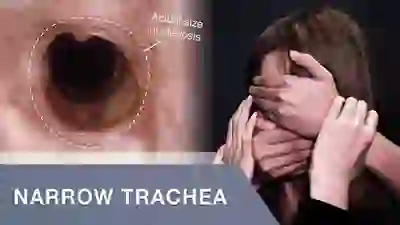
Stenosis
Stenosis is the abnormal narrowing of a passageway in the body. At our practice, it typically refers to narrowing in the breathing passage, such as for narrowing in the glottic, subglottic, or tracheal areas.
Stenosis in the airway can be the result of prolonged endotracheal intubation, external trauma such as gunshot wound, crush injury, or tracheotomy, an inflammatory or auto-immune process, surgical resection of part of the airway for tumor, or other causes.
Symptoms
Persons with airway stenosis will note a reduced capacity for exercise. Often the clinician hears noisy breathing on inhalation, especially when the patient is asked to fill the lungs quickly. Esophageal stenosis gives symptoms of difficulty swallowing solids more so than liquids.
Types of stenosis: Idiopathic Subglottic Stenosis, Subglottic Stenosis, Hypopharyngeal Stenosis, Glottic Stenosis, Esophageal Stenosis
Tracheal Stenosis
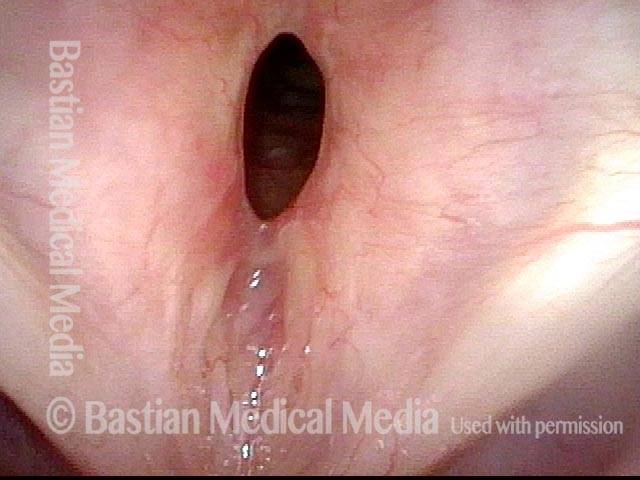
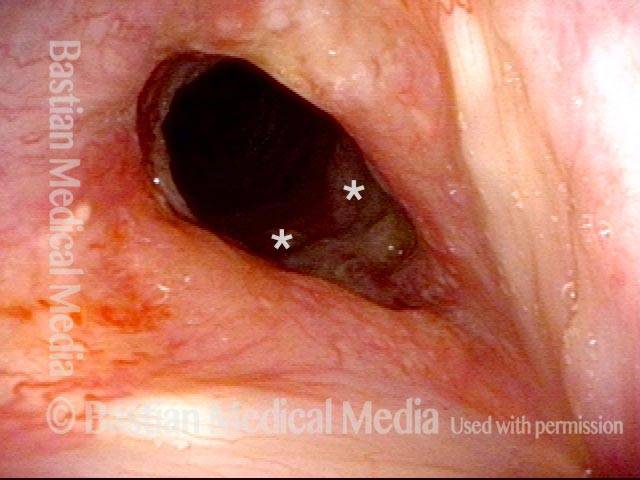
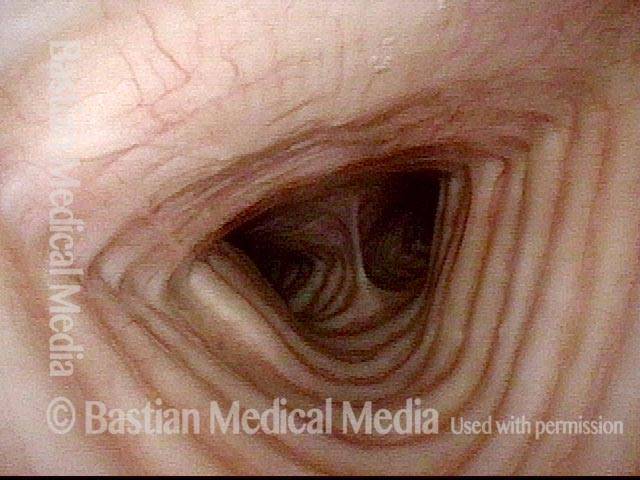
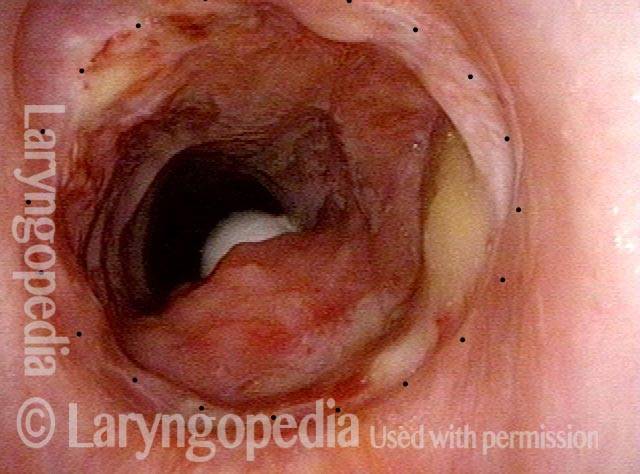
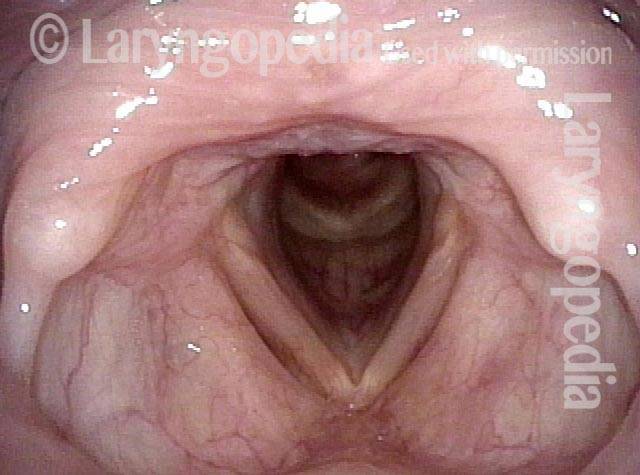
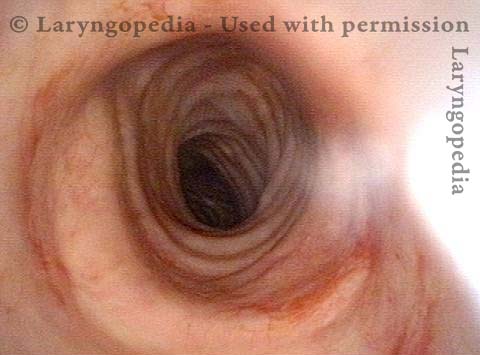
Tracheal stenosis (1 of 4)
Tracheal stenosis (1 of 4)
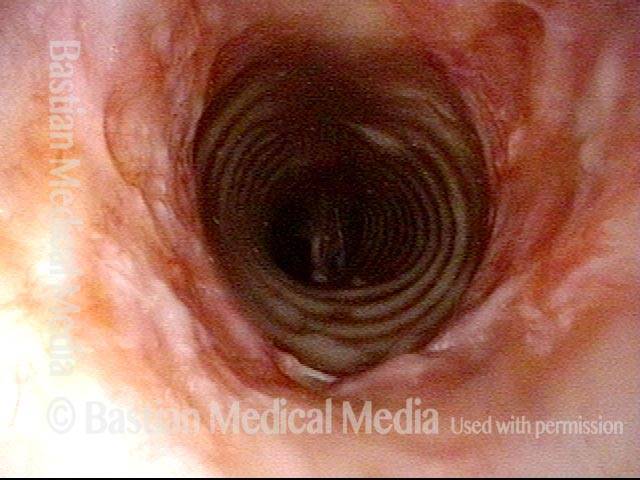
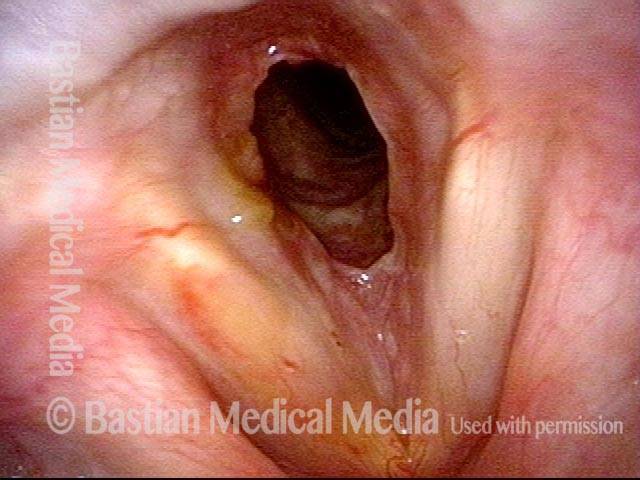
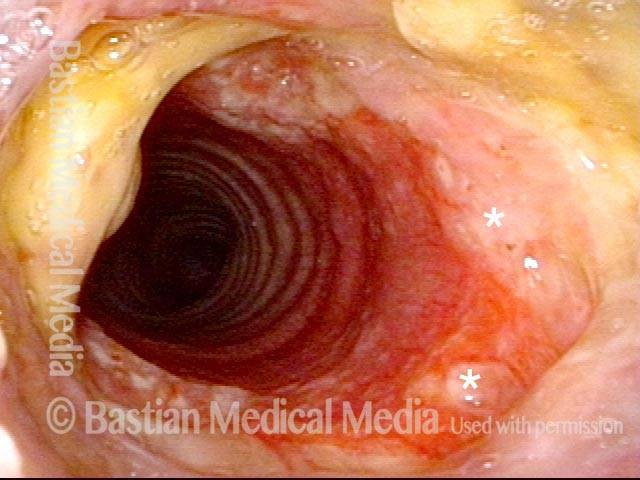
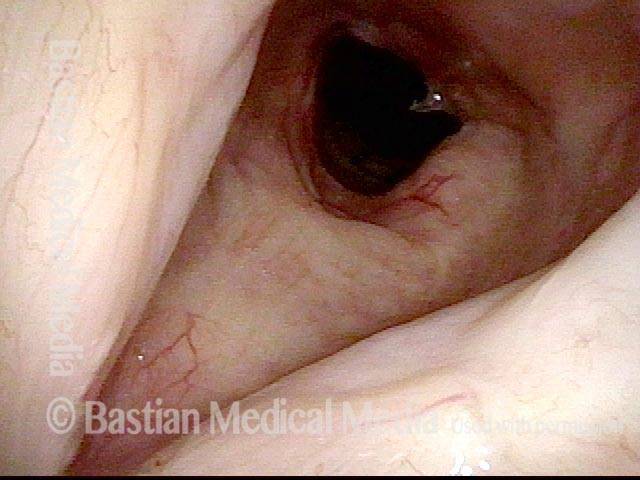
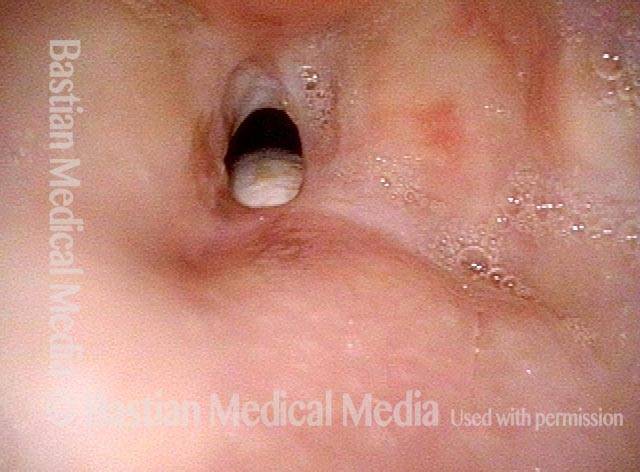
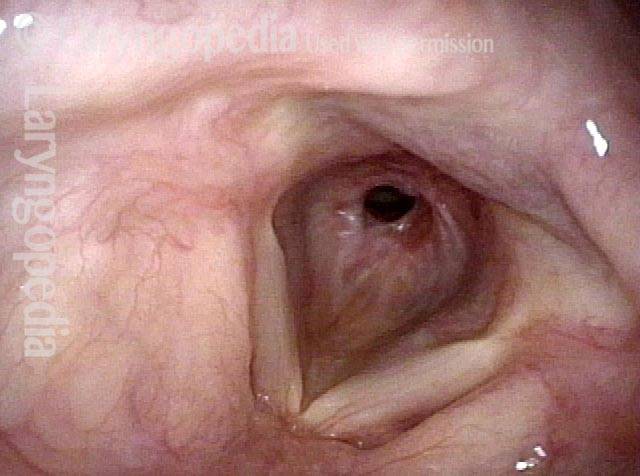
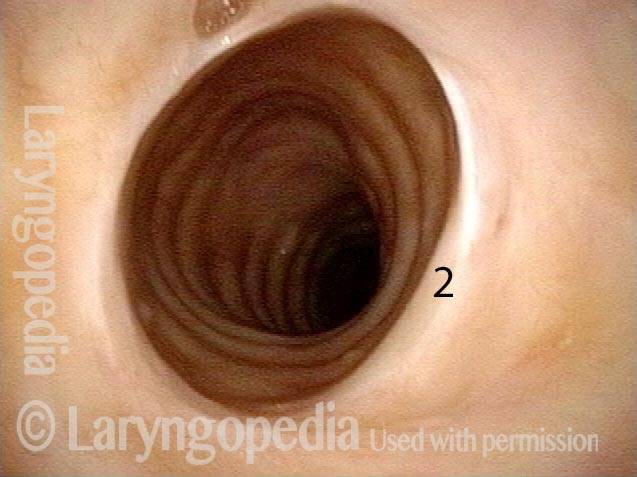
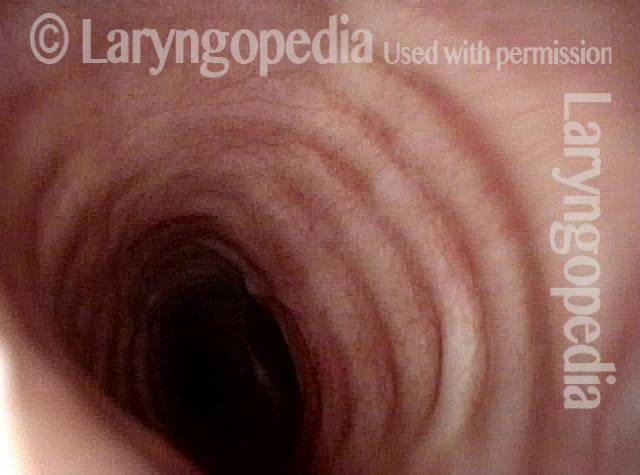
Tracheal stenosis (2 of 4)
Tracheal stenosis (2 of 4)
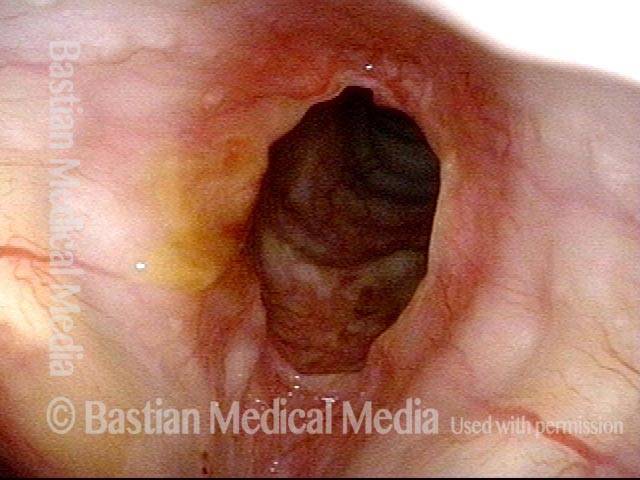
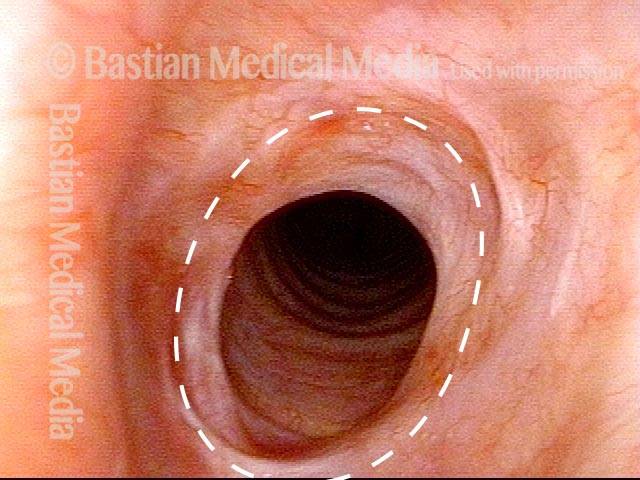
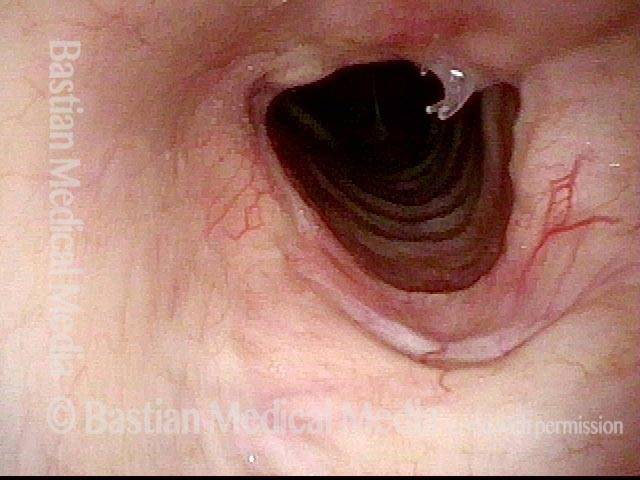
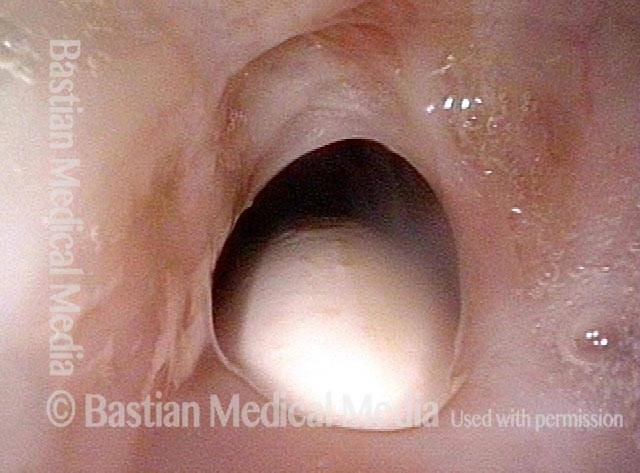
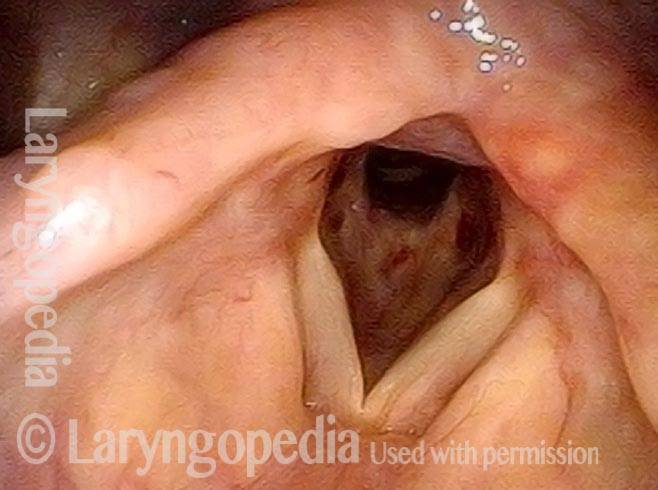
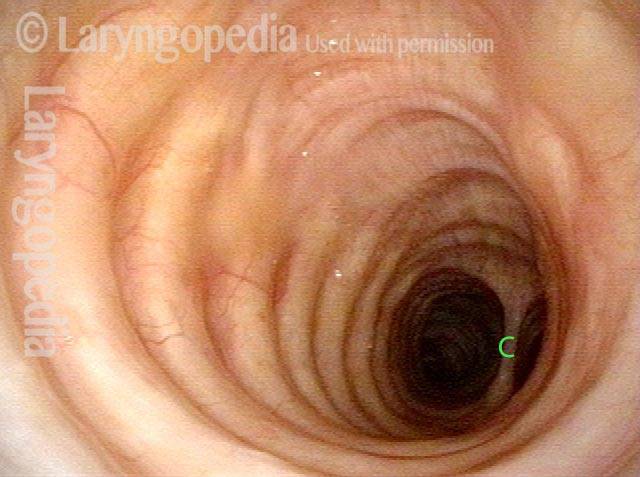
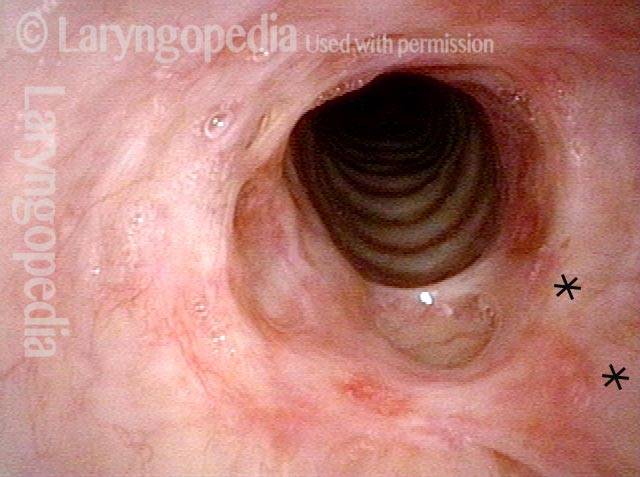
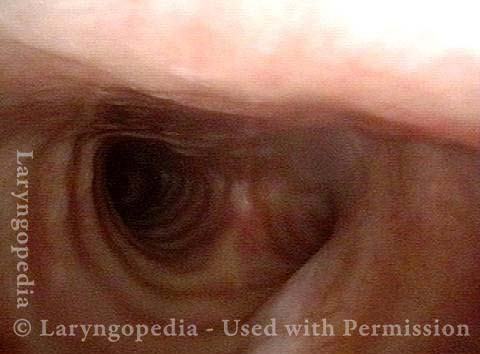
Tracheal stenosis (3 of 4)
Tracheal stenosis (3 of 4)
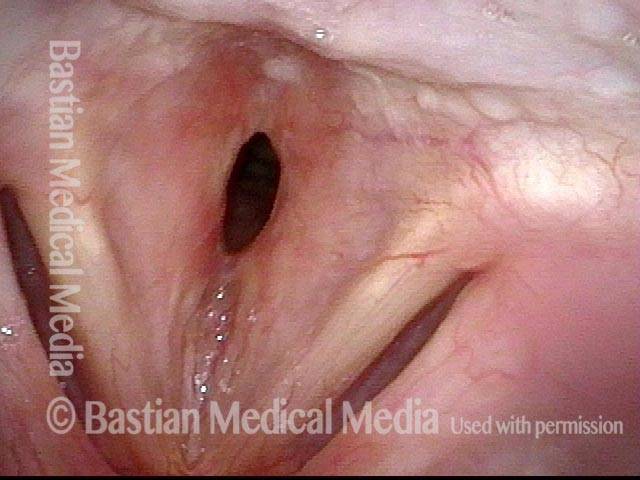
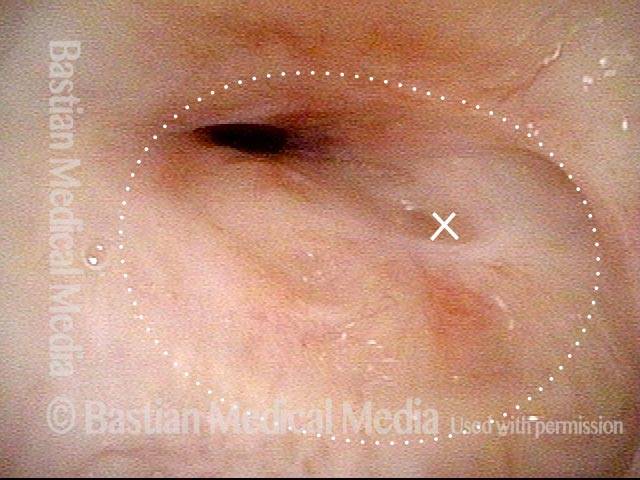
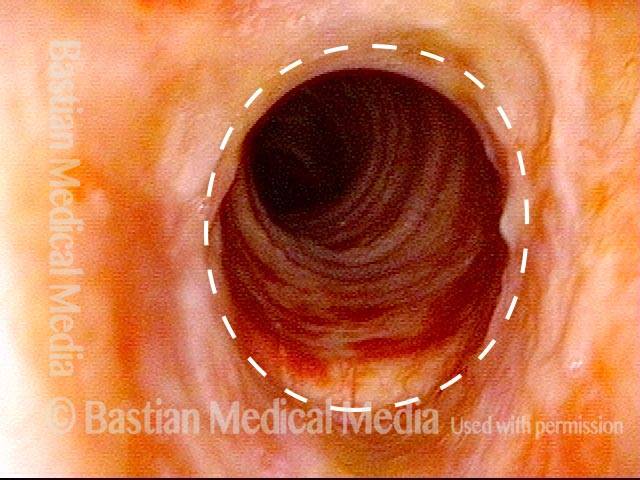
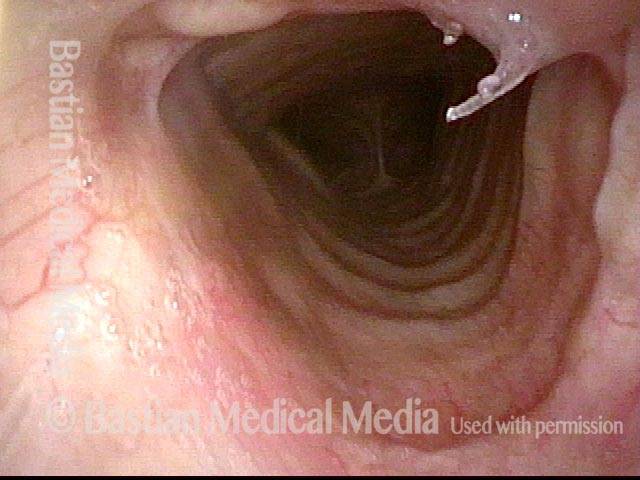
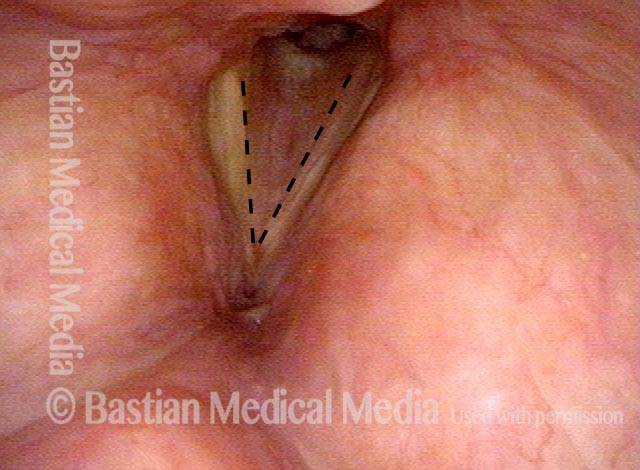
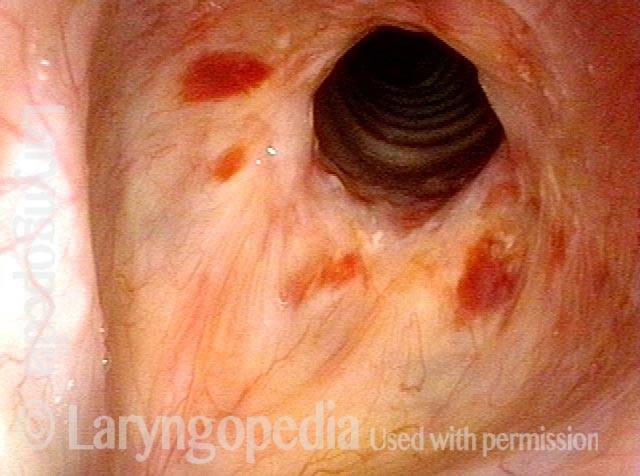
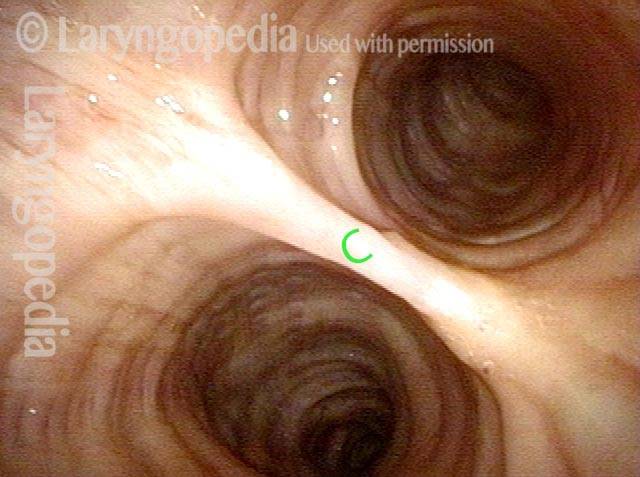
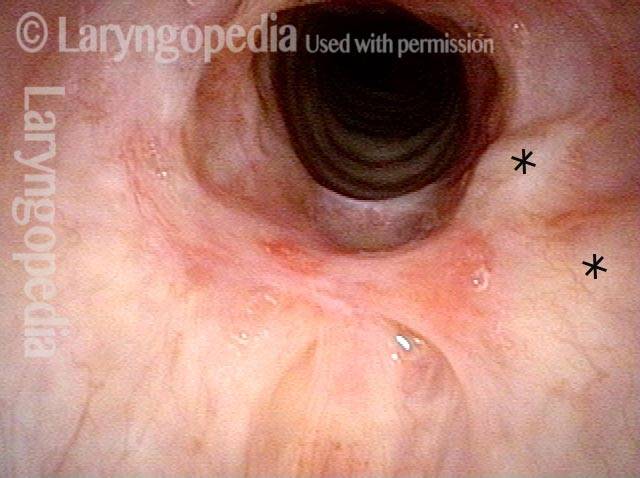
