¿No Puede Eructar?
La incapacidad para eructar o «eructar» (también conocida como disfunción cricofaríngea retrógrada o R-CPD para abreviar) ocurre cuando el esfínter esofágico superior (músculo cricofaríngeo) pierde su capacidad de relajarse para liberar la «burbuja» de aire.

¿Qué es R-CPD (incapacidad para eructar, no eructar)?
Las personas que no pueden liberar aire hacia arriba son miserables. Pueden sentir la «burbuja» asentada en la parte media y baja del cuello sin ningún lugar a donde ir. O experimentan gorgoteos cuando el aire sube por el esófago y descubren que la vía de escape está bloqueada por un esfínter que no se relaja. Es como si el músculo del esófago se agitara y apretara continuamente sin éxito. Los síntomas comunes incluyen la incapacidad para eructar, ruidos de gorgoteo, presión e hinchazón en el pecho/abdomen, y flatulencia.

Los 4 síntomas principales de R-CPD
Incapacidad para eructar
Esto es casi siempre, pero no exclusivamente, “de por vida”, aunque es posible que las personas no lo reconozcan como un “problema” o una “diferencia con los demás” hasta la primera infancia o la adolescencia.

Ruidos de gorgoteo socialmente incómodos
Estos ruidos pueden ser en su mayoría silenciosos e «internos», pero con mayor frecuencia son lo suficientemente fuertes como para ser vergonzosos. La apertura de la boca los hace más ruidosos. Casi todos dicen que se les escucha fácilmente a varios metros de distancia; no pocas veces “hasta la puerta”. Engendran ansiedad social en la mayoría de las personas con R-CPD, lo que hace que algunas eviten comer o beber horas antes de las ocasiones sociales e incluso durante ellas. La carbonatación los empeora mucho y debe evitarse a toda costa. Algunas descripciones de pacientes más coloridas:
- Sinfonía de gorgoteos
- Ranas croando
- Tablas del suelo que crujen
- Sonidos de dinosaurios
- Ballena estrangulada.
- El Exorcista
Hinchazón y Presión
La localización más frecuente es el abdomen central alto. La distensión es común, especialmente más tarde en el día. Usando el embarazo como una analogía incluso en los hombres, el grado habitual de distensión se describe como «3 o 4 meses». “Seis meses” no es raro, y un joven delgado estaba “a término”. Casi tan a menudo como el malestar abdominal, los pacientes describen presión en el pecho y, para algunos, ese es el peor síntoma. Algunos tienen presión en la parte baja del cuello. Si bien “presión” es el descriptor frecuente, algunos experimentan dolor agudo ocasional en el abdomen, la espalda o entre los omóplatos. Algunos tienen que acostarse después de comer para encontrar algo de alivio.
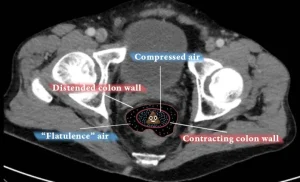
Flatulencia
Rutinariamente, esto se describe como «importante» o incluso «ridículo». La flatulencia aumenta a medida que avanza el día y muchos la experimentan durante la noche. Cuando están cerca de otros, algunos escanean su entorno en todo momento en busca de un lugar al que puedan ir brevemente para expulsar gases. Comprensiblemente, las ramificaciones sociales de este problema también pueden ser importantes.

Síntomas menos comunes de R-CPD
Náuseas
especialmente después de comer cantidades más grandes de lo normal o beber bebidas carbonatadas.
Hipersalivación
cuando los síntomas de hinchazón son importantes.
Hipo doloroso
de nuevo, más comúnmente después de comer.
Ansiedad e inhibición social.
Esto puede ser IMPORTANTE debido al gorgoteo, la flatulencia y la incomodidad.
Dificultad para respirar
Una persona puede estar tan llena de aire que el atletismo, o incluso la capacidad de subir escaleras, se ve afectada.
constipación
(Aún en evaluación): no siempre se puede responder a la flatulencia, y el resultado es que el colon descendente parece dilatarse, lo que hace que los músculos estirados en su pared sean menos efectivos para mover el contenido del colon.
Incapacidad para vomitar
Algunos simplemente no pueden vomitar; más a menudo es posible, pero sólo después de arcadas extenuantes. Los vómitos (espontáneos o autoinducidos) siempre comienzan con un ruido muy fuerte y una gran liberación de aire en un fenómeno que llamamos “vómitos de aire”. La emetofobia puede ser importante.

¿Qué causa la R-CPD?
