Leukoplakia
Leukoplakia (leuko = white; plakia = plaque) is a white patch found on the mucosa anywhere in the body. In the larynx, it is most often seen on the vocal cords, either in long-time smokers or in individuals with some other cause of chronic inflammation, such as (controversially) acid reflux.
Leukoplakia is the visually descriptive term for what—on biopsy—may prove to be keratosis, carcinoma in situ, or carcinoma. Unfortunately, it is a stubborn and frustrating problem in laryngology, with a tendency to recur after removal.
Treatment
Some patients can achieve longterm remission, but not all…The strategy is serial microlaryngoscopies (as illustrated in the largest series below). We speak of possibly “winning territory but not the entire war” with each procedure. Some eventually remit; others seem to continue recurring after each procedure, indefinitely.
Cake Icing and Spilled Milk Leukoplakia after Covid in a Former Smoker
This is a person who had smoked ½ pack per day for a little over a decade but stopped nearly 15 years ago. Voice was always normal until Covid-19 infection (despite vaccination). Laryngitis occurred during that illness and never resolved across six months to the time of this examination.
He is hoarse but voice is functional for basic communication. After supportive (acid reflux, etc.) treatments failed to resolve these lesions, microlaryngoscopy with meticulous “basement membrane” peeling of these lesions will follow.
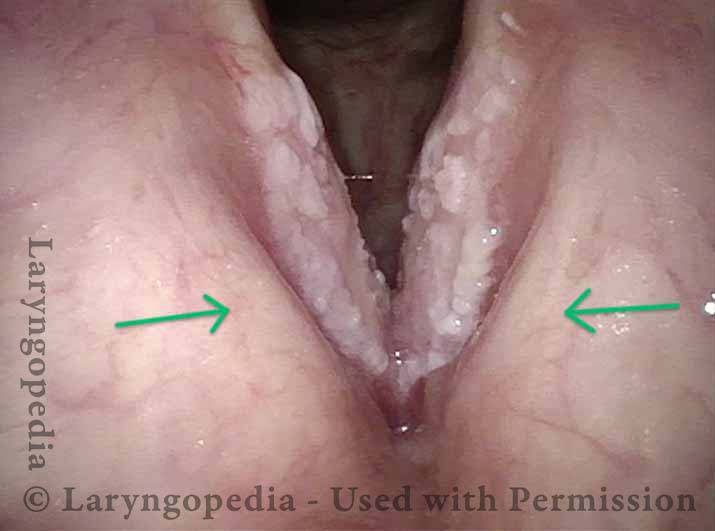
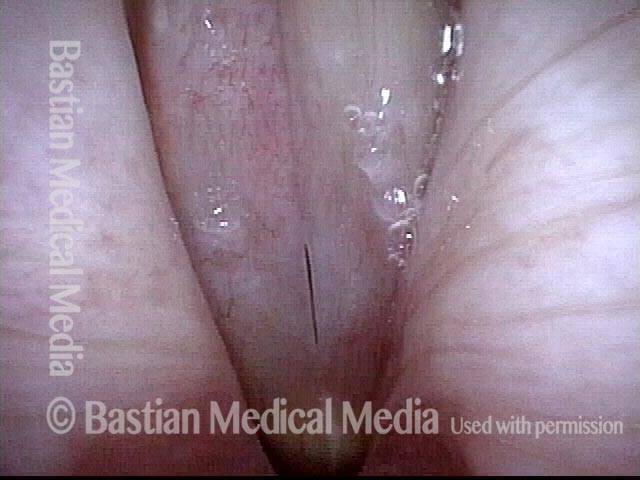
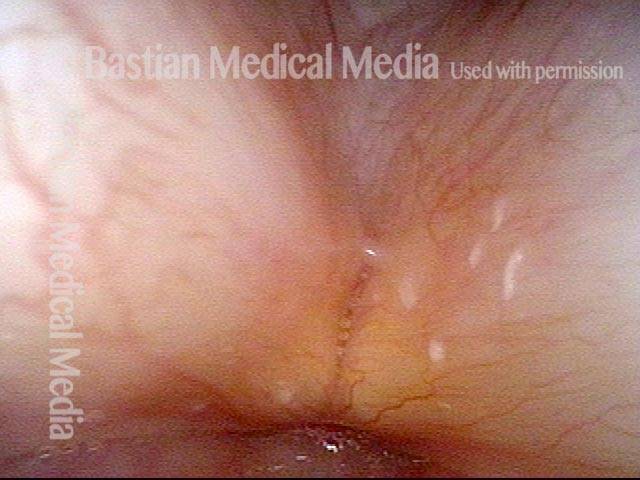
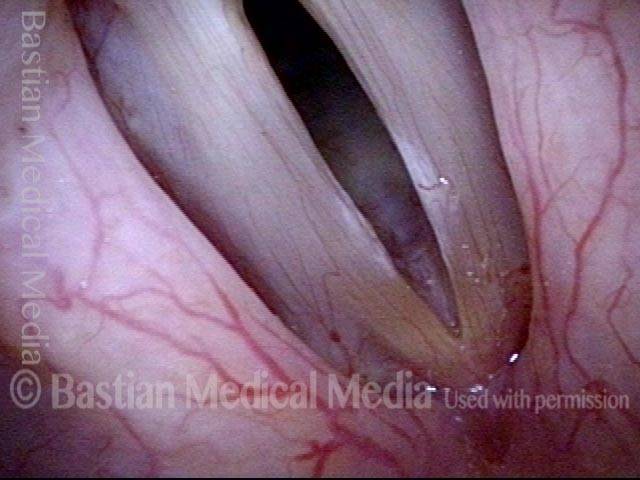
Leukoplakia (1 of 16)
Leukoplakia (1 of 16)
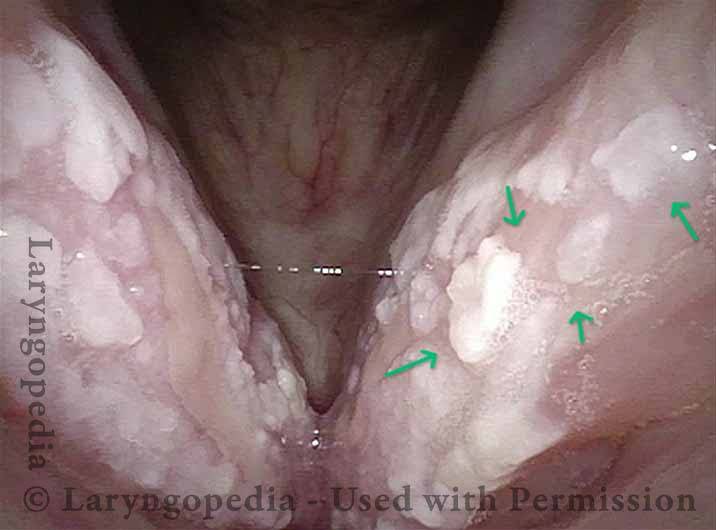
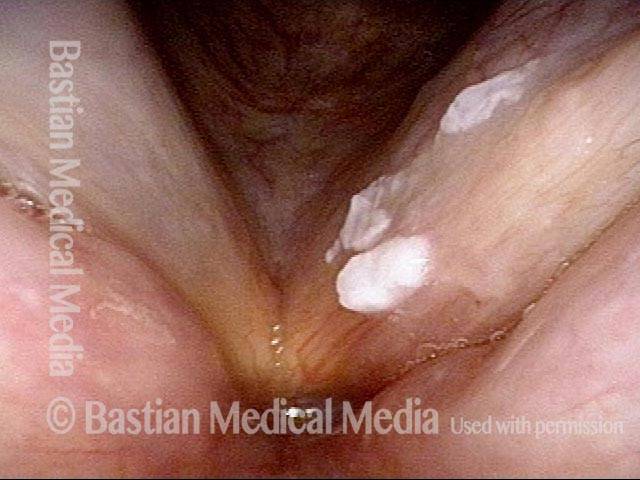
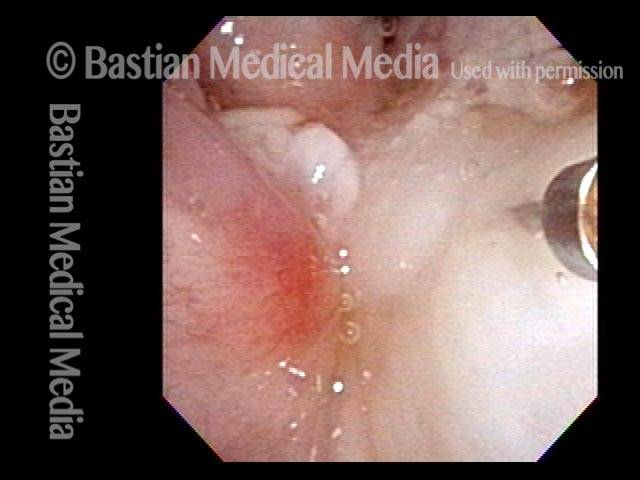