Just below the tracheal stenosis (4 of 4)
Just below the tracheal stenosis (4 of 4)
Example 2
Tracheal stenosis (1 of 3)
Tracheal stenosis (1 of 3)
Tracheal stenosis (2 of 3)
Tracheal stenosis (2 of 3)
Just below the tracheal stenosis (3 of 3)
Just below the tracheal stenosis (3 of 3)
Example 3
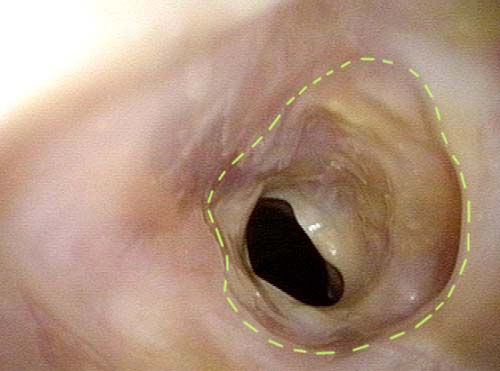
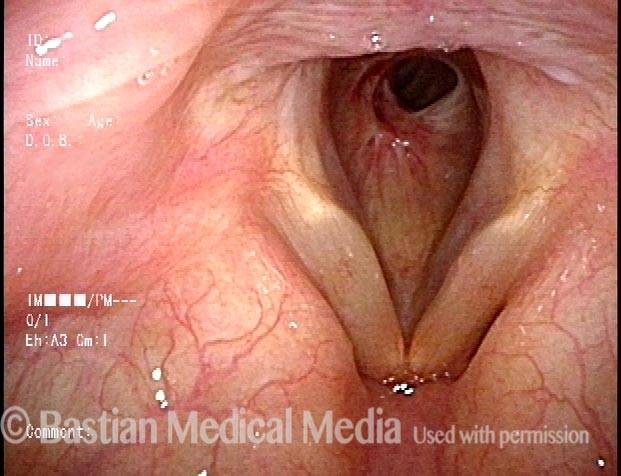
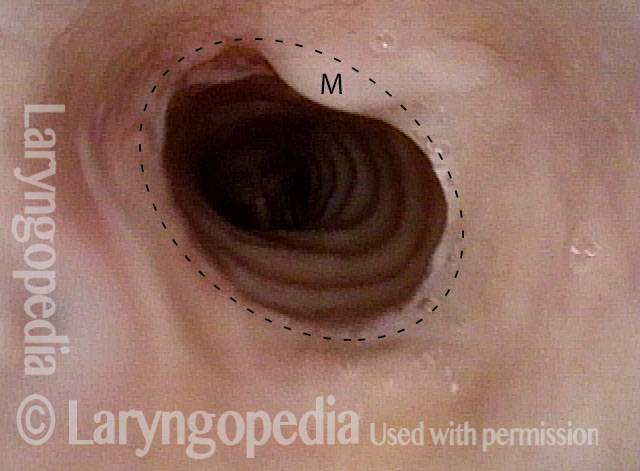
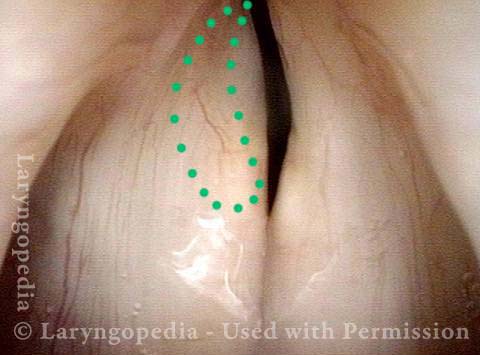
Narrowing in the Trachea > 50% (1 of 2)
Narrowing in the Trachea > 50% (1 of 2)
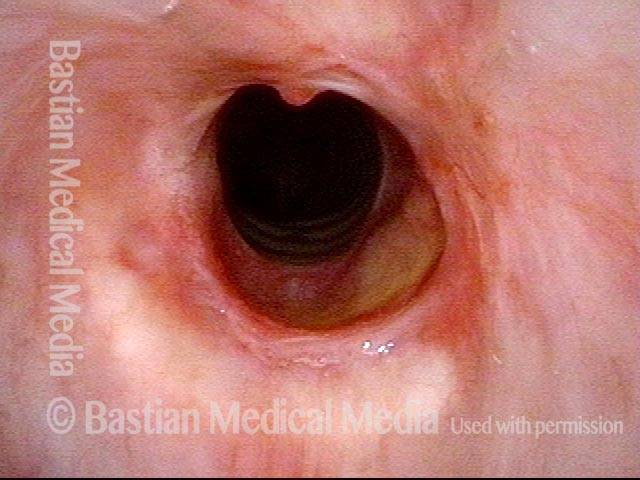
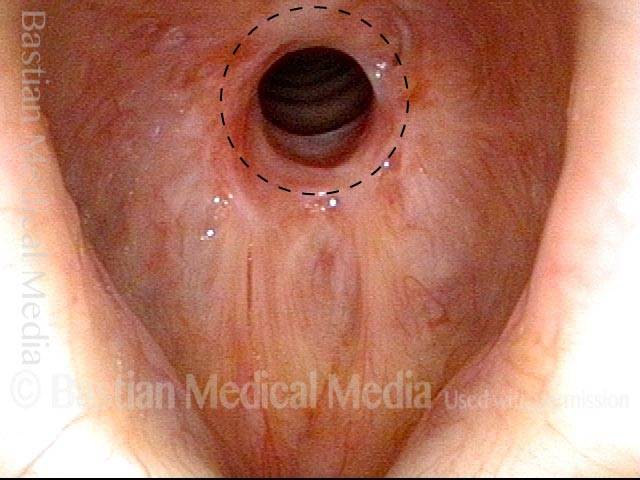
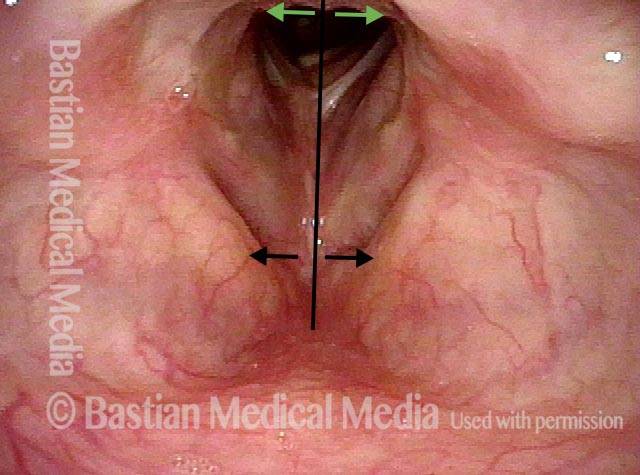
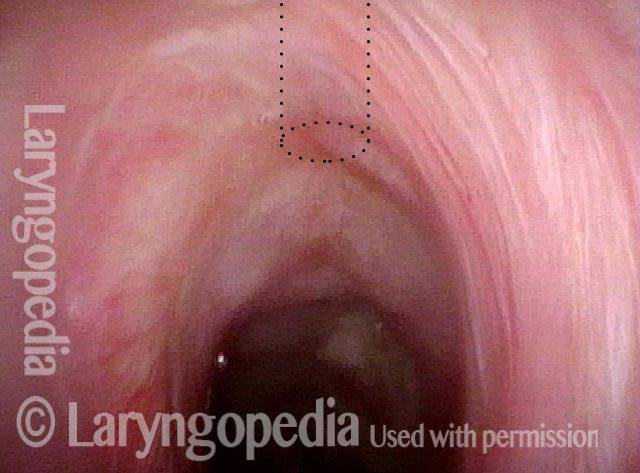
Expected Size of Tracheal Opening (2 of 2)
Expected Size of Tracheal Opening (2 of 2)
Subglottic Stenosis, before and after Dilation
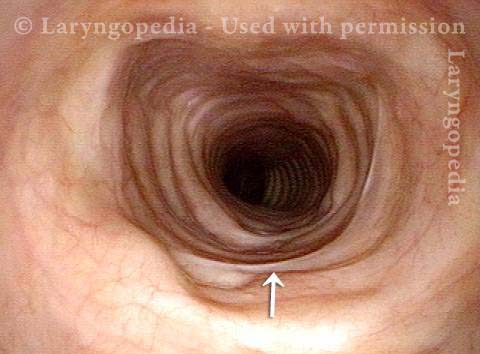
Subglottic stenosis, before dilation (1 of 2)
Subglottic stenosis, before dilation (1 of 2)
Subglottic stenosis, after dilation (2 of 2)
Subglottic stenosis, after dilation (2 of 2)
Example 2
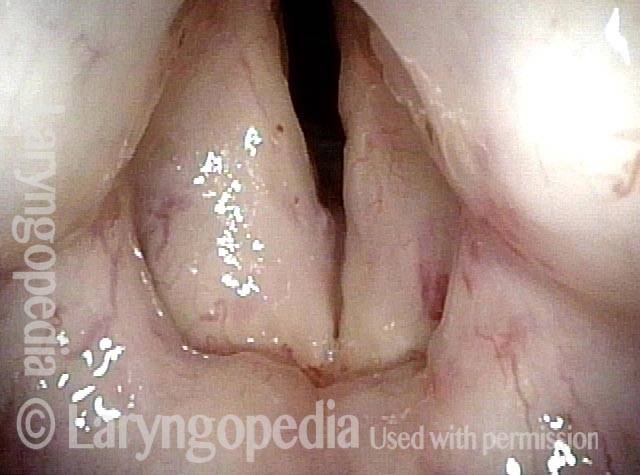
Subglottic stenosis (1 of 5)
Subglottic stenosis (1 of 5)
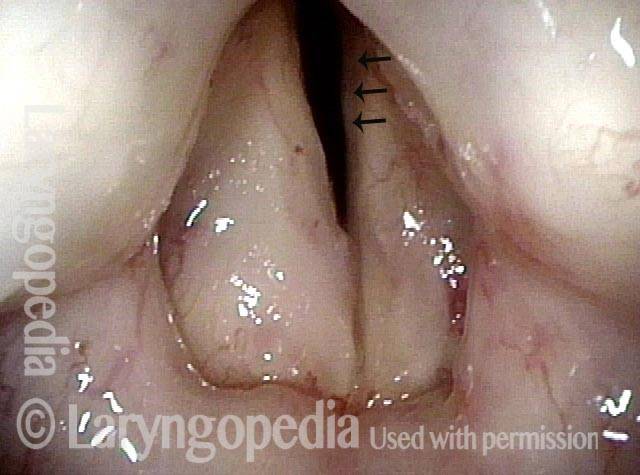
Subglottic stenosis, worsened (2 of 5)
Subglottic stenosis, worsened (2 of 5)
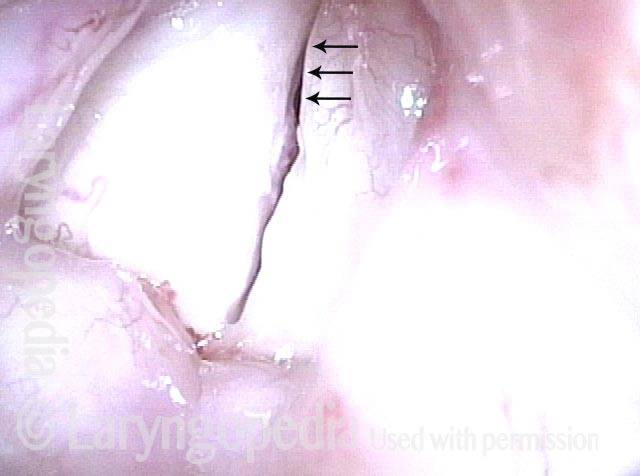
Subglottic stenosis, worsened (3 of 5)
Subglottic stenosis, worsened (3 of 5)
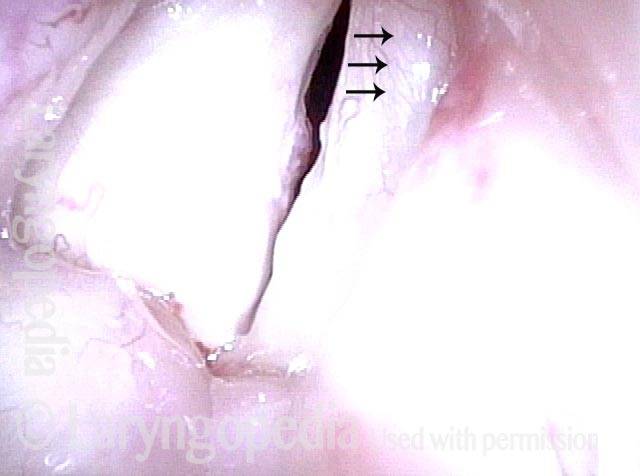
Subglottic stenosis, after dilation (4 of 5)
Subglottic stenosis, after dilation (4 of 5)
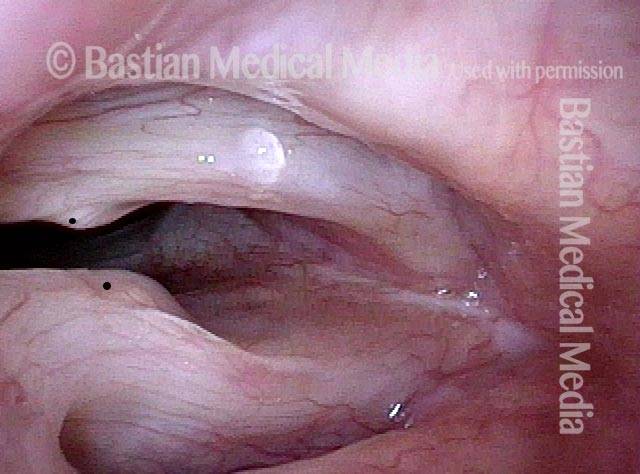
Subglottic stenosis, after dilation (5 of 5)
Subglottic stenosis, after dilation (5 of 5)
Tracheal Stenosis and Collapse
Tracheal stenosis and collapse (1 of 2)
Tracheal stenosis and collapse (1 of 2)
Tracheal stenosis and collapse (2 of 2)
Tracheal stenosis and collapse (2 of 2)
Tracheal Stenosis, Due to Forme Fruste Wegener’s Granulomatosis
Tracheal stenosis (1 of 3)
Tracheal stenosis (1 of 3)
Tracheal stenosis (2 of 3)
Tracheal stenosis (2 of 3)
Just below the tracheal stenosis (3 of 3)
Just below the tracheal stenosis (3 of 3)
Subglottic / Tracheal Stenosis
Wegener’s granulomatosis (1 of 4)
Wegener’s granulomatosis (1 of 4)
Subglottic / Tracheal stenosis (2 of 4)
Subglottic / Tracheal stenosis (2 of 4)
Subglottic / Tracheal stenosis (3 of 4)
Subglottic / Tracheal stenosis (3 of 4)
Inflammed Stenosis (4 of 4)