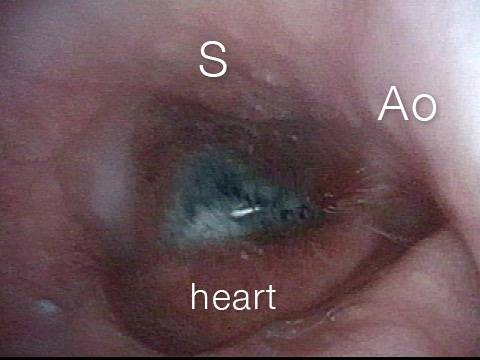
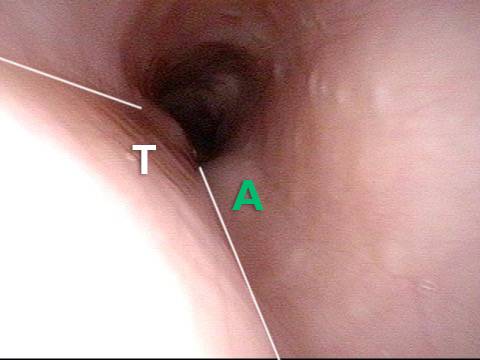
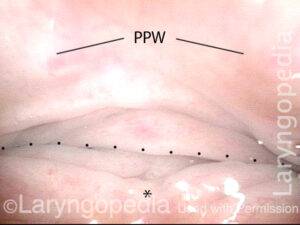
La incapacidad para eructar o eructar ocurre cuando el esfínter esofágico superior (músculo cricofaríngeo) no puede relajarse para liberar la «burbuja» de aire. El esfínter es una válvula muscular que rodea el extremo superior del esófago justo debajo del extremo inferior del conducto de la garganta. Si mira de frente el cuello de una persona, está justo debajo de la “nuez de Adán/Eva”, directamente detrás del cartílago cricoides.
Si desea ver esto en un modelo, mire la foto a continuación. Ese músculo del esfínter se relaja durante aproximadamente un segundo cada vez que tragamos saliva, comida o bebida. Todo el resto del tiempo se contrata. Siempre que una persona eructa, el mismo esfínter necesita soltarse durante una fracción de segundo para que el exceso de aire escape hacia arriba. En otras palabras, así como es necesario que el esfínter se “suelte” para admitir alimentos y bebidas hacia abajo en el acto normal de la deglución, también es necesario que el esfínter pueda “soltarse” para dejar salir el aire hacia arriba para eructar.
Las personas que no pueden liberar aire hacia arriba son miserables. Pueden sentir la «burbuja» asentada en la parte media y baja del cuello sin ningún lugar adonde ir. O experimentan gorgoteos cuando el aire sube por el esófago y es bloqueado por un esfínter que no se relaja. Es como si el músculo del esófago se agitara y apretara continuamente sin éxito. La persona quiere y necesita eructar, pero no puede. A veces esto puede incluso ser doloroso. Estas personas a menudo experimentan distensión abdominal ya que el aire debe atravesar los intestinos antes de ser finalmente liberado en forma de flatos.
Haga clic para ampliar. Arrastre para deslizar.

Tratamiento para R-CPD
Inyección de Botox en Bastian Voice Institute
Para las personas que experimentan este problema hasta el punto de la incomodidad y la reducción de la calidad de vida, aquí hay un enfoque: primero, un estudio videofluoroscópico de deglución, quizás con gránulos efervescentes. Esto establece que el esfínter funciona normalmente en una dirección de deglución hacia adelante (anterógrada), pero no en una dirección de eructo o regurgitación inversa (retrógrada). Junto con los síntomas descritos anteriormente, esto establece el diagnóstico de disfunción cricofaríngea retrógrada solamente (falta de relajación).
En segundo lugar, una prueba de tratamiento que involucra la colocación de Botox en el músculo del esfínter que funciona mal. El efecto deseado del Botox en el músculo es debilitarlo durante al menos varios meses. La persona tiene así muchas semanas para comprobar que el problema se soluciona o al menos se minimiza. La inyección de Botox podría potencialmente realizarse en un consultorio, pero recomendamos la primera vez (al menos) colocarla durante una breve anestesia general en un quirófano ambulatorio. Eso es porque la primera vez, es importante responder a la pregunta de manera definitiva, es decir, que el problema es la incapacidad del esfínter para relajarse cuando se le presenta una burbuja de aire desde abajo.
Al menos durante unos meses, los pacientes deberían experimentar un alivio espectacular de sus síntomas. Y, la experiencia temprana sugiere que puede ser que esta sola inyección de Botox permita que el sistema se «reinicie» y que la persona nunca pierda su capacidad de eructar. Por supuesto, si el problema reaparece, la persona podría optar por seguir tratamientos adicionales con Botox o, en un caso realmente grave, incluso podría optar por someterse a una miotomía cricofaríngea con láser endoscópica.