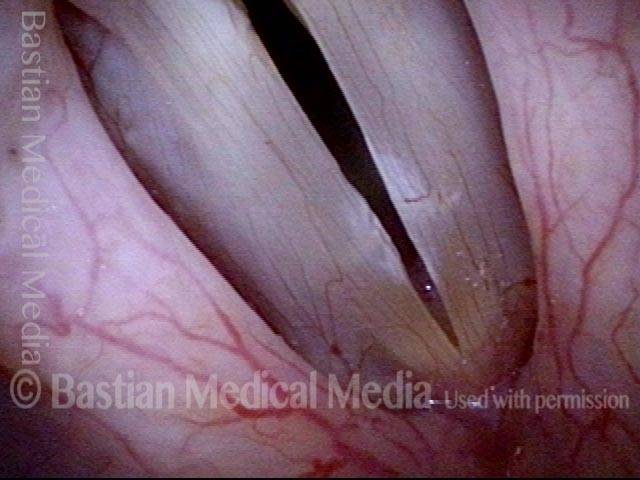
Spilled milk Leukoplakia (2 of 16)
Spilled milk Leukoplakia (2 of 16)
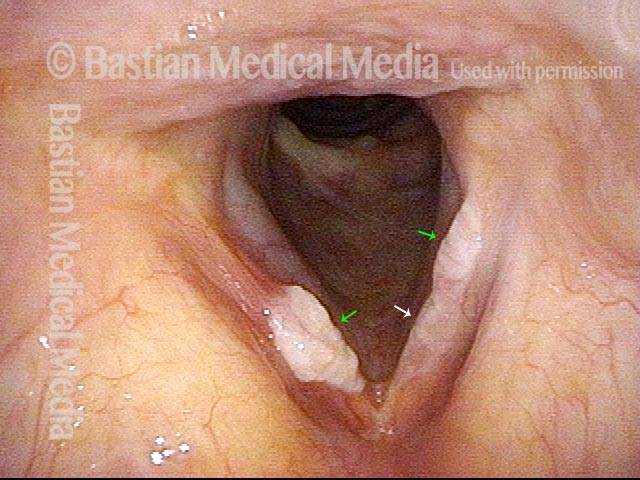
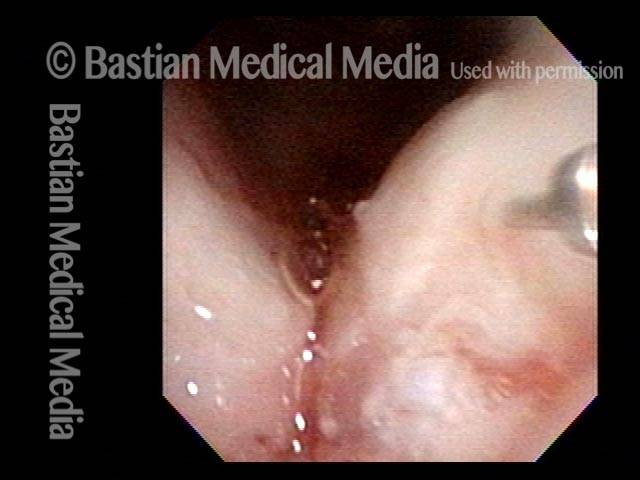
Superficial ulceration (3 of 16)
Superficial ulceration (3 of 16)
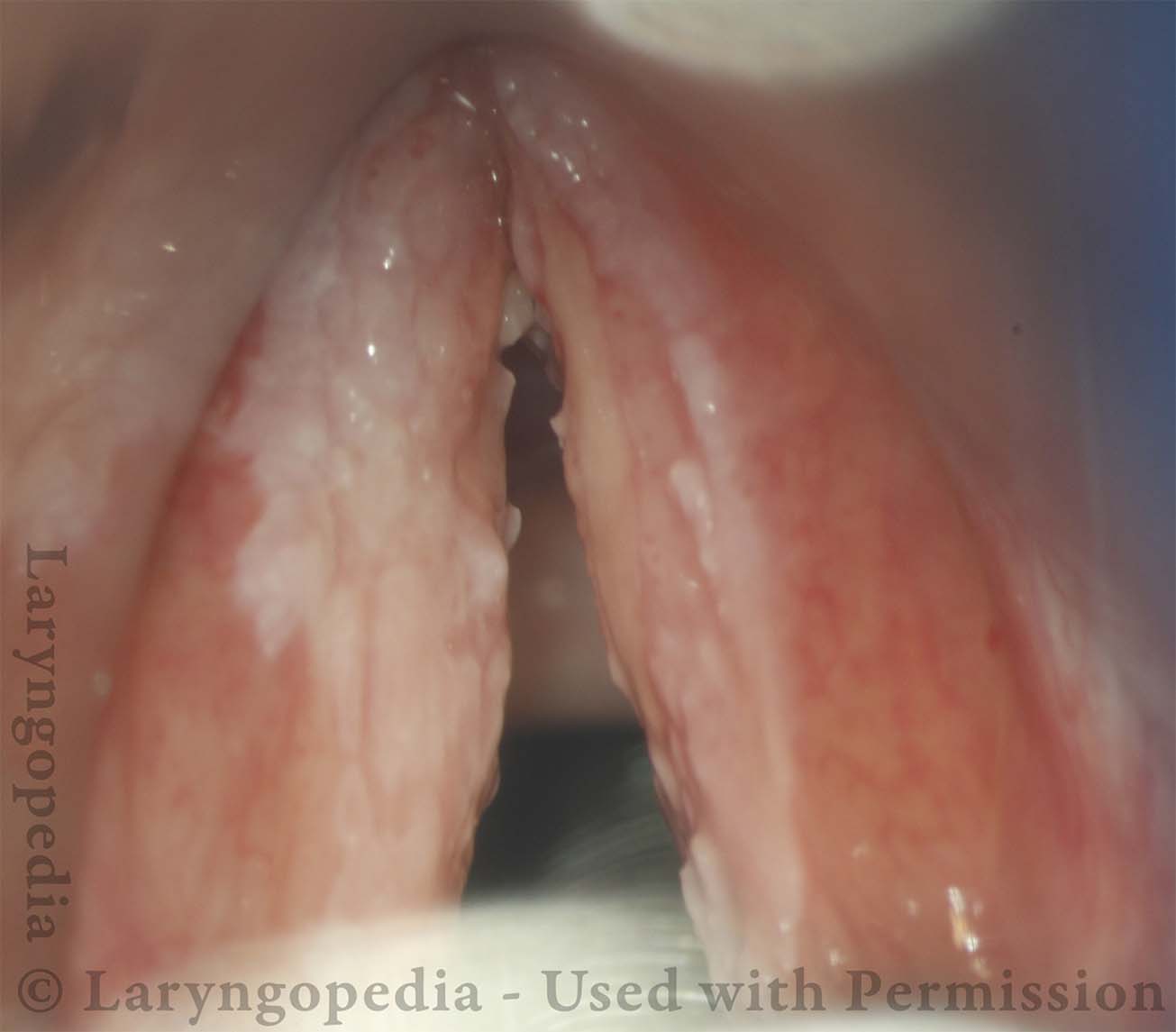
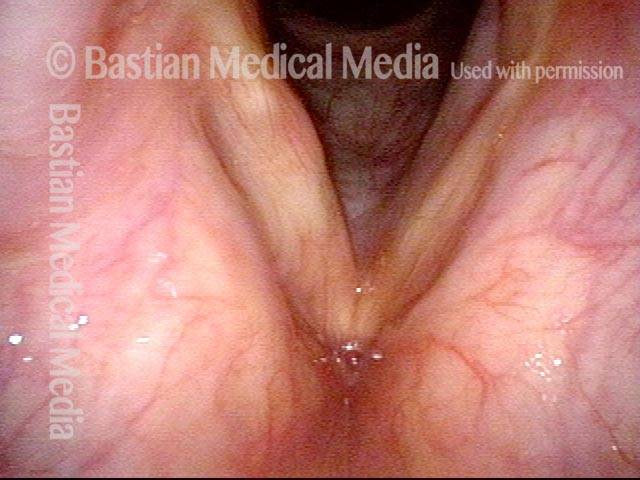
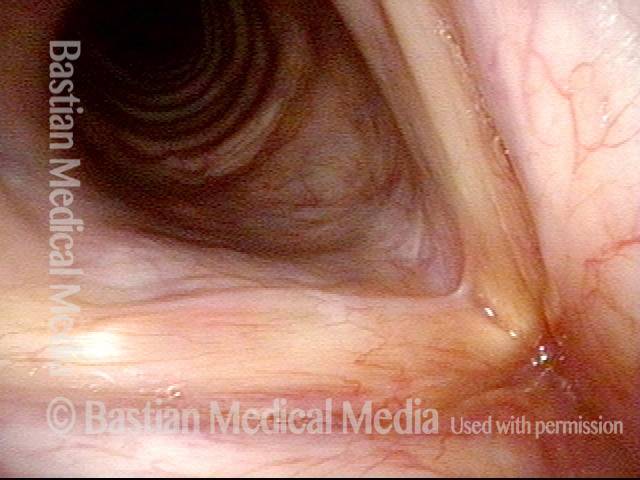
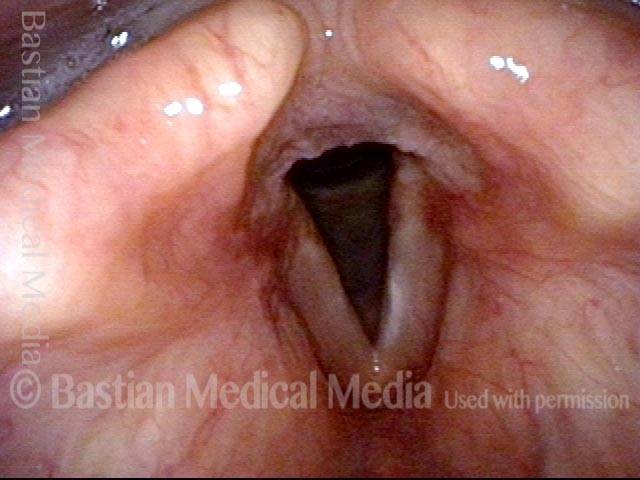
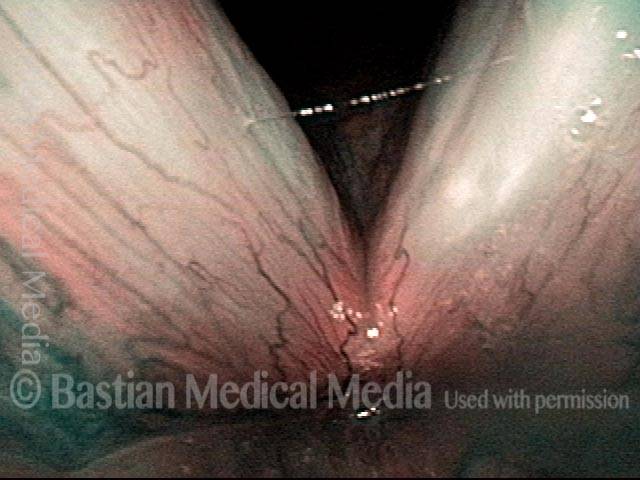
Closed phase of vibration (4 of 16)
Closed phase of vibration (4 of 16)
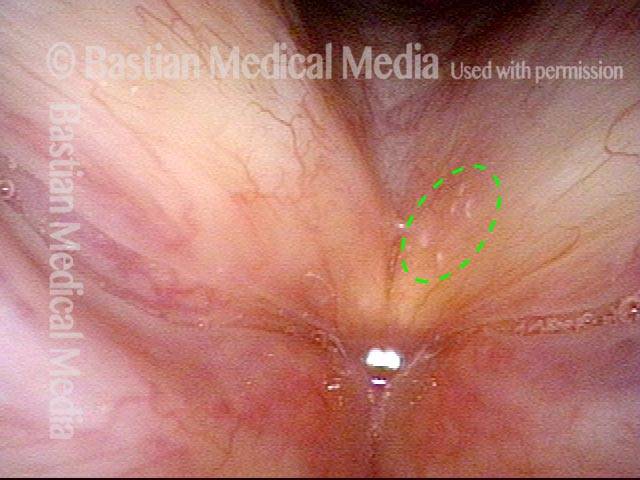
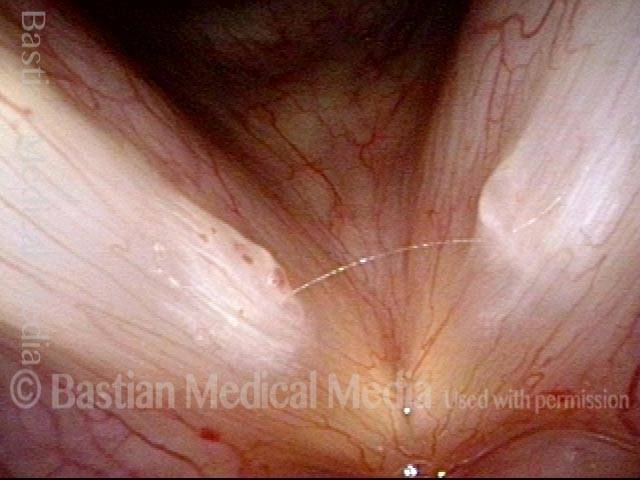
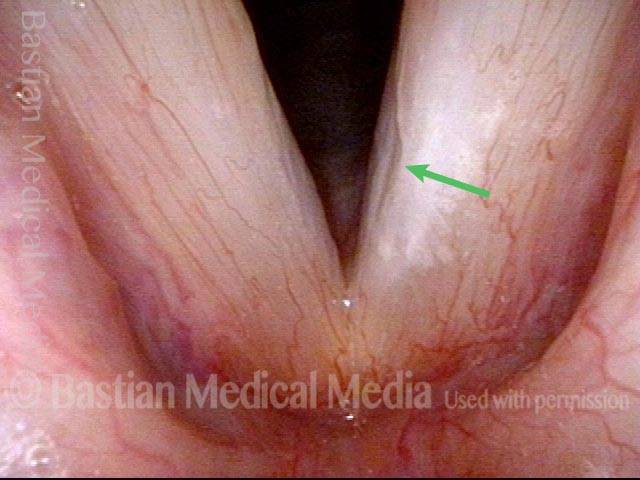
Stiff mucosa limits vibration (5 of 16)
Stiff mucosa limits vibration (5 of 16)
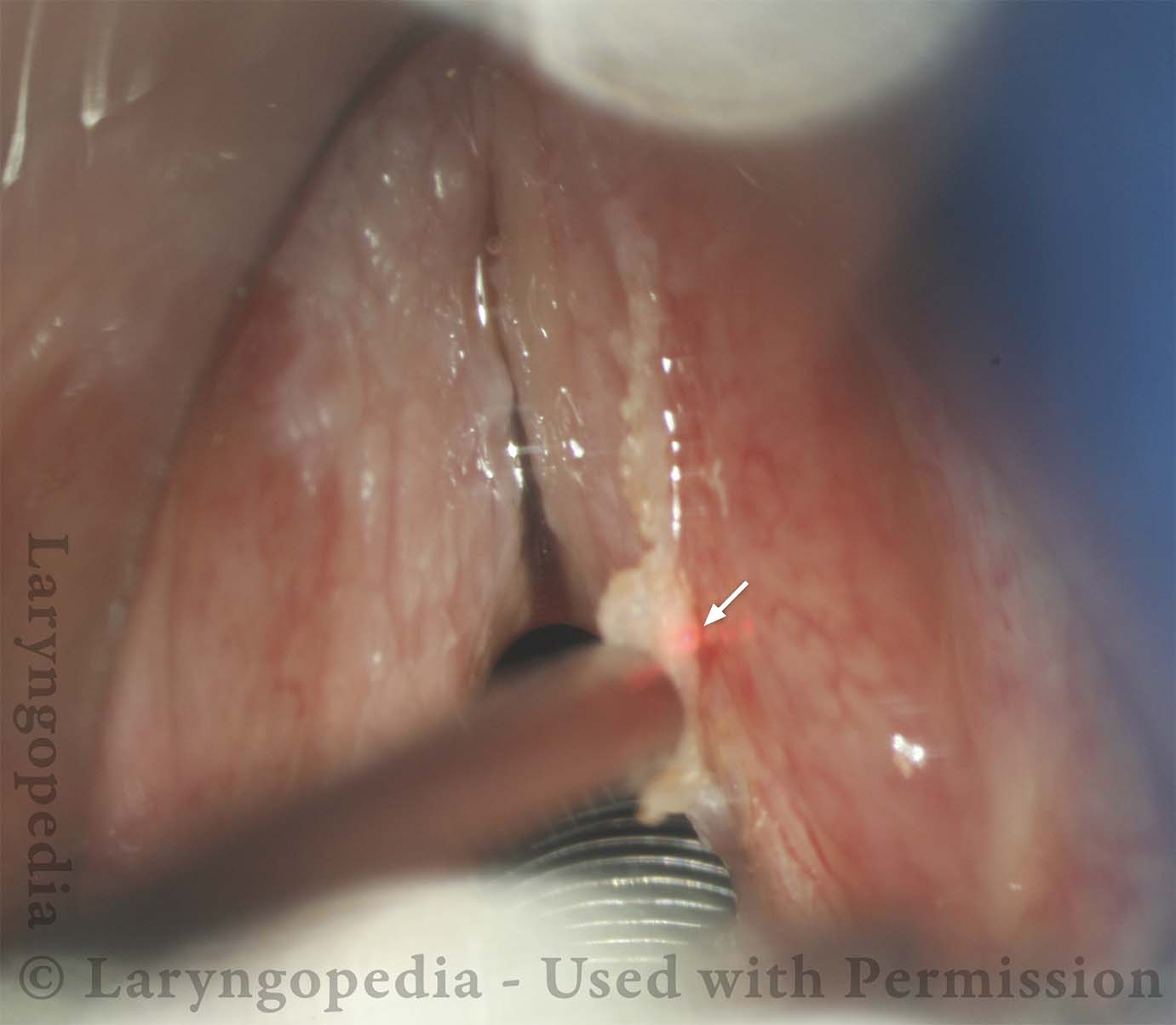
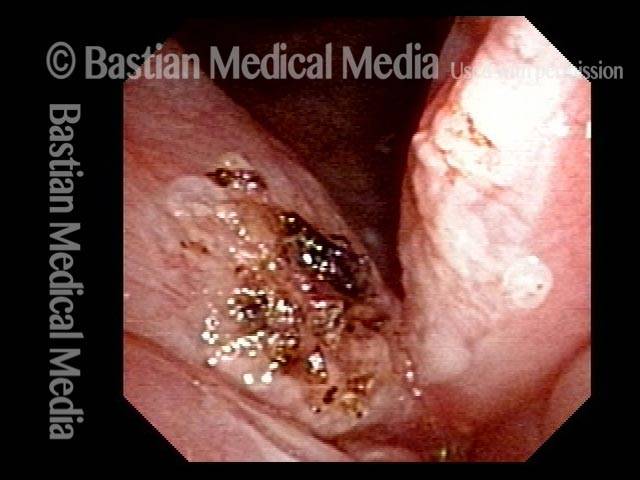
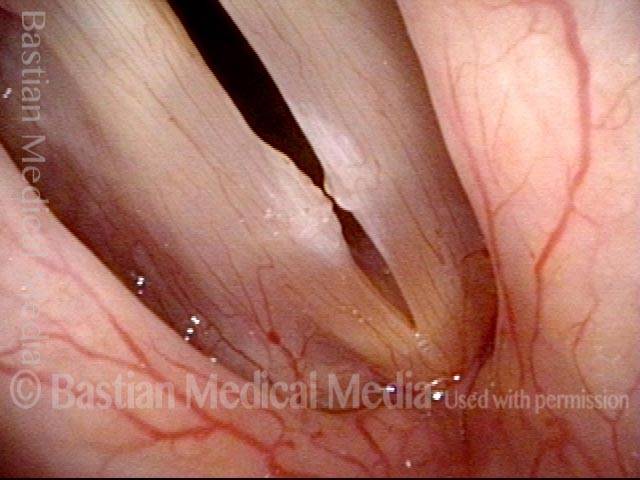