Inflammed Stenosis (4 of 4)
Hypopharyngeal Stenosis
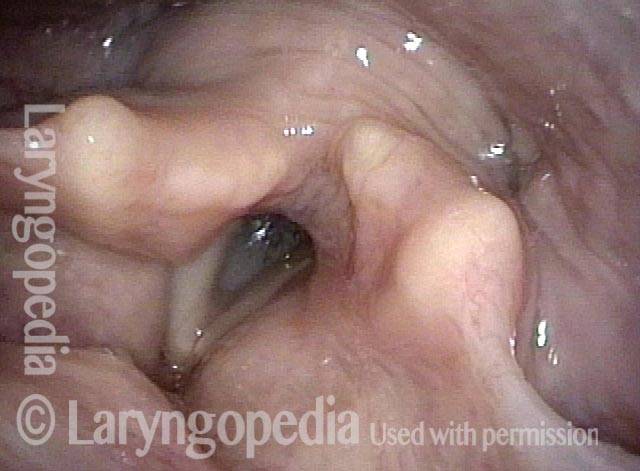
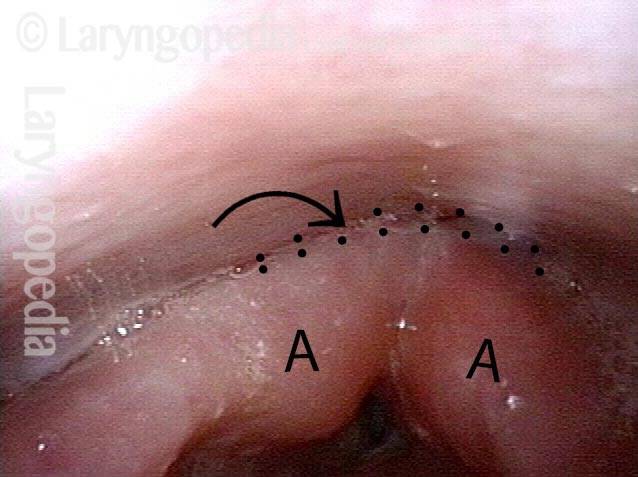
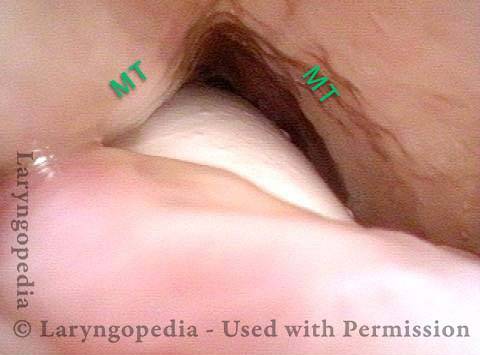
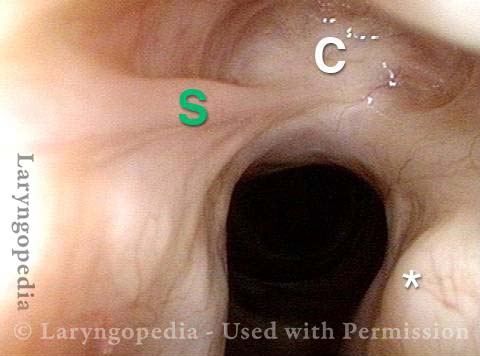
Hypopharyngeal stenosis: not yet visible (1 of 2)
Hypopharyngeal stenosis: not yet visible (1 of 2)
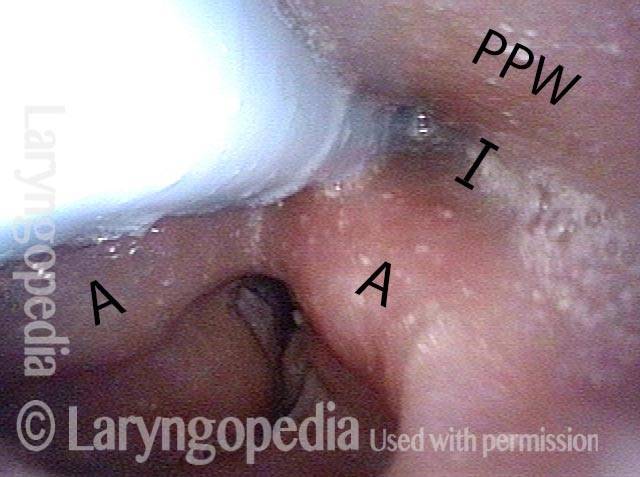
Hypopharyngeal stenosis: revealed (2 of 2)
Hypopharyngeal stenosis: revealed (2 of 2)
Subglottic Stenosis, Due to Wegener’s Granulomatosis
Subglottic stenosis, due to Wegener’s (1 of 2)
Subglottic stenosis, due to Wegener’s (1 of 2)
Subglottic stenosis, due to Wegener’s (2 of 2)
Subglottic stenosis, due to Wegener’s (2 of 2)
Airway Stenosis Caused By Wegener’s Granulomatosis, Before and After Dilations
Airway stenosis (1 of 5)
Airway stenosis (1 of 5)
Airway stenosis, after dilation (2 of 5)
Airway stenosis, after dilation (2 of 5)
Airway stenosis, after dilation (3 of 5)
Airway stenosis, after dilation (3 of 5)
Airway stenosis, before another dilation (4 of 5)
Airway stenosis, before another dilation (4 of 5)
Airway stenosis, after another dilation (5 of 5)
Airway stenosis, after another dilation (5 of 5)
Tracheal Stenosis, before and after Tracheal Resection and Primary Reanastomosis
Tracheal stenosis (1 of 8)
Tracheal stenosis (1 of 8)
Tracheal stenosis (2 of 8)
Tracheal stenosis (2 of 8)
Close up view (3 of 8)
Close up view (3 of 8)
Just below the tracheal stenosis (4 of 8)
Just below the tracheal stenosis (4 of 8)
Tracheal stenosis, 5 days after surgery (5 of 8)
Tracheal stenosis, 5 days after surgery (5 of 8)
Tracheal stenosis, 5 days after surgery (6 of 8)
Tracheal stenosis, 5 days after surgery (6 of 8)
Tracheal stenosis, 2 months after surgery (7 of 8)
Tracheal stenosis, 2 months after surgery (7 of 8)
Tracheal stenosis, 2 months after surgery (8 of 8)
Tracheal stenosis, 2 months after surgery (8 of 8)
Dilation for Post-Radiation Hypopharyngeal Stenosis
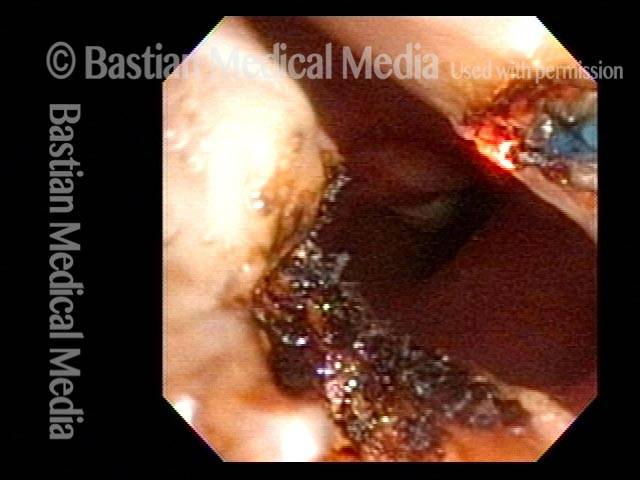
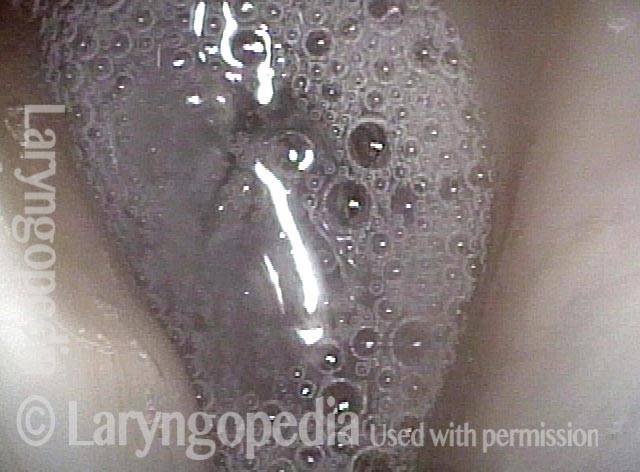
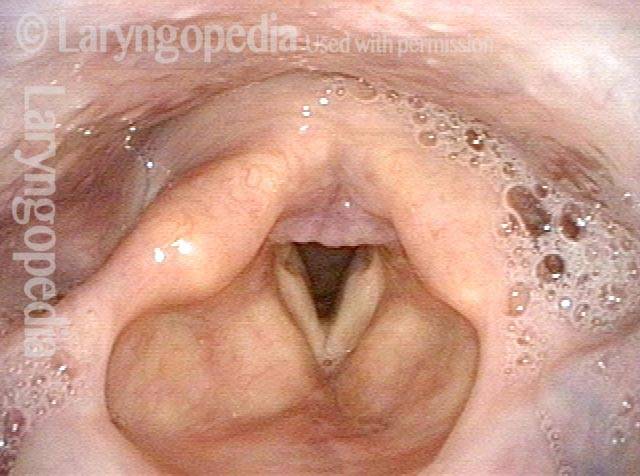
Dilation for post-radiation hypopharyngeal stenosis (1 of 4)
Dilation for post-radiation hypopharyngeal stenosis (1 of 4)
Dilation for post-radiation hypopharyngeal stenosis (2 of 4)
Dilation for post-radiation hypopharyngeal stenosis (2 of 4)
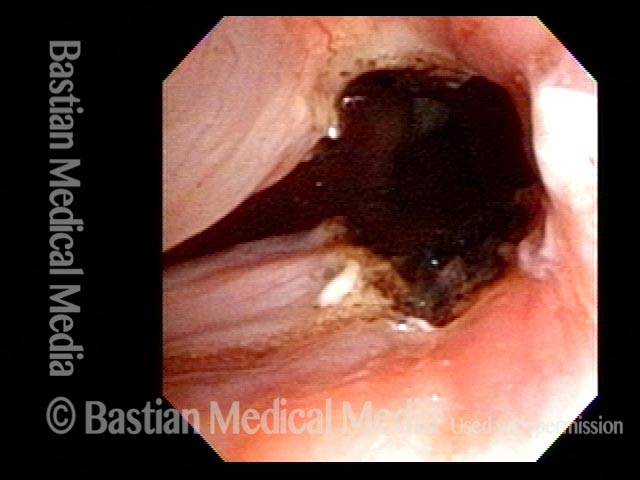