Complicaciones en comparación con los efectos esperados en el tratamiento de R-CPD
En este video, el Dr. Bastian distingue la diferencia entre los EFECTOS tempranos que se esperan y las COMPLICACIONES que los pacientes han experimentado en un número de casos de aproximadamente 870 personas. Esta discusión informal probablemente tranquilizará a las personas que estén considerando este tratamiento por la miseria diaria severa causada por el R-CPD.
¿Cuál es la mejor dosis de Botox para R-CPD? 100 unidades? 50? 200?
Los pacientes con R-CPD recién diagnosticados a menudo preguntan: «¿Cuál es la mejor dosis para la inyección inicial de Botox?» El Dr. Bastian brinda una respuesta que incluye contexto y matices de la experiencia de su grupo con más de 1200 pacientes inyectados hasta la fecha.
¿Funcionan los ejercicios Shaker en el tratamiento de R-CPD?
En este video, el Dr. Bastian explica su pensamiento sobre los «Ejercicios Shaker» como un medio para aprender a eructar en personas con R-CPD (sin eructos). Se creó un hilo de Reddit reciente en respuesta a sus comentarios del seminario web de julio de 2022 sobre este tema, y le pareció que no había transmitido su pensamiento con la suficiente claridad. Aquí está su discusión más detallada y matizada…

