPD Webinar
A live R-CPD (no-burp) Webinar hosted by Dr. Bastian on July 26, 2022 at 6 p.m. CSTQ&A—Part I
Dr. Bastian answers a list of questions submitted by our R-CPD webinar attendees.Q&A—Part II
In Part 2 of the R-CPD Q&A, Dr. Bastian answers more questions submitted by our webinar attendees.R-CPD Panel - U.S. Doctors Discuss R-CPD
A panel of expert discussion on R-CPD (aka “No-Burp Syndrome”) featuring questions and answers from leaders in the field.Your Common Questions about R-CPD
Dr. Bastian responds to a list of questions submitted through YouTube, Facebook, and Instagram.What Surprises No-burpers about People who Can Burp
Here are a few things that surprise people who can’t burp, about people who can! (This is especially for those with R-CPD aka no-burp).What Is the Best Botox Dose for R-CPD? 100 units? 50? 200?
Newly diagnosed R-CPD patients often ask: "What is the best dose for the initial injection of Botox?" Dr. Bastian provides an answer that includes context and nuance from his group's experience with over 1200 patients injected to date.RCPD Workup - Do You Need Testing for a Diagnosis?
What is necessary to diagnose R-CPD? What is sufficient? Do we need to spend thousands of dollars for x-rays, manometry, upper GI scopes, gastric emptying studies?What if Botox Doesn’t Work for My R-CPD? | High Quality Injections
Rarely, treatment of R-CPD (no-burp) with botox fails to initiate burping. Why might that be? Is the diagnosis wrong? Was the dose of botox Inadequate? Was the target missed? Dr. Bastian explores these possibilities...What is the Relationship between R-CPD and GERD? SIBO? IBS?
Often, and almost routinely, persons with easily-diagnosed R-CPD may initially be diagnosed instead as "gastroesophageal reflux disease" (GERD), or "irritable bowel syndrome," (IBS) or "small intestine bacterial overgrowth" (SIBO).
Do GERD, IBS, and SIBO symptoms and findings point to coexisting and separate diagnoses, or are those symptoms part of the larger, umbrella diagnosis of R-CPD? Dr. Bastian discusses these questions in this video.
My Baby Can't Burp! This May Explain Why
“My baby can’t burp!" "He/she cries with colic, sometimes for a long time." "So much spitting up and even projectile vomiting!" "I’ve never seen such a gassy baby!” Babies and older children with this condition are in misery, and so are their parents, with the stress of it all. The answer might be R-CPD.
When such babies grow older, those with severe cases of R-CPD may refuse to eat, and may continue to complain of stomach distress. In this video, Dr. Robert Bastian explains this “new” diagnosis that can cause all of these symptoms. Parents who are exhausted and depressed may find here a glimmer of hope.
Do Shaker Exercises Work in Treating R-CPD?
In this video, Dr. Bastian explains his thinking about “Shaker Exercises” as a means of learning to burp in persons with R-CPD (no-burp). A recent Reddit thread was created in response to his July 2022 Webinar comments on this subject, and it appeared to him that he had not conveyed his thinking clearly enough. Here is his more detailed and nuanced discussion…What about Dilation along with Botox injection for R-CPD?
R-CPD (the no-burp syndrome) has been clearly described. Thousands of patients have been "cured" by injecting botox into the upper esophageal sphincter (cricopharyngeus muscle). Still, the question occasionally arises: Is there added value to dilation of the sphincter? Dr. Bastian explains why he thinks the answer is “no."![]()
Dr. Bastian’s Published R-CPD Articles
Dr. Bastian’s Initial Article about R-CPD
Inability to Belch and Associated Symptoms Due to Retrograde Cricopharyngeus Dysfunction: Diagnosis and Treatment
March 15, 2019
Partial Cricopharyngeal Myotomy for Treatment of Retrograde Cricopharyngeal Dysfunction
April 16, 2020
The Long-term Efficacy of Botulinum Toxin Injection to Treat Retrograde Cricopharyngeus Dysfunction
June 29, 2020
Efficacy and Safety of Electromyography-Guided Injection of Botulinum Toxin to Treat Retrograde Cricopharyngeus Dysfunction
February 2, 2021
![]()
Additional R-CPD Resources
R-CPD Publications
Community Created Content

No-Burp: It's not just you
(33,000+ no-burpers)

Retrograde Cricopharyngeus Dysfunction (R-CPD)
[4,100+ members]

I can now burp
@Lilamycox

My weird medical history
@Brittcurls
My R-CPD journey
Julie Anne Gay
Map of Doctors who treat R-CPD
Map created by u/karybrie. None of these Doctors (besides Dr. Brent E Richardson and Dr. Rebecca C Hoesli) are affiliated with Dr. Robert W. Bastian or Laryngopedia. We cannot guarantee if any doctor on this map treats R-CPD.
See more entries about R-CPD
Share this article