Dilation for post-radiation hypopharyngeal stenosis (3 of 4)
Dilation for post-radiation hypopharyngeal stenosis (3 of 4)
Dilation for post-radiation hypopharyngeal stenosis (4 of 4)
Dilation for post-radiation hypopharyngeal stenosis (4 of 4)
Tracheal Deformity and Stenosis, before and after Repair
Upper tracheal stenosis, before repair (1 of 6)
Upper tracheal stenosis, before repair (1 of 6)
Upper tracheal stenosis, before repair (2 of 6)
Upper tracheal stenosis, before repair (2 of 6)
Looking from below the stenosis (3 of 6)
Looking from below the stenosis (3 of 6)
After tracheal repair (4 of 6)
After tracheal repair (4 of 6)
After tracheal repair (5 of 6)
After tracheal repair (5 of 6)
After tracheal repair (6 of 6)
After tracheal repair (6 of 6)
Post-Intubation Stenosis
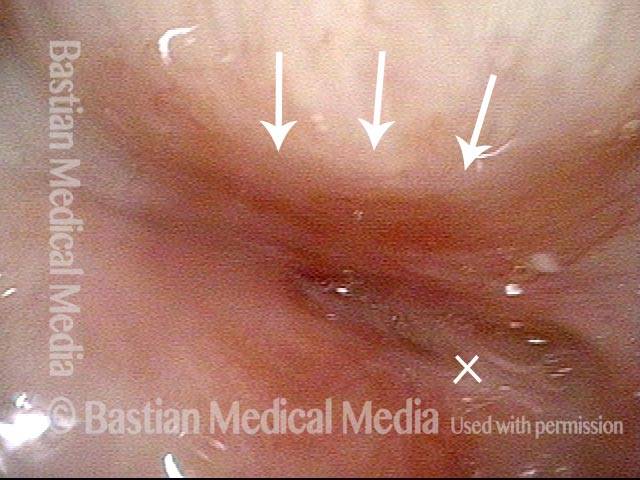
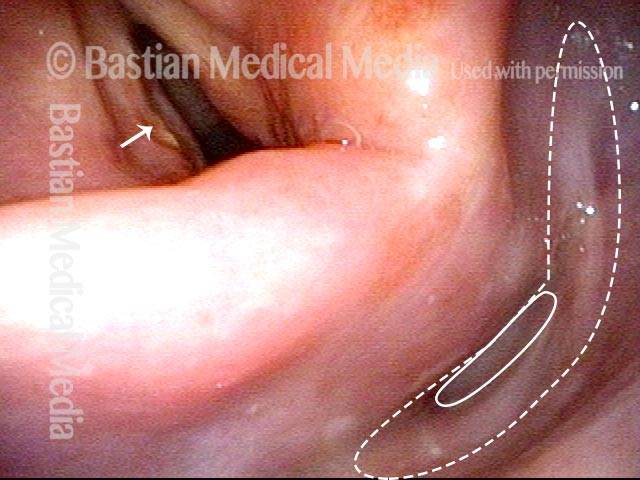
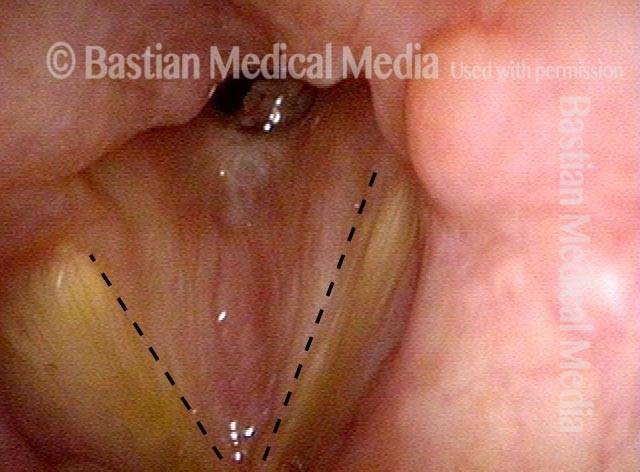
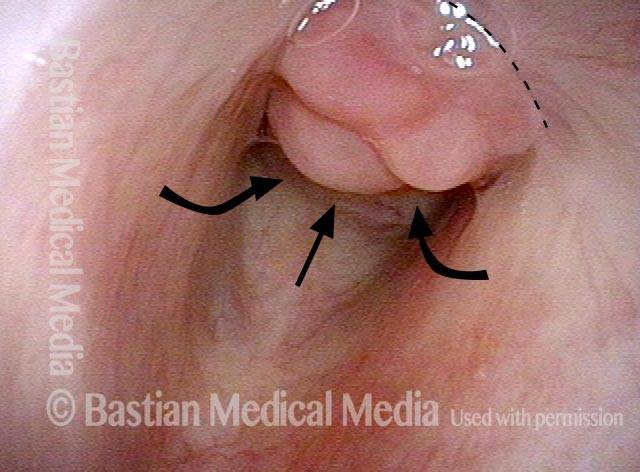
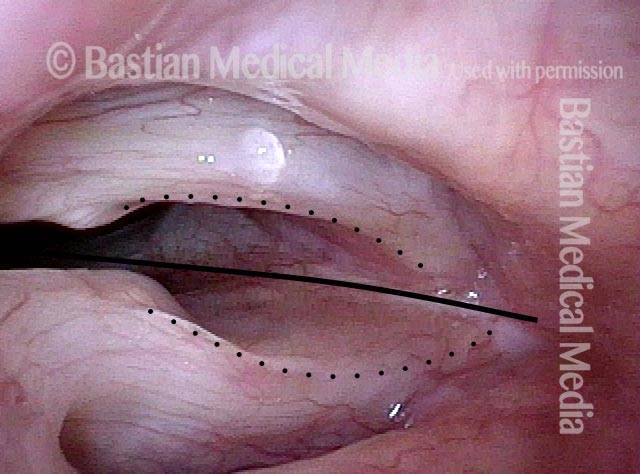
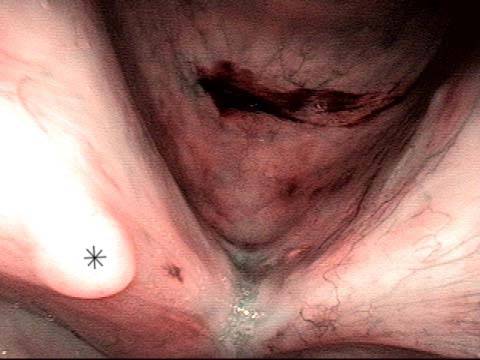
Endotrachel tube injury (1 of 4)
Endotrachel tube injury (1 of 4)
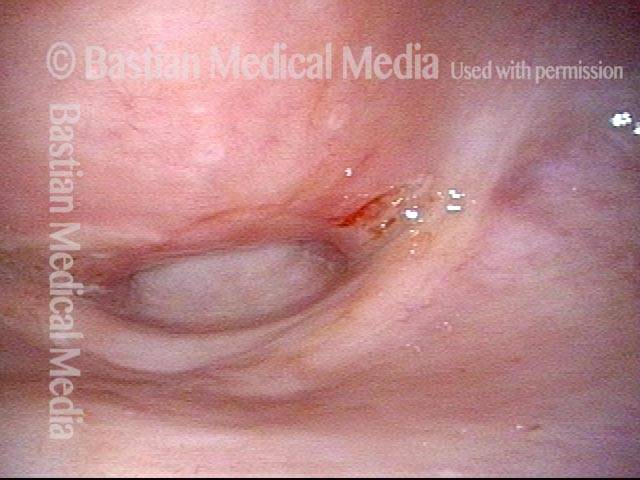
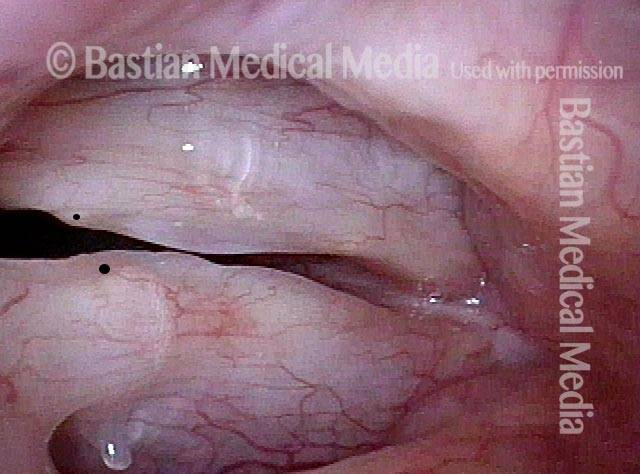
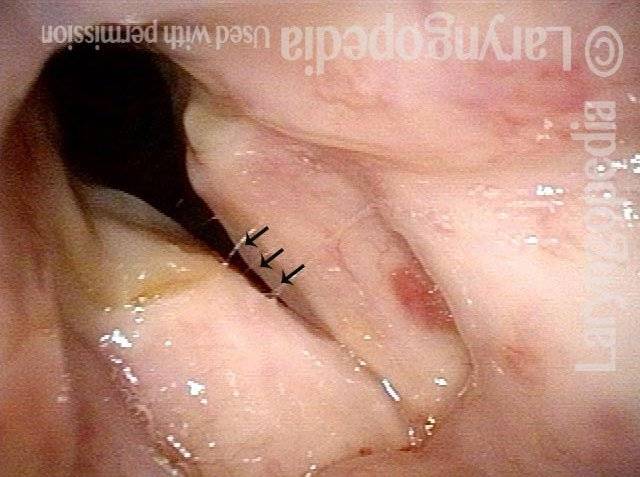
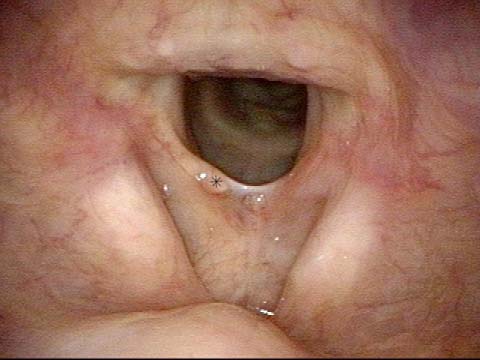
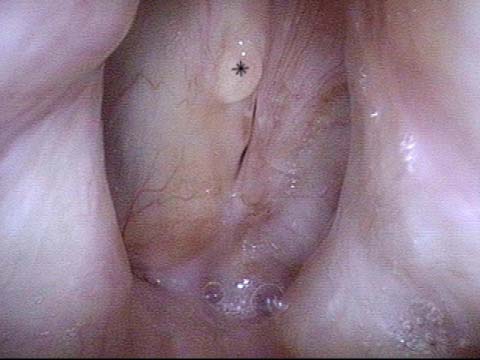
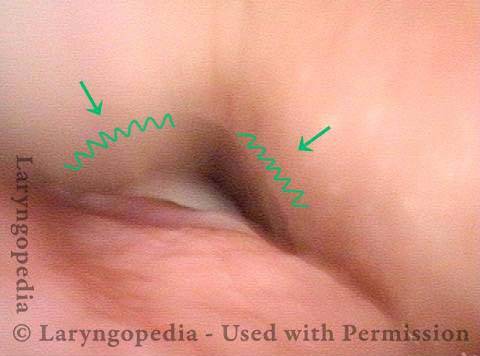
Closer view, between the posterior vocal cords (2 of 4)
Closer view, between the posterior vocal cords (2 of 4)
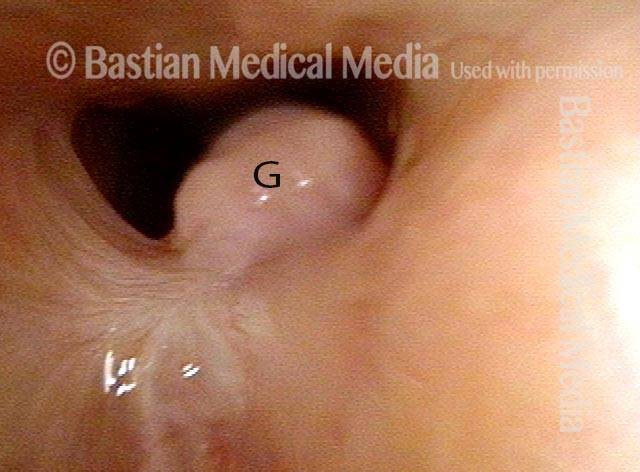
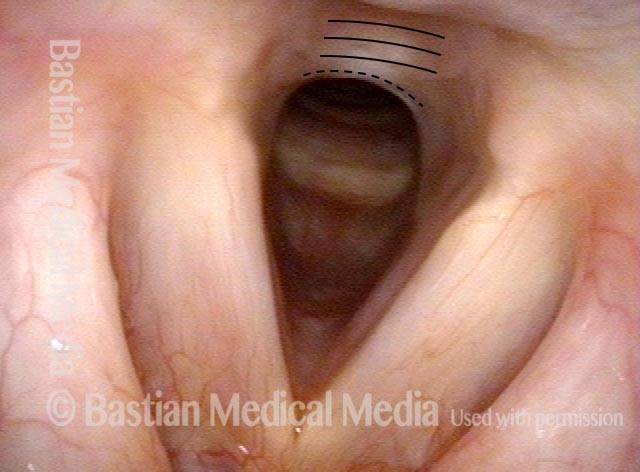
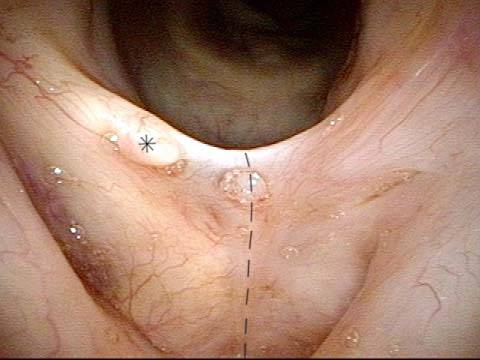
Even closer view, showing upper surface of the tube (3 of 4)
Even closer view, showing upper surface of the tube (3 of 4)
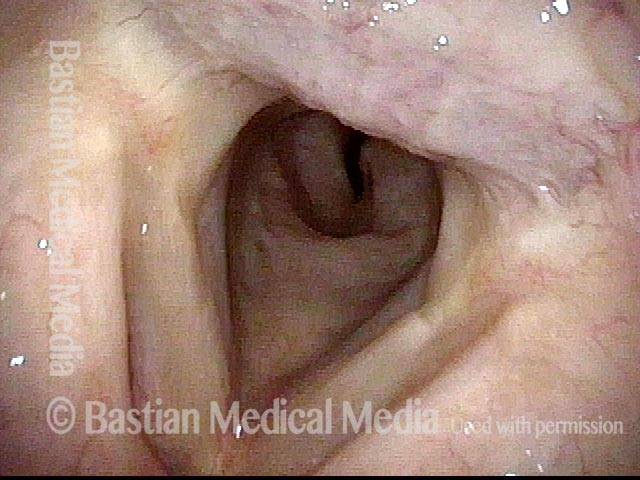
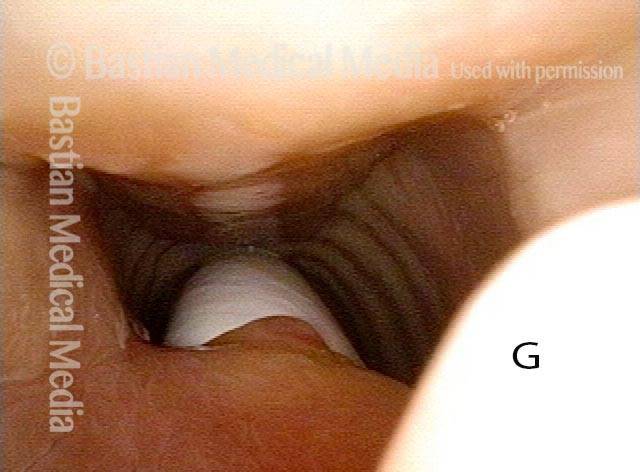
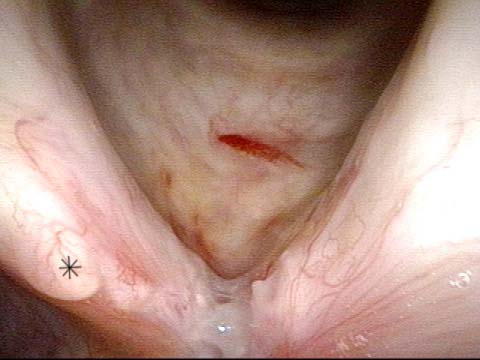
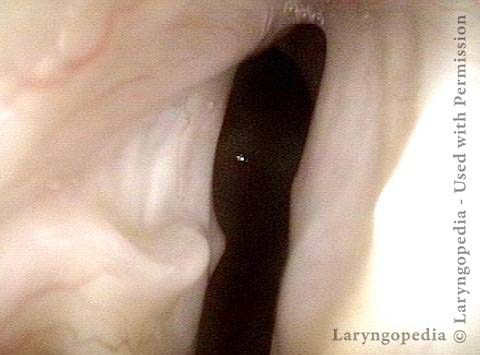
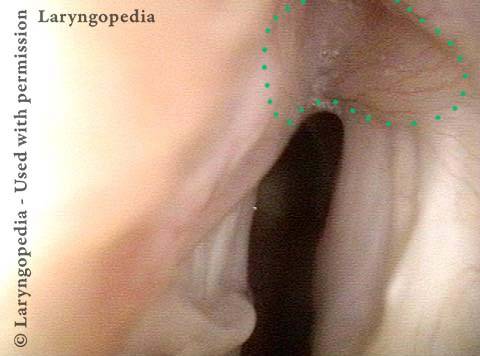
Non-inflammatory stenosis, caused purely by injury (4 of 4)
Non-inflammatory stenosis, caused purely by injury (4 of 4)
Sickle Cell Disease and Laryngeal Stenosis
Sickle cell disease and subglottic swelling (1 of 4)
Sickle cell disease and subglottic swelling (1 of 4)
At closer range (2 of 4)
At closer range (2 of 4)
Maturing granuloma (3 of 4)
Maturing granuloma (3 of 4)
High-grade stenosis ( 4 of 4)
High-grade stenosis ( 4 of 4)
Subglottic Granulation and Curving Airstream