Operative view, first surgical procedure (6 of 16)
Operative view, first surgical procedure (6 of 16)
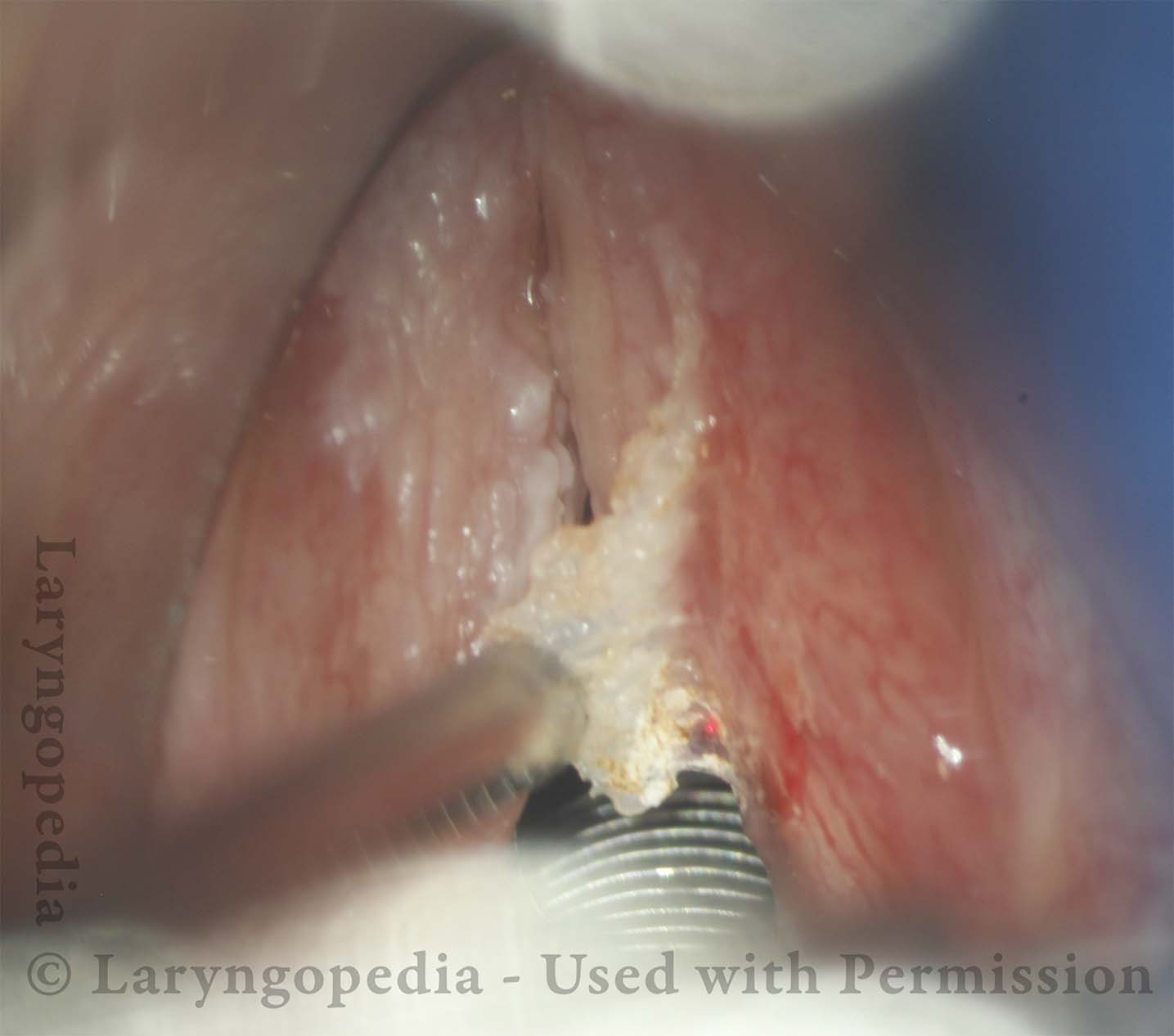
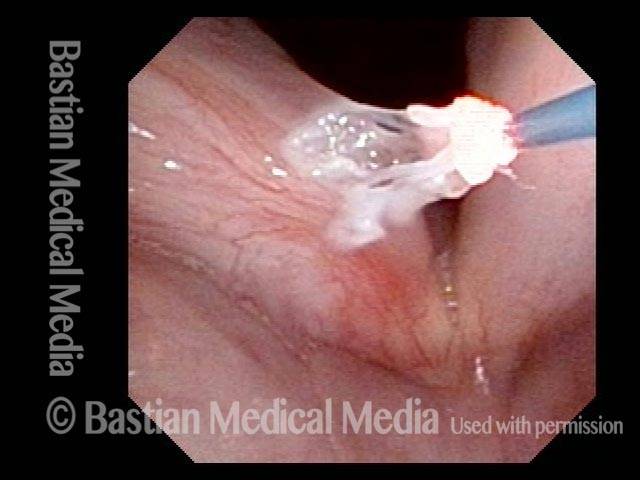
Peeling begins (7 of 16)
Peeling begins (7 of 16)
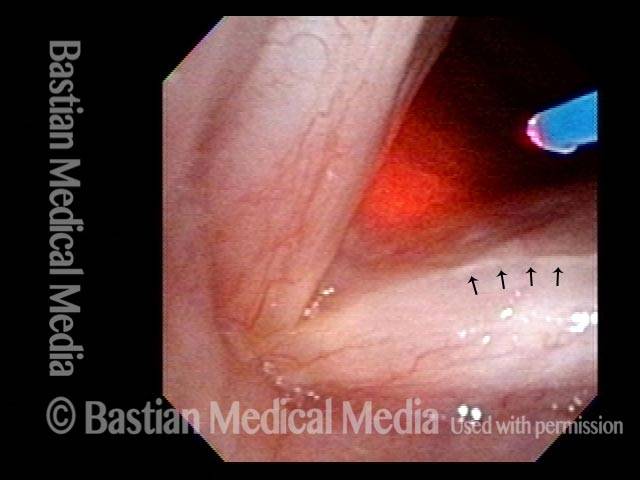
Can be relatively bloodless (8 of 16)
Can be relatively bloodless (8 of 16)
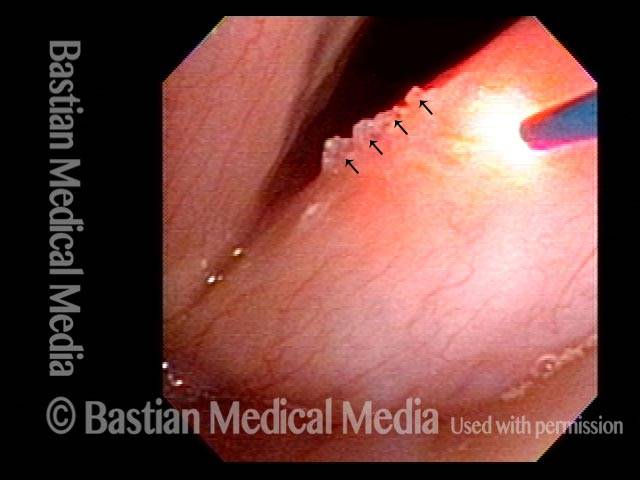
Near complete (9 of 16)
Near complete (9 of 16)
Leukoplakia diminishes (10 of 16)
Leukoplakia diminishes (10 of 16)
Residual leukoplakia (11 of 16)
Residual leukoplakia (11 of 16)
Hazy grey is surgical wound not leukoplakia (12 of 16)
Hazy grey is surgical wound not leukoplakia (12 of 16)
About to win more territory (13 of 16)
About to win more territory (13 of 16)
Second battle (14 of 16)
Second battle (14 of 16)
Winning the war (15 of 16)
Winning the war (15 of 16)
Good vibratory flexibility (16 of 16)