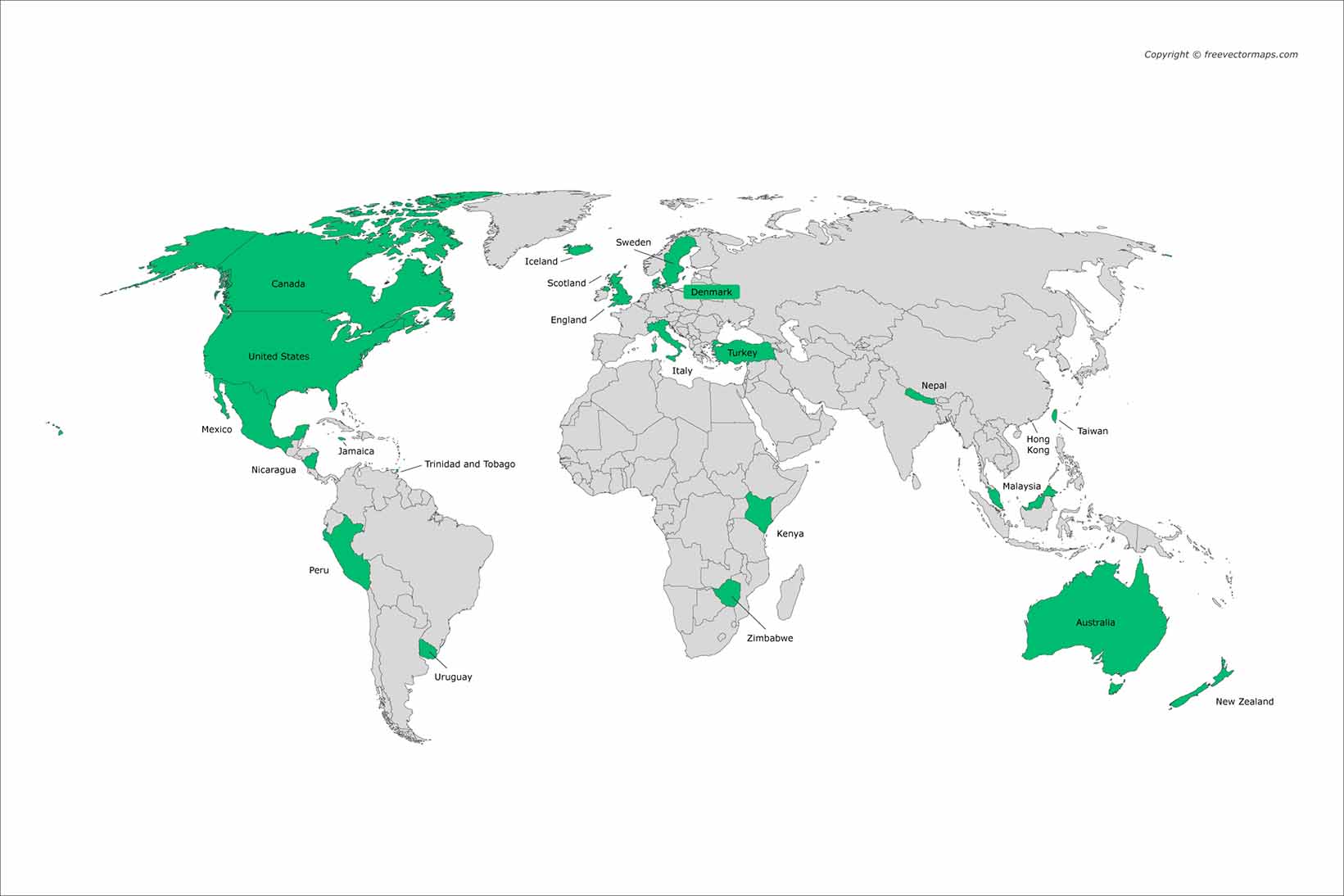
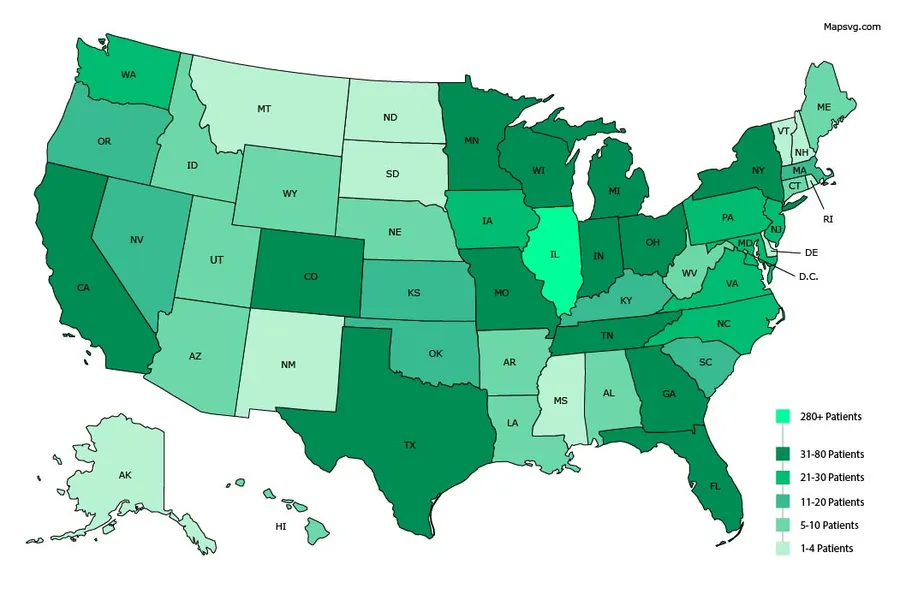
De dónde vienen nuestros pacientes con R-CPD

Ensayos fotográficos de nuestros pacientes con R-CPD
Distensión abdominal de R-CPD
Gastric Air Bubble (1 of 3)
Gastric Air Bubble (1 of 3)
Bloated Abdomen (2 of 3)
Bloated Abdomen (2 of 3)
Non-bloated Abdomen (3 of 3)
Non-bloated Abdomen (3 of 3)
Progresión de la hinchazón y la distensión abdominal: un ciclo diario para muchos con R-CPD
Esta joven tiene los síntomas clásicos de R-CPD: el síndrome de no poder eructar. Temprano en el día, sus síntomas son mínimos y el abdomen está en la «línea de base» porque se ha «desinflado» a través de la flatulencia durante la noche. En esta serie se ve la diferencia en su distensión abdominal entre temprano y tarde en el día. Las imágenes de rayos X muestran la notable cantidad de aire retenido que explica su hinchazón y distensión. Su progresión es bastante típica; algunos con R-CPD se distienden incluso más de lo que se muestra aquí, especialmente después de comer una comida copiosa o consumir algo carbonatado.