Intubation injury (1 of 4)
Intubation injury (1 of 4)
Lobules (2 of 4)
Lobules (2 of 4)
2 months later (3 of 4)
2 months later (3 of 4)
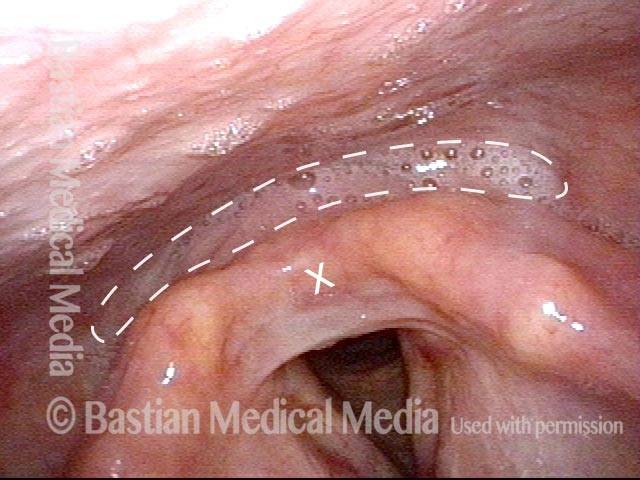
Scar band (4 of 4)
Scar band (4 of 4)
Office-Based Surgery When General Anesthesia Is too Risky
Involuntary inspiratory voice (1 of 6)
Involuntary inspiratory voice (1 of 6)
Laser posterior commissuroplasty (2 of 6)
Laser posterior commissuroplasty (2 of 6)
During the commissuroplasty (3 of 6)
During the commissuroplasty (3 of 6)
Deepening divot (4 of 6)
Deepening divot (4 of 6)
Inspiratory indrawing decreased (5 of 6)
Inspiratory indrawing decreased (5 of 6)
Phonation (6 of 6)
Phonation (6 of 6)
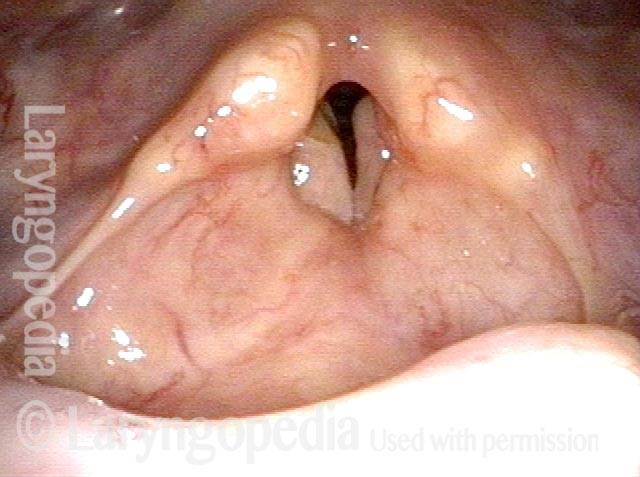
The Adult Result of Infant Cricoid Split
Cricoid split procedure (1 of 6)
Cricoid split procedure (1 of 6)
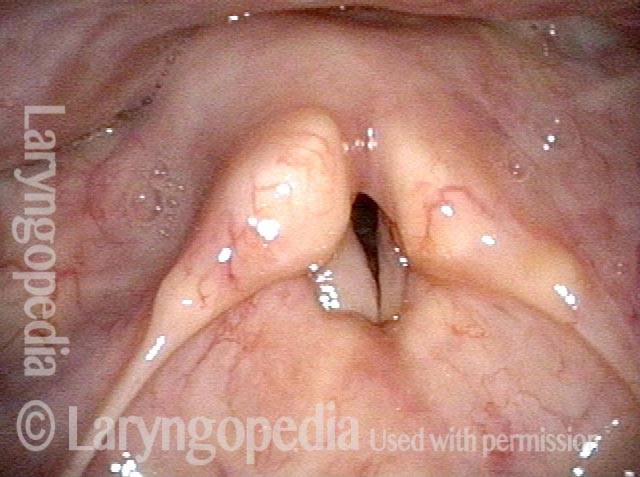
Rotated view (2 of 6)
Rotated view (2 of 6)
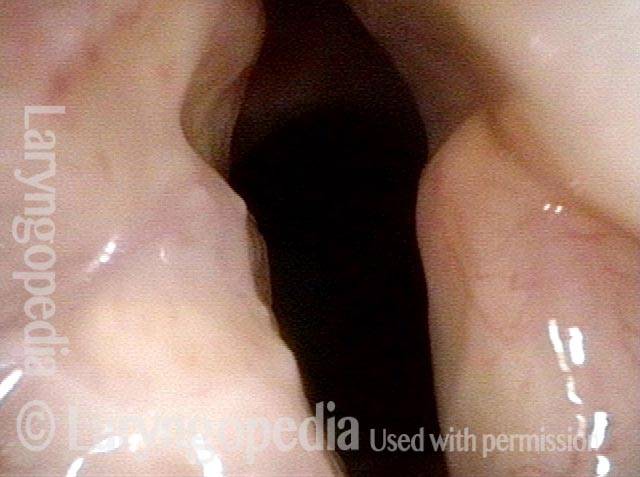
Open phase (3 of 6)
Open phase (3 of 6)
Cricoarytenoid joints (4 of 6)
Cricoarytenoid joints (4 of 6)
Lateral excursion (5 of 6)
Lateral excursion (5 of 6)
Closed phase (6 of 6)
Closed phase (6 of 6)
A Fenestrated Trach Tube Allows Voicing when there Is Stenosis
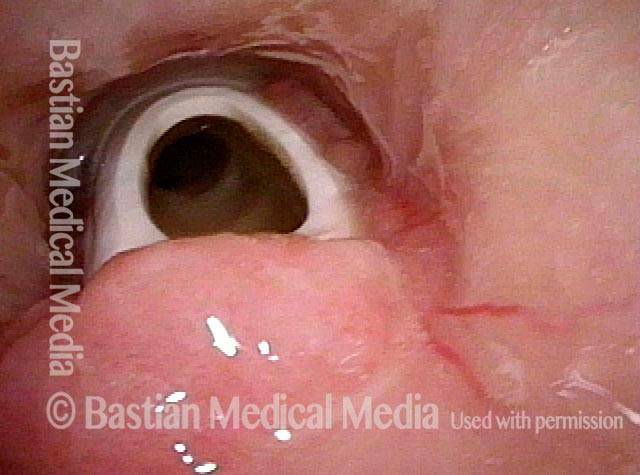
Tracheotomy (1 of 4)
Tracheotomy (1 of 4)
View below vocal cords (2 of 4)
View below vocal cords (2 of 4)
Fenestra (3 of 4)
Fenestra (3 of 4)
Patient post-trach (4 of 4)
Patient post-trach (4 of 4)
Stenosis of Larynx and Trachea before and after Cricotracheal Resection and Reanastomosis
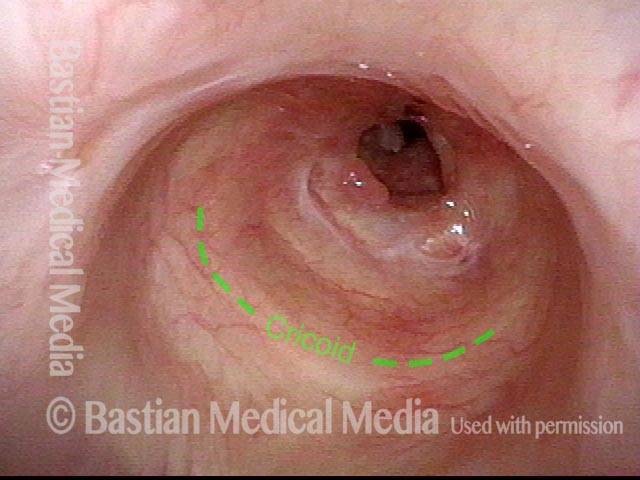
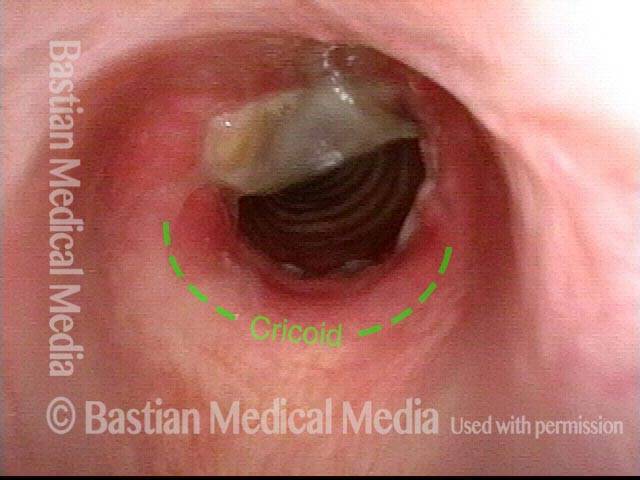
Post intubation and tracheotomy (1 of 8)
Post intubation and tracheotomy (1 of 8)
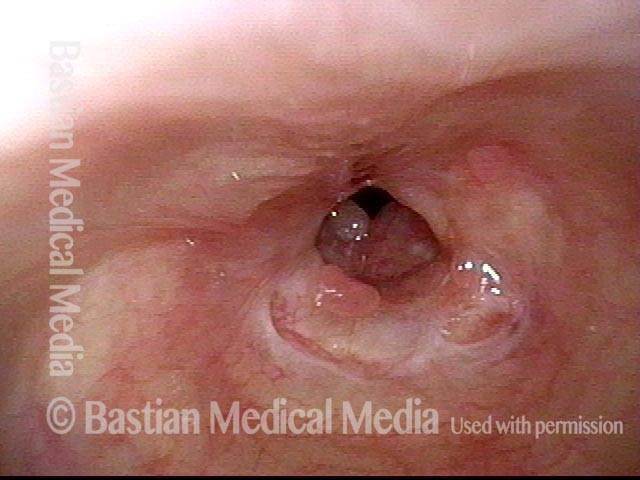
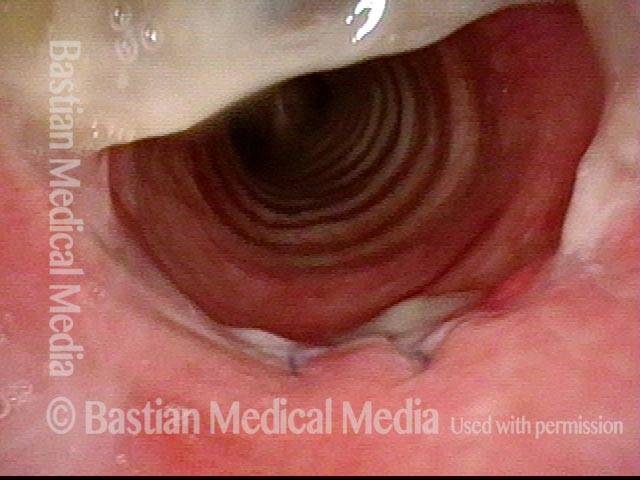
Confirmed stenosis (2 of 8)
Confirmed stenosis (2 of 8)
Tracheotomy tract (3 of 8)
Tracheotomy tract (3 of 8)
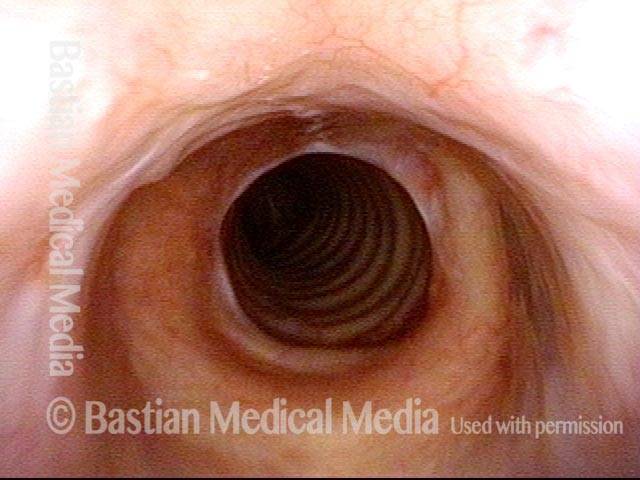
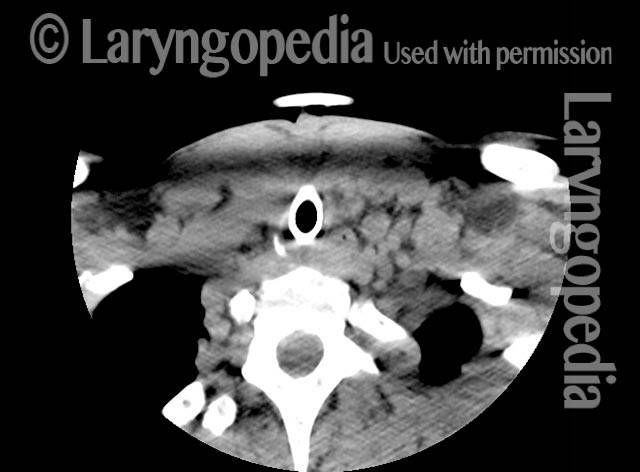
Cricoid cartilage (4 of 8)
Cricoid cartilage (4 of 8)
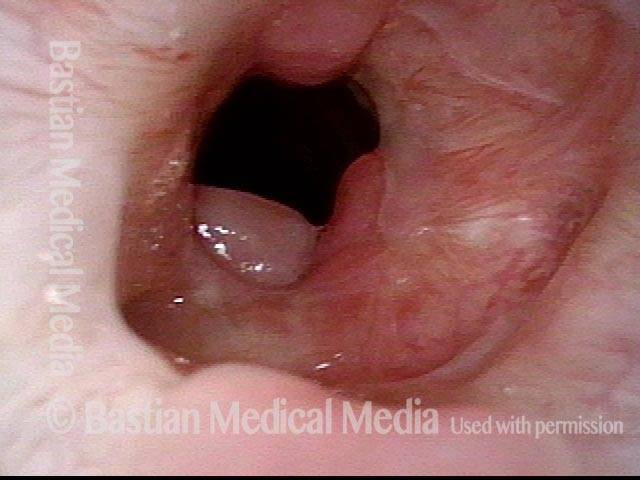
Resection needed (5 of 8)
Resection needed (5 of 8)
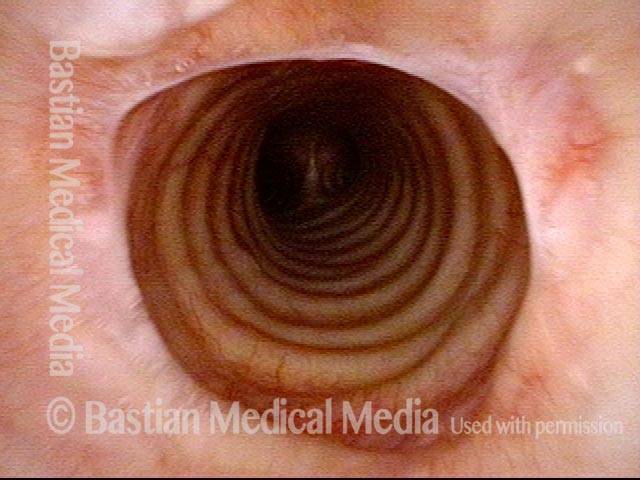
Post surgery (6 of 8)
Post surgery (6 of 8)
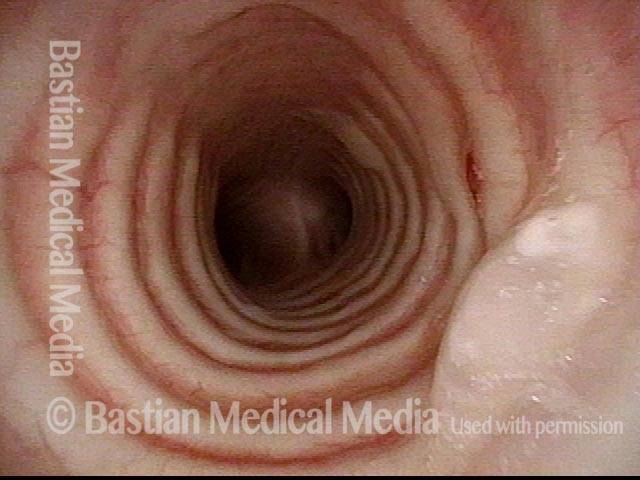
Trach removed (7 of 8)
Trach removed (7 of 8)
Patient’s sentiment (8 of 8)
Patient’s sentiment (8 of 8)