Good vibratory flexibility (16 of 16)
Leukoplakia, Before and After Surgical Removal
Diffuse leukoplakia (1 of 7)
Diffuse leukoplakia (1 of 7)
HPV effect (2 of 7)
HPV effect (2 of 7)
Surgical view (3 of 7)
Surgical view (3 of 7)
Basement membrane peeling (4 of 7)
Basement membrane peeling (4 of 7)
Removal complete (5 of 7)
Removal complete (5 of 7)
Two years post-op (6 of 7)
Two years post-op (6 of 7)
Mucosa is flexible (7 of 7)
Mucosa is flexible (7 of 7)
Photo Examples of Leukoplakia
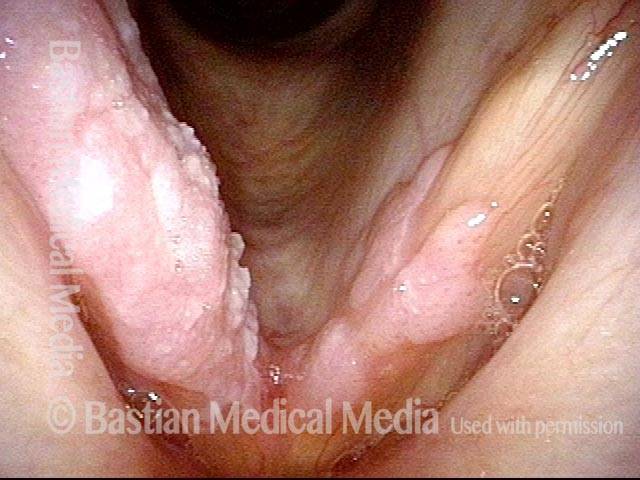
Cake-icing Leukoplakia (1 of 4)
Cake-icing Leukoplakia (1 of 4)
Hazy Leukoplakia (2 of 4)
Hazy Leukoplakia (2 of 4)
Leukoplakia (3 of 4)
Leukoplakia (3 of 4)
Closer look (4 of 4)
Closer look (4 of 4)
Example 2
Leukoplakia (1 of 2)
Leukoplakia (1 of 2)
Leukoplakia (2 of 2)
Leukoplakia (2 of 2)
Leukoplakia Battled Over Time
Leukoplakia (1 of 8)
Leukoplakia (1 of 8)