Side view of a bloated abdomen (1 of 6)
Side view of a bloated abdomen (1 of 6)
Front view (2 of 6)
Front view (2 of 6)
Greater Distention (3 of 6)
Greater Distention (3 of 6)
Front view of bloating stomach (4 of 6)
Front view of bloating stomach (4 of 6)
X-ray of trapped air (5 of 6)
X-ray of trapped air (5 of 6)
Side view (6 of 6)
Side view (6 of 6)
Una rara "crisis abdominal" debido a R-CPD (incapacidad para eructar)
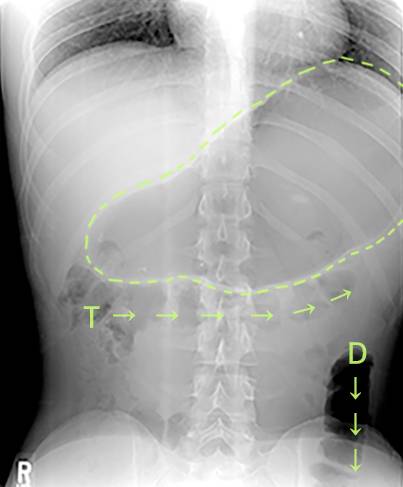
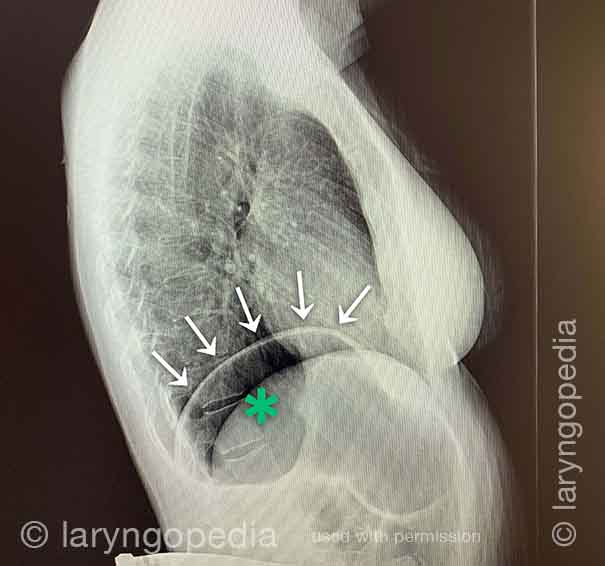
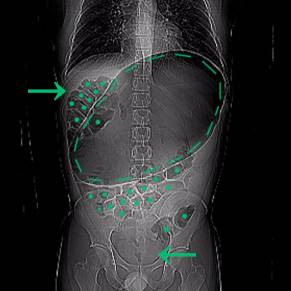
Este joven tenía una crisis abdominal relacionada con R-CPD. Ha tenido síntomas de por vida de R-CPD clásico: incapacidad para eructar, gorgoteo, hinchazón y flatulencia. Durante un momento de particular incomodidad, lamentablemente tomó un “remedio” que era carbonatado. Aquí se ve una enorme burbuja de aire en el estómago. Muchos de sus intestinos están llenos de aire y presionados hacia arriba y hacia su derecha (a la izquierda de la foto, en la flecha). La presión interna dentro de su abdomen también cortó su capacidad de expulsar gases.
X-Ray of Abdominal Bloating (1 of 2)
X-Ray of Abdominal Bloating (1 of 2)
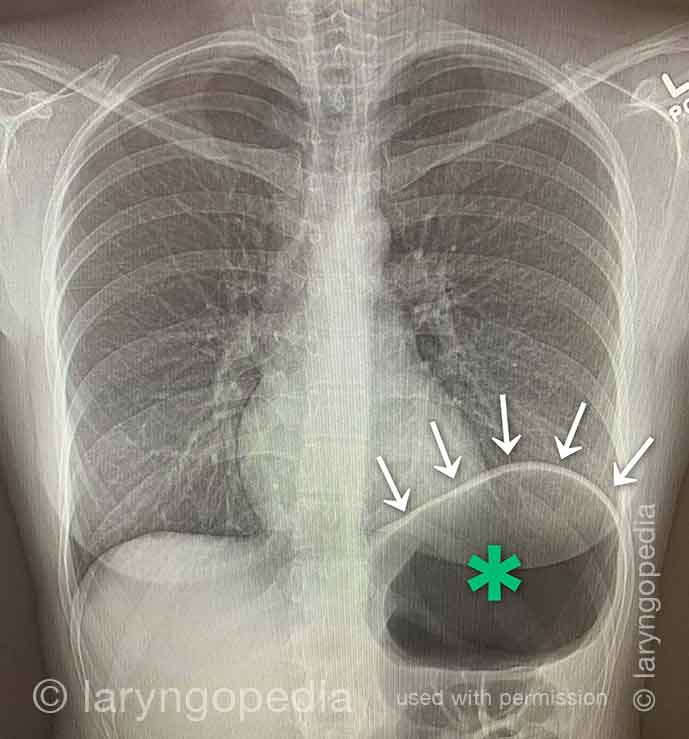
Dificultad para respirar causada por no eructar
Las personas que no pueden eructar y tienen el síndrome R-CPD completo a menudo dicen que cuando la hinchazón y la distensión son particularmente malas, y especialmente cuando tienen una sensación de presión en el pecho, también tienen una sensación de dificultad para respirar. Dirán, por ejemplo, “Soy un [cantante, o corredor, o ciclista o _____], pero mi habilidad está muy disminuida por R-CPD. Si estoy compitiendo o actuando, no puedo comer ni beber durante las 6 horas anteriores”. Algunos incluso dicen que no pueden completar un bostezo cuando los síntomas son particularmente graves. Las radiografías a continuación explican cómo la incapacidad para eructar puede causar dificultad para respirar.