Stenosis Before and After Dilation for Forme Fruste Wegener’s
Subglottic stenosis (1 of 5)
Subglottic stenosis (1 of 5)
Inflammation (2 of 5)
Inflammation (2 of 5)
Flexible scope (3 of 5)
Flexible scope (3 of 5)
Post-dilation (4 of 5)
Post-dilation (4 of 5)
Post-operative bruising (5 of 5)
Post-operative bruising (5 of 5)
Sometimes “low-tech” Is Best for Stenosis
Esophageal bougie (1 of 4)
Esophageal bougie (1 of 4)
Swallowing crescent (2 of 4)
Swallowing crescent (2 of 4)
Post-arytenoid area (3 of 4)
Post-arytenoid area (3 of 4)
Maximum diameter (4 of 4)
Maximum diameter (4 of 4)
Who knew…? Many Such Injuries Are Never Found
Coughing evaluation (1 of 6)
Coughing evaluation (1 of 6)
Intubation scars (2 of 6)
Intubation scars (2 of 6)
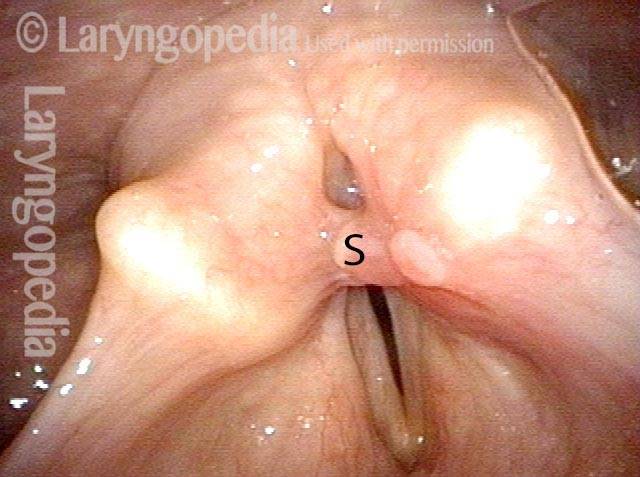
Stenosis (3 of 6)
Stenosis (3 of 6)
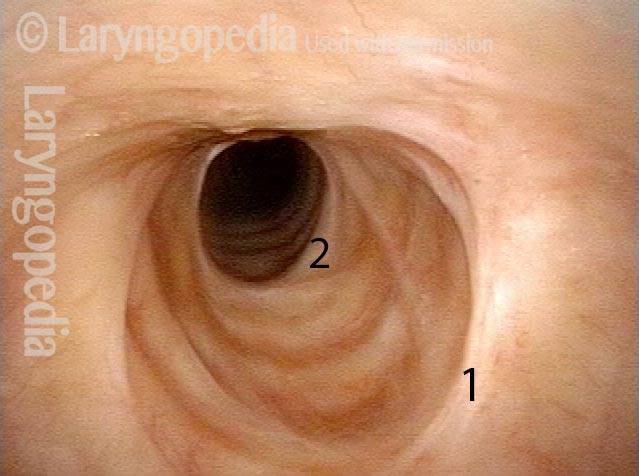
Further down trachea (4 of 6)
Further down trachea (4 of 6)
Below stenosis (5 of 6)
Below stenosis (5 of 6)
Carina (6 of 6)
Carina (6 of 6)
Stenosis at Two Levels: Supraglottic and Glottic
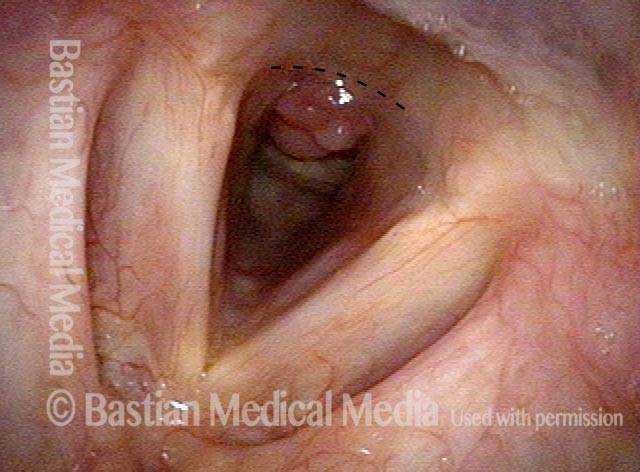
Laryngeal stenosis post intubation (1 of 7)
Laryngeal stenosis post intubation (1 of 7)
Closer range (2 of 7)
Closer range (2 of 7)
Posterior commissure (3 of 7)
Posterior commissure (3 of 7)
View into trachea (4 of 7)
View into trachea (4 of 7)
Post laser release (5 of 7)
Post laser release (5 of 7)
Scarring (6 of 7)
Scarring (6 of 7)
Closer view (7 of 7)
Closer view (7 of 7)
Progressive Radiation Fibrosis Effects on the Larynx and a Solution to some of it
Forty years post-radiation (1 of 8)
Forty years post-radiation (1 of 8)
Involuntary inspiratory voice (2 of 8)
Involuntary inspiratory voice (2 of 8)
Only capable of high pitch (3 of 8)
Only capable of high pitch (3 of 8)
Open phase vibration (4 of 8)
Open phase vibration (4 of 8)
One week post-commissuroplasty (5 of 8)
One week post-commissuroplasty (5 of 8)
Rapid inhalation, closer view (6 of 8)
Rapid inhalation, closer view (6 of 8)
Three months post-surgery (7 of 8)
Three months post-surgery (7 of 8)
Closer view, post-surgery (8 of 8)
Closer view, post-surgery (8 of 8)
Tracheal Red Herring; the Real Culprit is Cricopharyngeus Spasm
Tracheal stenosis? (1 of 4)
Tracheal stenosis? (1 of 4)
Narrowing at trachea (2 of 4)
Narrowing at trachea (2 of 4)
Closer view (3 of 4)
Closer view (3 of 4)
No significant change in breathing (4 of 4)