Spilled Milk (2 of 8)
Spilled Milk (2 of 8)
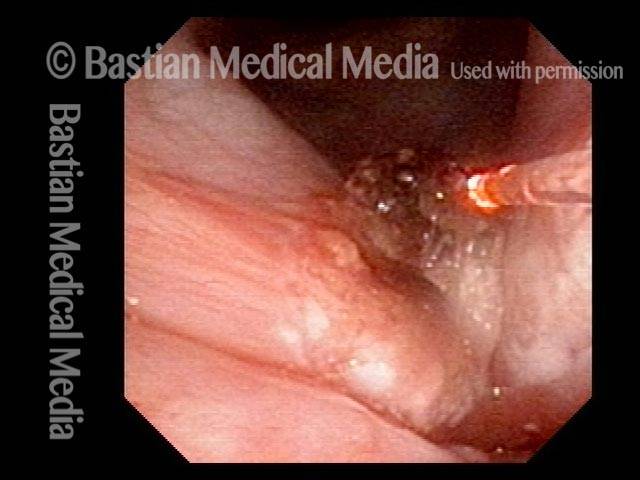
Thulium laser (3 of 8)
Thulium laser (3 of 8)
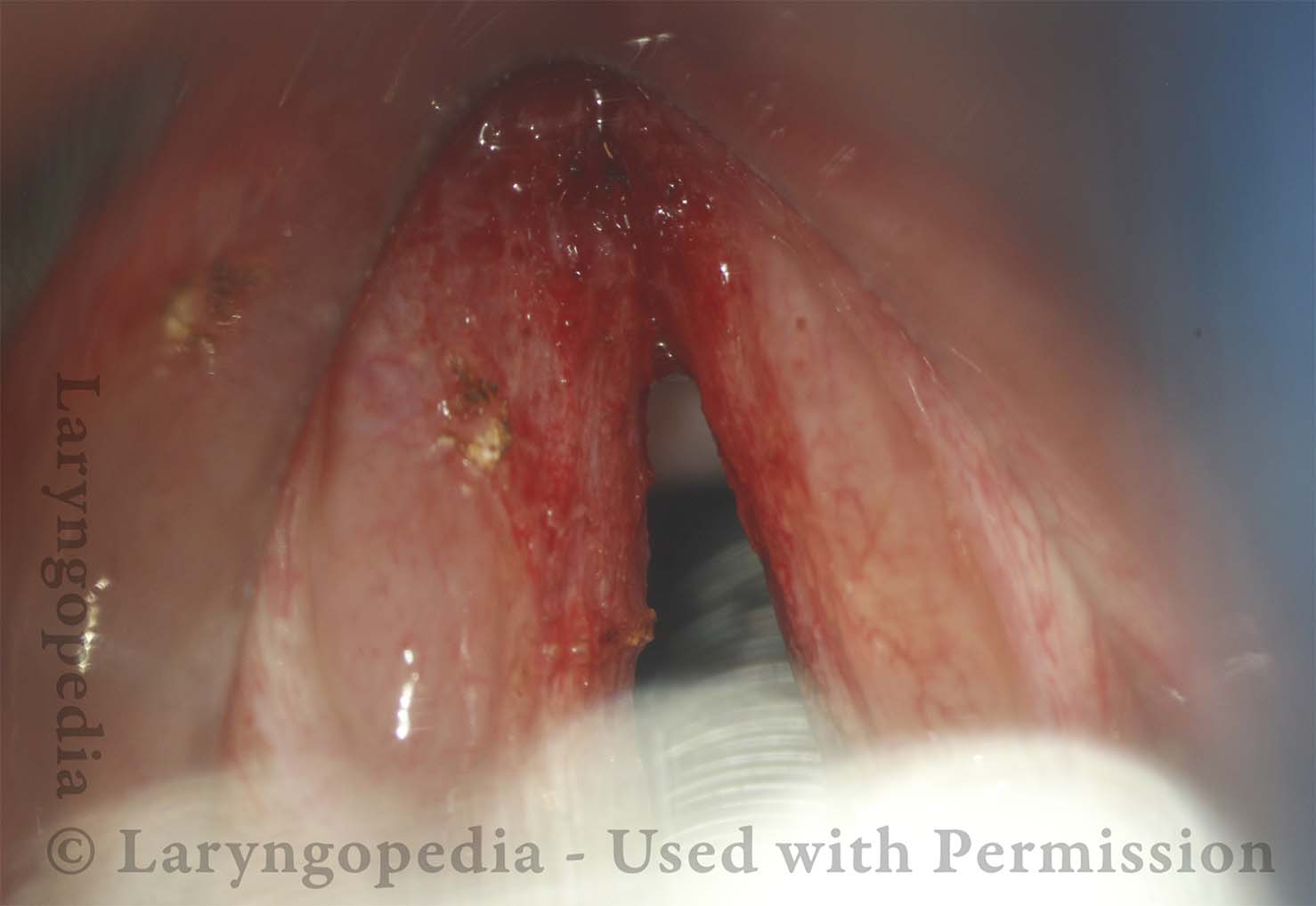
Coagulated tissue (4 of 8)
Coagulated tissue (4 of 8)
Leukoplakia (5 of 8)
Leukoplakia (5 of 8)
Detachment (6 of 8)
Detachment (6 of 8)
Superficial vascular pattern (7 of 8)
Superficial vascular pattern (7 of 8)
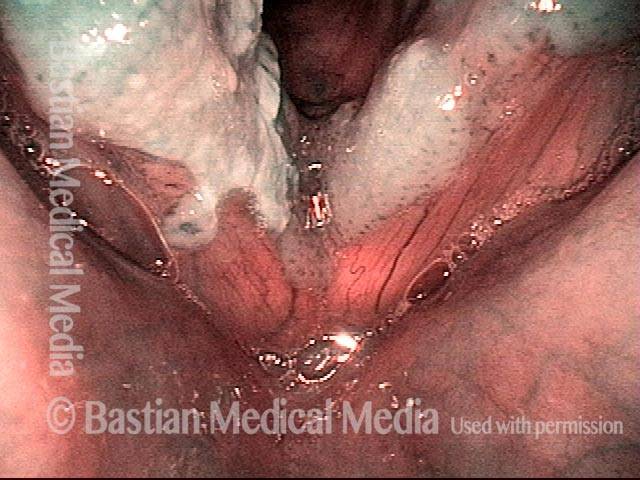
Coagulated tissue (8 of 8)
Coagulated tissue (8 of 8)
Thulium Laser Surgery, With Local Anesthetic Injection, to Treat Leukoplakia
Leukoplakia, about to be treated with laser (1 of 4)
Leukoplakia, about to be treated with laser (1 of 4)
Injection of local anesthetic (2 of 4)
Injection of local anesthetic (2 of 4)
Injection of local anesthetic (3 of 4)
Injection of local anesthetic (3 of 4)
Right after thulium laser treatment (4 of 4)
Right after thulium laser treatment (4 of 4)