X-ray of trapped air (1 of 2)
X-ray of trapped air (1 of 2)
Side view (2 of 2)
Side view (2 of 2)
Hallazgos esofágicos
Aortic shelf (1 of 3)
Aortic shelf (1 of 3)
Bony spur emerges due to stretched esophagus (2 of 3)
Bony spur emerges due to stretched esophagus (2 of 3)
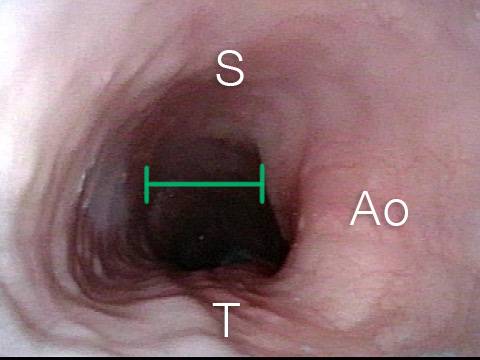
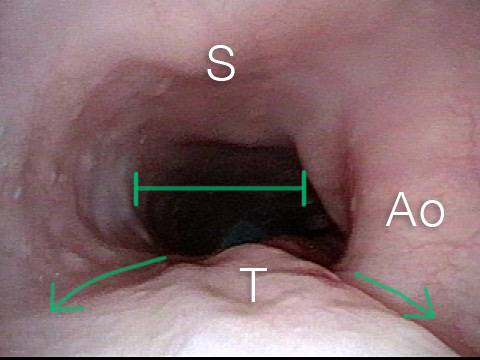
Stretched esophagus due to unburpable air (3 of 3)
Stretched esophagus due to unburpable air (3 of 3)
Estiramiento esofágico por aire no burpable en R-CPD
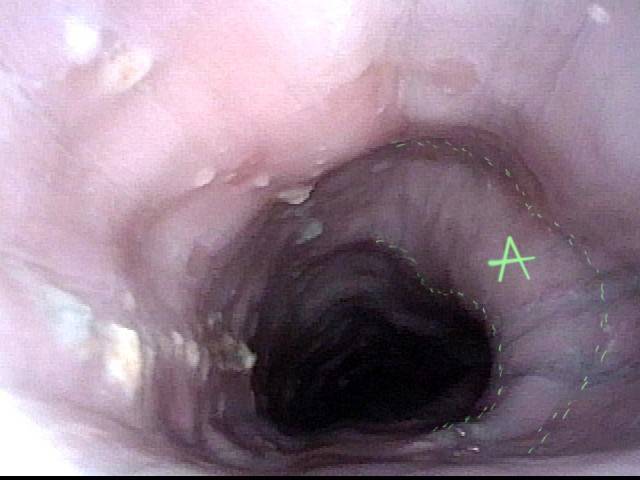
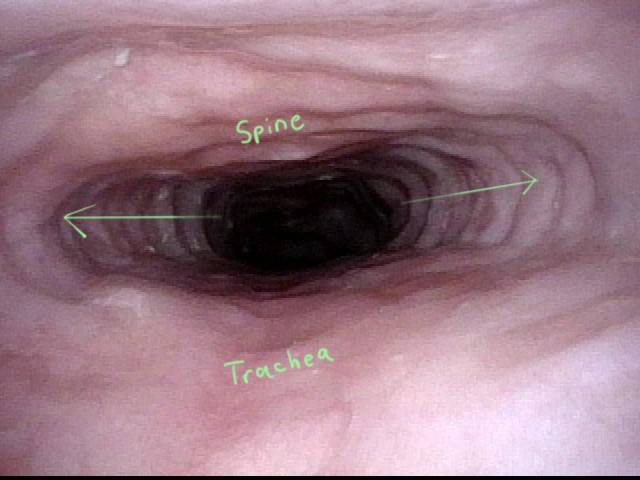
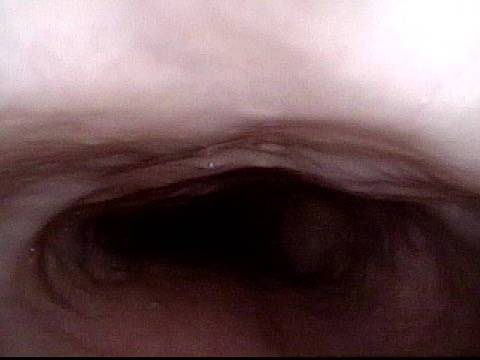
Este joven ha tenido el síndrome clásico de R-CPD durante toda su vida. Sus hallazgos esofágicos al final de un estudio videoendoscópico de deglución son clásicos. El esófago es principalmente un tubo muscular colapsado en personas jóvenes, sin embargo, su esófago está muy abierto de forma continua debido al aire que traga y que no puede eructar.