No significant change in breathing (4 of 4)
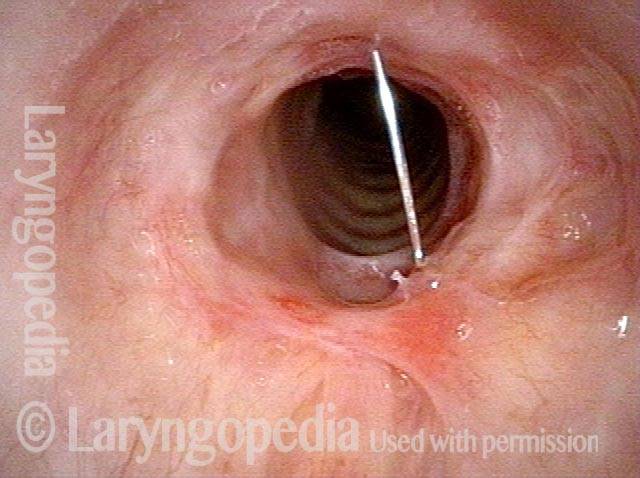
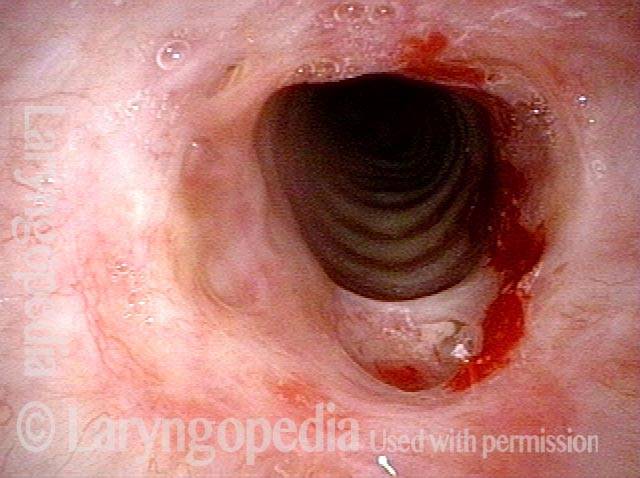
A Different Approach to Inflammatory Tracheal Stenosis
Planning on periodical injections (1 of 4)
Planning on periodical injections (1 of 4)
Long-acting steroid (2 of 4)
Long-acting steroid (2 of 4)
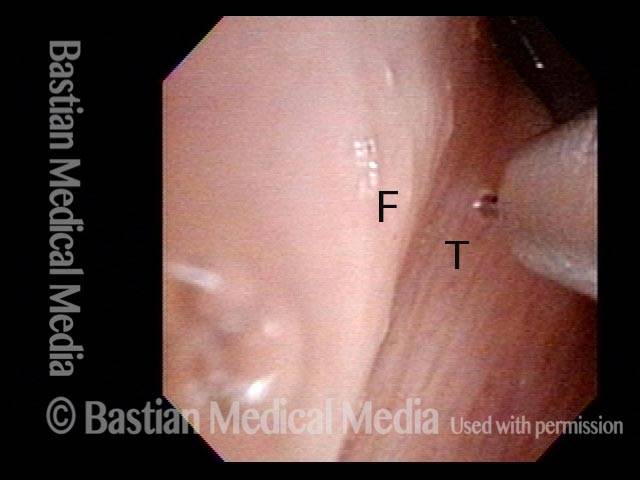
Needle going into the posterior of stenosis (3 of 4)
Needle going into the posterior of stenosis (3 of 4)
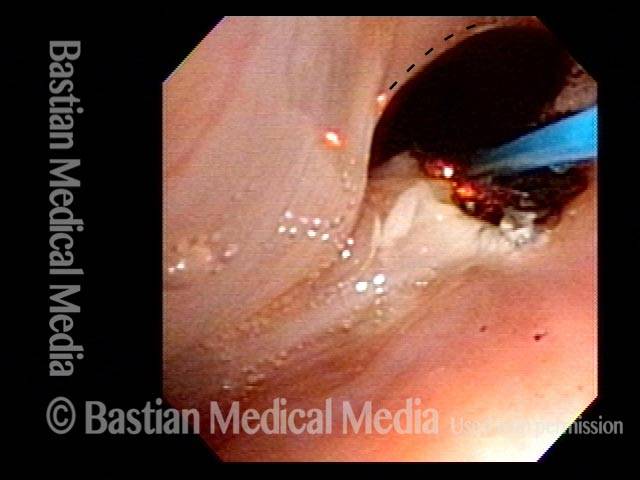
Posterior tracheal wall (4 of 4)
Posterior tracheal wall (4 of 4)
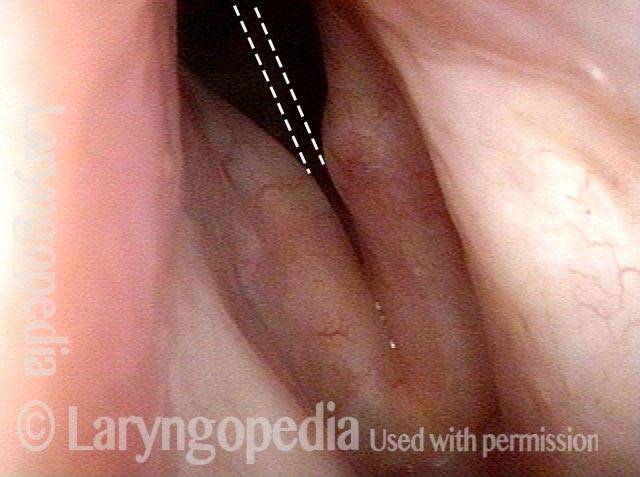
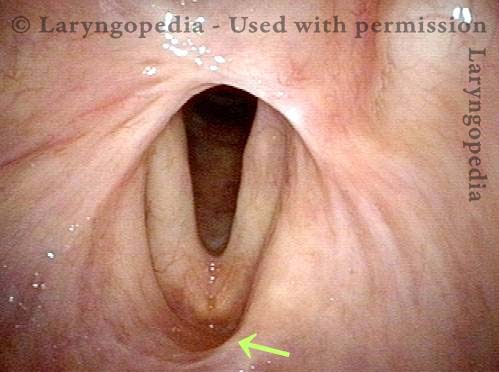
Motivated Airway Examination Avoids Further Surgery
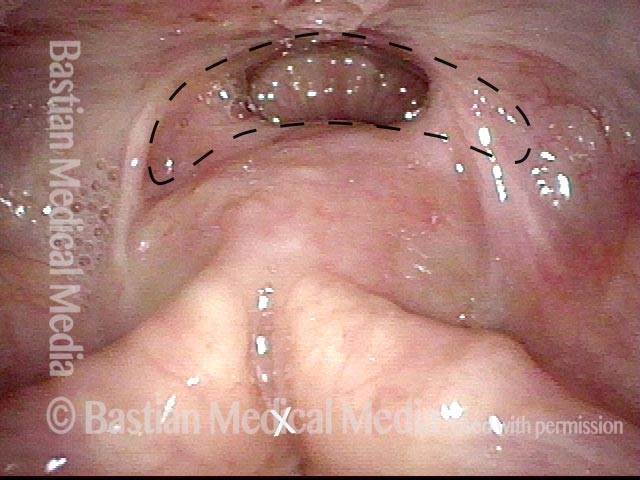
Marginal airway (1 of 4)
Marginal airway (1 of 4)
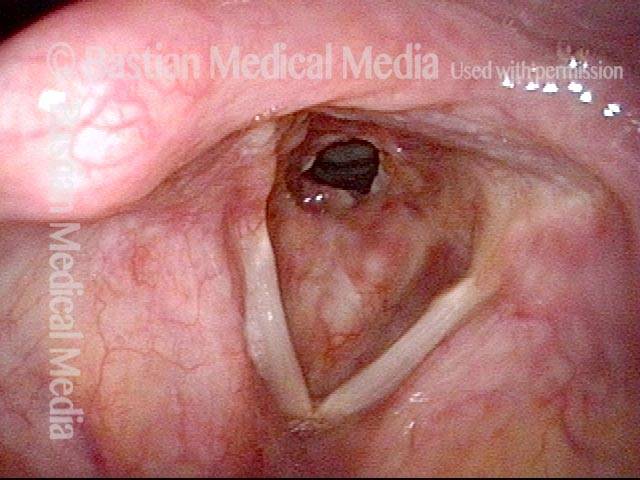
Airway at close range (2 of 4)
Airway at close range (2 of 4)
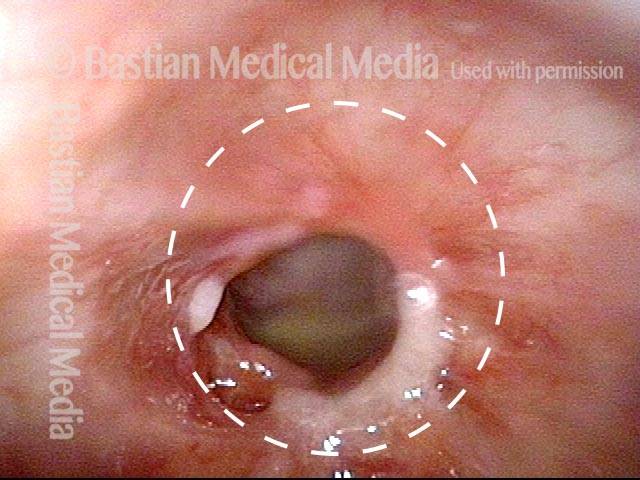
Forced inspiration (3 of 4)
Forced inspiration (3 of 4)
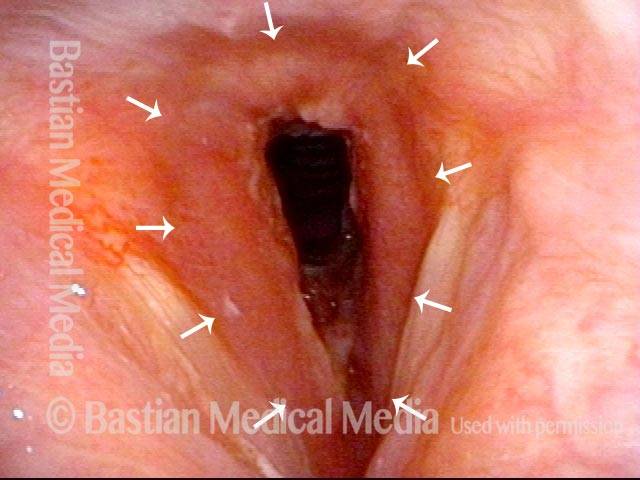
Alternative to tracheotomy (4 of 4)
Alternative to tracheotomy (4 of 4)
Supraglottic (above the vocal cord) scarring as a result of radiotherapy
Supraglottic Scarring (1 of 4)
Supraglottic Scarring (1 of 4)
Hoarseness caused by radiation effects (2 of 4)
Hoarseness caused by radiation effects (2 of 4)
Cords don’t close completely (3 of 4)
Cords don’t close completely (3 of 4)
Normal caliber trachea (4 of 4)
Normal caliber trachea (4 of 4)
Glottic Web Management Without A Keel
Glottic Web (1 of 7)
Glottic Web (1 of 7)
Glottic Web (2 of 7)
Glottic Web (2 of 7)
Glottic Web (3 of 7)
Glottic Web (3 of 7)
Glottic Web (4 of 7)
Glottic Web (4 of 7)
Re-grown mucosa (5 of 7)
Re-grown mucosa (5 of 7)
Closed phase of vibration (6 of 7)
Closed phase of vibration (6 of 7)
Restoration of oscillatory ability (7 of 7)
Restoration of oscillatory ability (7 of 7)
Nuances of Endotracheal Tube Injury
This woman with high-risk comorbidities of diabetes and obesity, was in ventilated in ICU more than a month for pulmonary complications of Covid-19 infection. She had an orotracheal tube in place for 3.5 weeks, and then a tracheotomy tube was placed. Now at her first visit a year later, she remains tracheotomy-dependent, and is told she has bilateral vocal cord paralysis (disproven in the following photo series).