Leukoplakia, Before, During, and After Laser Coagulation
Leukoplakia, not yet seen (1 of 6)
Leukoplakia, not yet seen (1 of 6)
Leukoplakia (2 of 6)
Leukoplakia (2 of 6)
Leukoplakia (3 of 6)
Leukoplakia (3 of 6)
Leukoplakia, coagulated by laser (4 of 6)
Leukoplakia, coagulated by laser (4 of 6)
Leukoplakia, 3 months after laser treatment (5 of 6)
Leukoplakia, 3 months after laser treatment (5 of 6)
Leukoplakia, 3 months after laser treatment (6 of 6)
Leukoplakia, 3 months after laser treatment (6 of 6)
Vocal Nodules, Leukoplakia, and Capillary Ectasia
Vocal nodules, leukoplakia, and capillary ectasia (1 of 4)
Vocal nodules, leukoplakia, and capillary ectasia (1 of 4)
Vocal nodules, leukoplakia, and capillary ectasia (2 of 4)
Vocal nodules, leukoplakia, and capillary ectasia (2 of 4)
Vocal nodules, leukoplakia, and capillary ectasia: 6 months later (3 of 4)
Vocal nodules, leukoplakia, and capillary ectasia: 6 months later (3 of 4)
Vocal nodules, leukoplakia, and capillary ectasia: 6 months later (4 of 4)
Vocal nodules, leukoplakia, and capillary ectasia: 6 months later (4 of 4)
Glottic Furrow / Leukoplakia / Acid Reflux
Glottic furrow / Leukoplakia / Acid reflux (1 of 4)
Glottic furrow / Leukoplakia / Acid reflux (1 of 4)
Leukoplakia (2 of 4)
Leukoplakia (2 of 4)
Glottic furrows (3 of 4)
Glottic furrows (3 of 4)
Gap during closed phase (4 of 4)
Gap during closed phase (4 of 4)
Leukoplakia Biopsy
HIV Testing (1 of 2)
HIV Testing (1 of 2)
Biopsy (2 of 2)
Biopsy (2 of 2)
Narrow-band vs. Standard Light: Leukoplakia
Narrow-band vs. standard light: leukoplakia (1 of 2)
Narrow-band vs. standard light: leukoplakia (1 of 2)
Narrow-band vs. standard light: leukoplakia (2 of 2)
Narrow-band vs. standard light: leukoplakia (2 of 2)
Share this article