Typical view of an esophagus (1 of 4)
Typical view of an esophagus (1 of 4)
Lower esophagus (2 of 4)
Lower esophagus (2 of 4)
Stretched mid-esophagus (3 of 4)
Stretched mid-esophagus (3 of 4)
Esophagus stretches laterally (4 of 4)
Esophagus stretches laterally (4 of 4)
Abdominal Distention Caused by R-CPD
Este hombre de sesenta y tantos ha soportado la miseria de R-CPD toda su vida. Sus síntomas de incapacidad para eructar, gorgoteo, distensión abdominal, flatulencia (y más) se alivian drásticamente después de aplicar la toxina botulínica en el músculo cricofaríngeo (esfínter esofágico superior). Aquí, también vemos la diferencia de antes y después en su distensión abdominal.
Bloating and abdominal distention before botox injection for inability to burp (1 of 2)
Bloating and abdominal distention before botox injection for inability to burp (1 of 2)
Resolved, one month after botox, with burping restored (2 of 2)
Resolved, one month after botox, with burping restored (2 of 2)
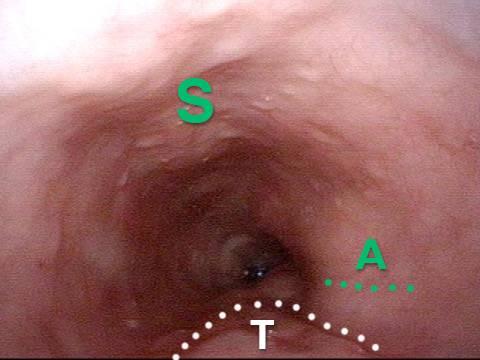
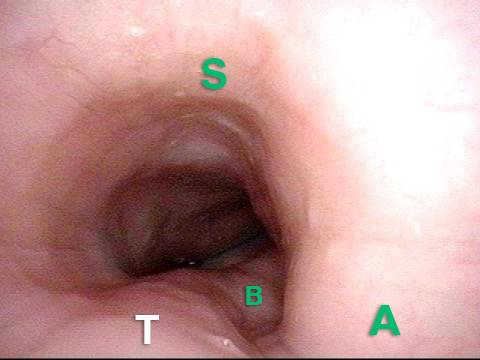
Hallazgos esofágicos más interesantes de R-CPD (incapacidad para eructar)
Stretched Esophagus (1 of 4)
Stretched Esophagus (1 of 4)
Tracheal Wall (2 of 4)
Tracheal Wall (2 of 4)
Over-dilation (3 of 4)
Over-dilation (3 of 4)
Bronchus (4 of 4)
Bronchus (4 of 4)
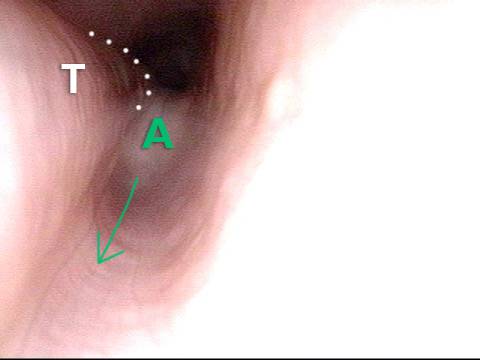
R-CPD y dilatación esofágica
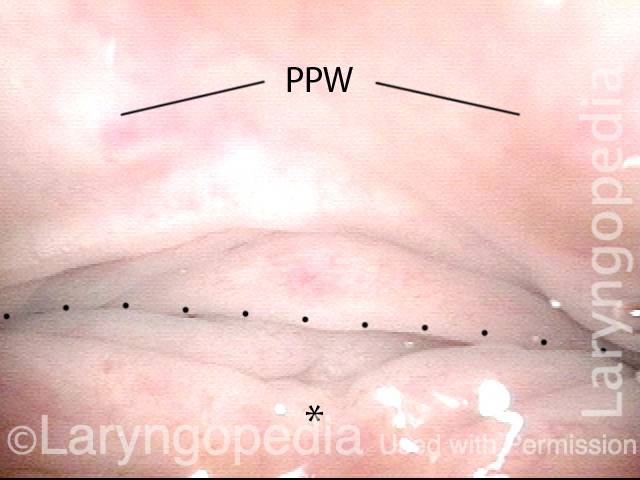
Posterior pharyngeal wall (1 of 3)
Posterior pharyngeal wall (1 of 3)
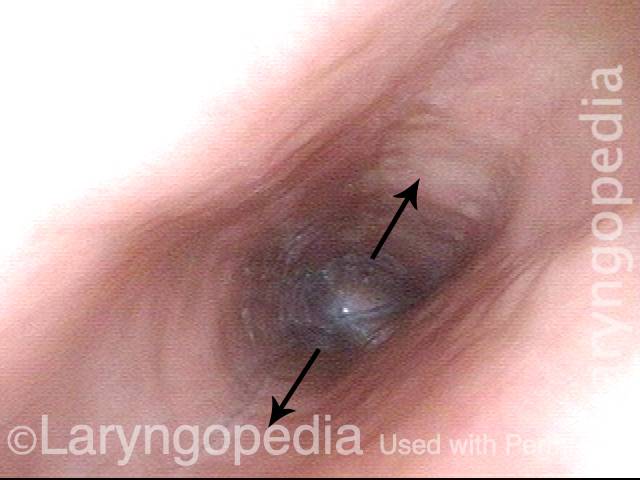
Is it R-CPD? (2 of 3)
Is it R-CPD? (2 of 3)
Stretched esophagus indicates R-CPD (3 of 3)
Stretched esophagus indicates R-CPD (3 of 3)
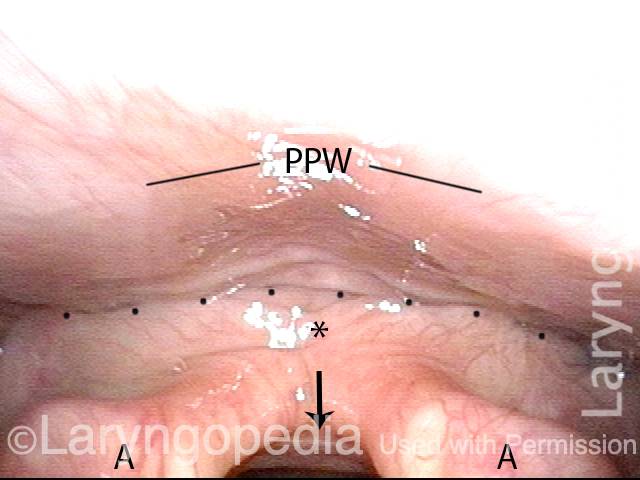
Cómo puede verse el esófago "debajo de un eructo"
Baseline (1 of 3)
Baseline (1 of 3)
Pre-burp (2 of 3)
Pre-burp (2 of 3)
Post-burp (3 of 3)
Post-burp (3 of 3)

Recursos adicionales de R-CPD
Artículos publicados del Dr. Bastian