Maximum glottic opening (1 of 8)
Maximum glottic opening (1 of 8)
Undersurface mucosa indraws (2 of 8)
Undersurface mucosa indraws (2 of 8)
Phonation (3 of 8)
Phonation (3 of 8)
Posterior commissure divot (4 of 8)
Posterior commissure divot (4 of 8)
Further evidence of scarring (5 of 8)
Further evidence of scarring (5 of 8)
View into trachea (6 of 8)
View into trachea (6 of 8)
Vibration of trachea (7 of 8)
Vibration of trachea (7 of 8)
Open trachea beyond the tube (8 of 8)
Open trachea beyond the tube (8 of 8)
The plan here is posterior commissuroplasty, followed by placement of a smaller trach tube and a trial of plugging. If plugging is tolerated during the day, she will need a sleep study with it plugged at night, given the tracheomalacia and her obesity.
Breathing Tube Injury, not Vocal Cord Paralysis
This middle-aged woman was injured severely in an auto accident as a teenager. Recovery involved a long stay in ICU, and ventilation via a breathing (endotracheal) tube for a few weeks prior to tracheotomy.
Fifteen years earlier, a posterior commissuroplasty was done by me on the left side. Severely short of breath before that procedure, she said the improvement was such that she was able to do most activities of daily living remarkably well for many years.
While still much better than prior to the posterior commissuroplasty, she has felt a little more limited in the past few years and wants now another similar airway-widening procedure. Speaking voice can easily pass for normal, though she thinks it is occasionally a little rough.
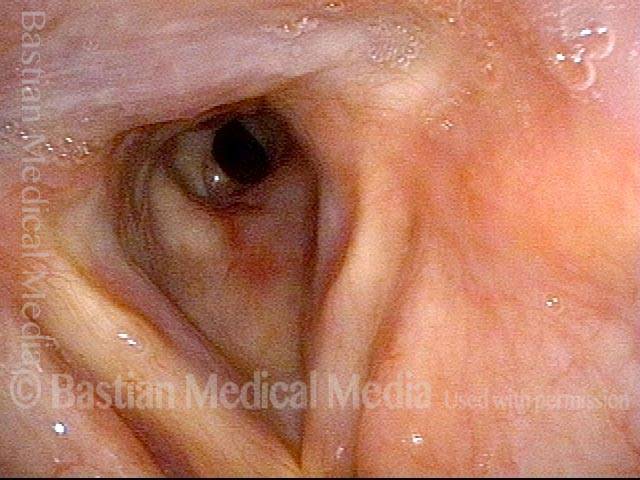
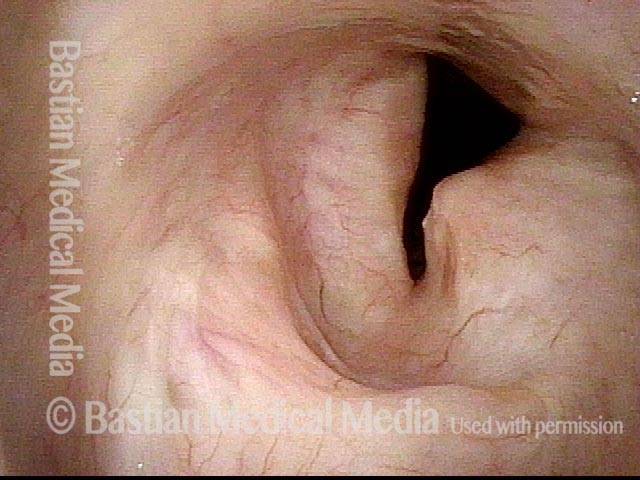
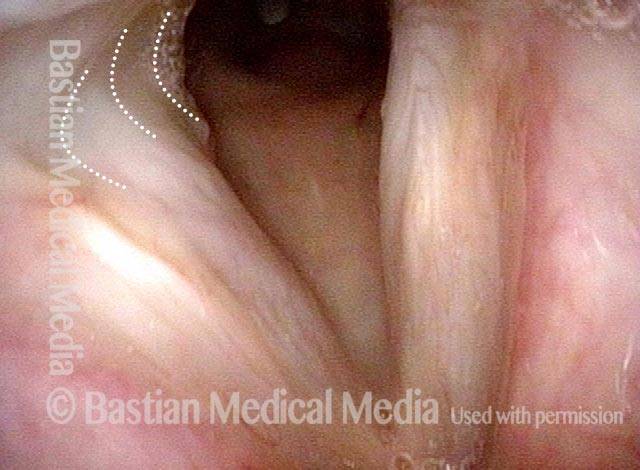
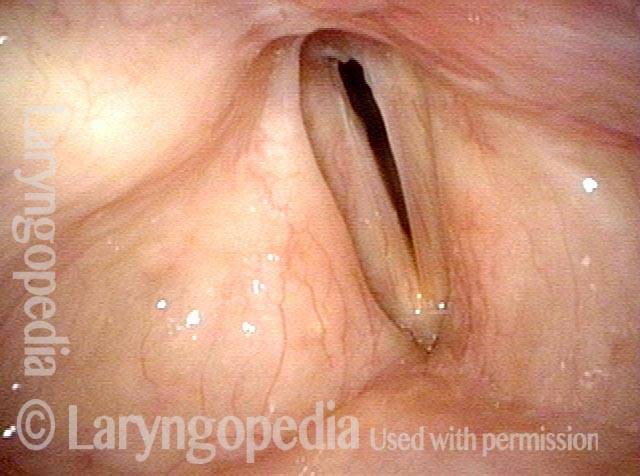
Aperture is very narrow (1 of 6)
Aperture is very narrow (1 of 6)
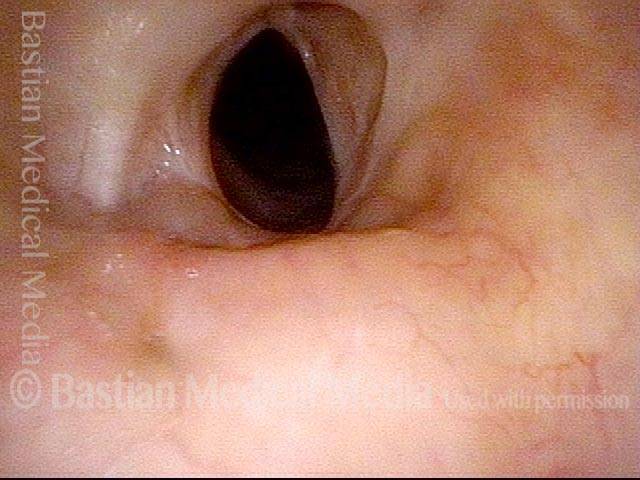
Involuntary inspiratory phonation (2 of 6)
Involuntary inspiratory phonation (2 of 6)
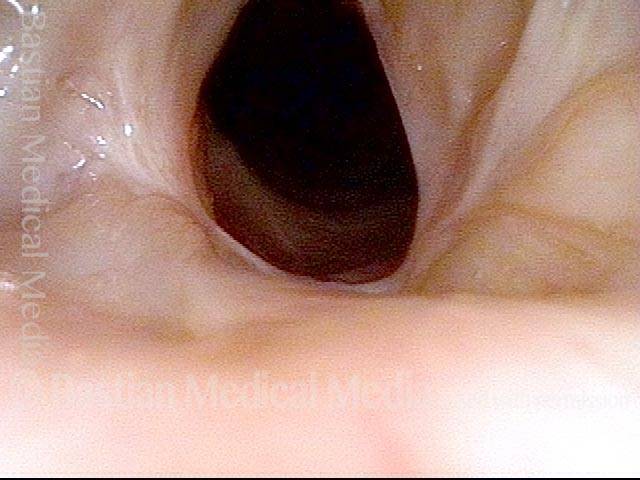
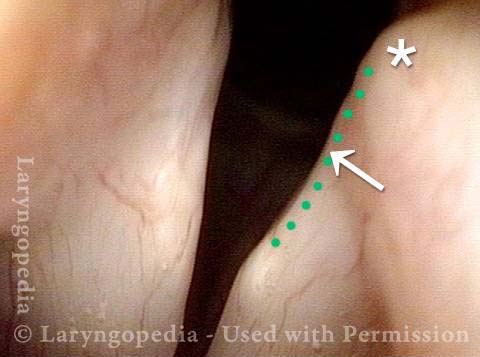
Divot on left vocal cord (3 of 6)
Divot on left vocal cord (3 of 6)
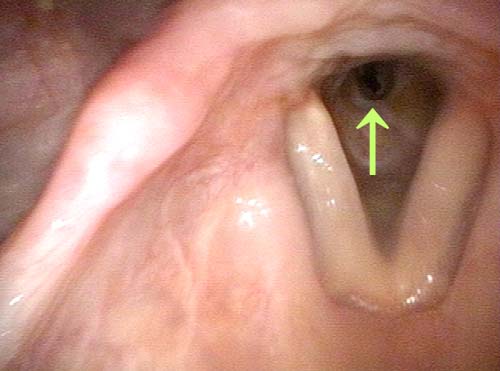
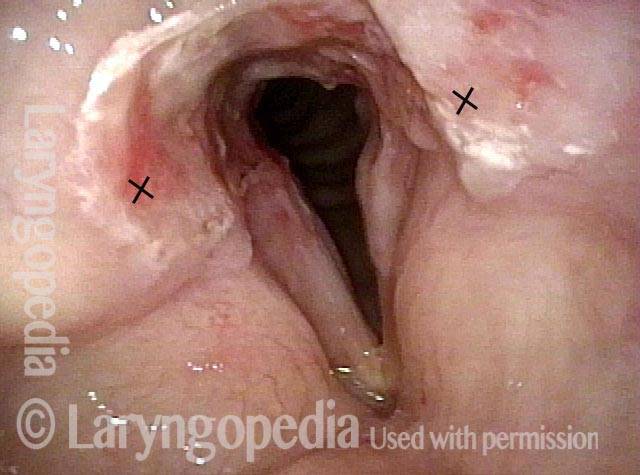
Endotracheal tube injury (4 of 6)
Endotracheal tube injury (4 of 6)
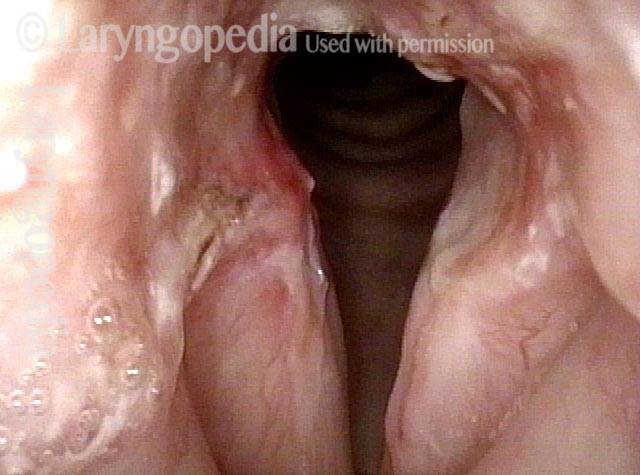
Laser cookie bite (5 of 6)
Laser cookie bite (5 of 6)
Surface scarring in the tracheotomy (6 of 6)
Surface scarring in the tracheotomy (6 of 6)
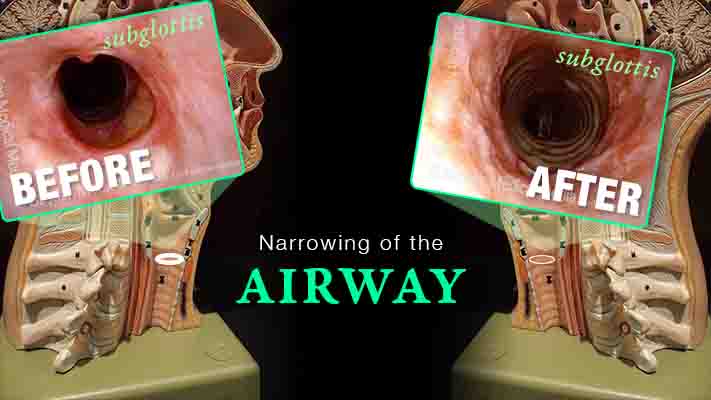
Inflammation Subglottic Stenosis – Definition, Symptoms, and Treatments
Are you experiencing gradual onset of noisy, even effortful breathing? One uncommon but important explanation is idiopathic, inflammatory subglottic stenosis. That just means “unknown cause, likely autoimmune narrowing just below the vocal cords and at the highest part of the windpipe.”
This video explains the disorder and its management, shows “before” and “after” photos, and reassures viewers that if yours is the usual case, there doesn’t seem to be any effect on general health or lifespan.
Tracheal Stenosis: Before and After
In this video, trachea (windpipe) blockage causes shortness of breath until the narrowed segment is removed. You will see views of the trachea before and after surgical repair.
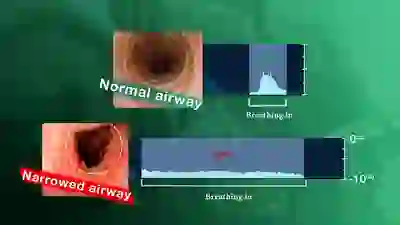
Using Your EARS to Understand Airway Narrowing
A narrowing anywhere in the breathing “pipe” that leads to the lungs causes shortness of breath, typically with harsh inspiratory noise on exertion. Such a narrowing can follow injury, intubation, cancer treatment, auto-immune disorders, etc.
It is possible to gain an immediate understanding of the magnitude of the airway narrowing within minutes by using a simple test “graded” with one’s ears. The severity of the problem can be understood before any examination or X-ray evaluation. Dr. Bastian explains…
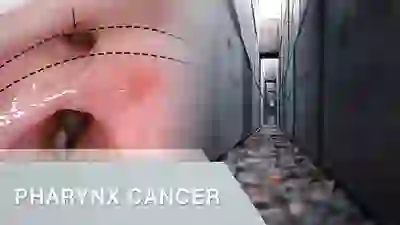
Post-Radiation Hypopharyngeal Stenosis
People with larynx or pharynx (voice box or throat) cancer often undergo radiation therapy as part of their treatment regimen. An uncommon complication is stenosis (narrowing, scarring) of the entrance to the upper esophagus at the junction of the throat and esophagus. This video provides an example of this disorder.