Artículo inicial del Dr. Bastian sobre R-CPD
Inability to Belch and Associated Symptoms Due to Retrograde Cricopharyngeus Dysfunction: Diagnosis and Treatment
Read more →
March 15, 2019
Partial Cricopharyngeal Myotomy for Treatment of Retrograde Cricopharyngeal Dysfunction
Read More →
April 16, 2020
The Long-term Efficacy of Botulinum Toxin Injection to Treat Retrograde Cricopharyngeus Dysfunction Read More →
June 29, 2020
Efficacy and Safety of Electromyography-Guided Injection of Botulinum Toxin to Treat Retrograde Cricopharyngeus Dysfunction Read More →
February 2, 2021
Seminarios web de R-CPD

Panel R-CPD
Un panel de discusión de expertos sobre R-CPD (también conocido como «Síndrome sin eructos») con preguntas y respuestas de líderes en el campo.
R-CPD Webinar
Un seminario web en vivo de R-CPD (sin eructos) organizado por el Dr. Bastian el 26 de julio de 2022 a las 6 p.m. CST
Q&A—Part I
El Dr. Bastian responde una lista de preguntas enviadas por los asistentes al seminario web de R-CPD.
Q&A—Part II
En la Parte 2 de las preguntas y respuestas de R-CPD, el Dr. Bastian responde una lista de preguntas enviadas por los asistentes al seminario web de R-CPD.
Véanos en las noticias
Contenido creado por la comunidad
Ver más artículos

Babies Who Cannot Burp, and Still Cannot as Adults.
Robert W. Bastian, M.D. — Published: July 1, 2021 The big picture Babies who cannot burp are in terrible misery. So are their parents. While
What to Expect After Botox Injection for R-CPD
Background of R-CPD R-CPD causes 4 primary symptoms: inability to belch, gurgling noises, bloating, and flatulence. Less universal symptoms include painful hiccups, nausea after large
Why Is Constipation Often a Symptom of Retrograde Cricopharyngeus Dysfunction (R-CPD)? A Thought Experiment
Introduction Retrograde cricopharyngeus dysfunction is also known by three other names: R-CPD; inability to burp and associated symptoms, or “no-burp.” Because of the inability to